How This Recommendation Was Created
Our international panel included patient partners , general practitioners, general internists, urologists, epidemiologists, methodologists, and statisticians. They determined the scope of the question that the recommendation should address and what outcomes are most important to patients considering screening.
No person had financial conflicts of interest intellectual and professional conflicts were minimised and managed .
The panel identified eight critical outcomes needed to inform the recommendations: all-cause mortality prostate cancer mortality incidence of prostate cancer diagnoses incidence of localised cancer incidence of advanced cancer complications from biopsies , complications from prostate cancer treatment and quality of life. The panel also identified three additional patient-important outcomes: false positive rates false negative rates , and the anxiety and uncertainty related to concerns about having prostate cancer. The panel asked that potential subgroups effects be explored according to age, screening interval, family history, being of African descent, and being of lower socioeconomic level. They also asked for a sensitivity analysis of the effect of screening restricted to trials at lower risk of bias.
To inform the recommendation, the panel members requested two systematic reviews, on the following questions:
Two parallel teams conducted these systematic reviews, which are linked to this publication.
What Is Involved In A Prostate Cancer Screening
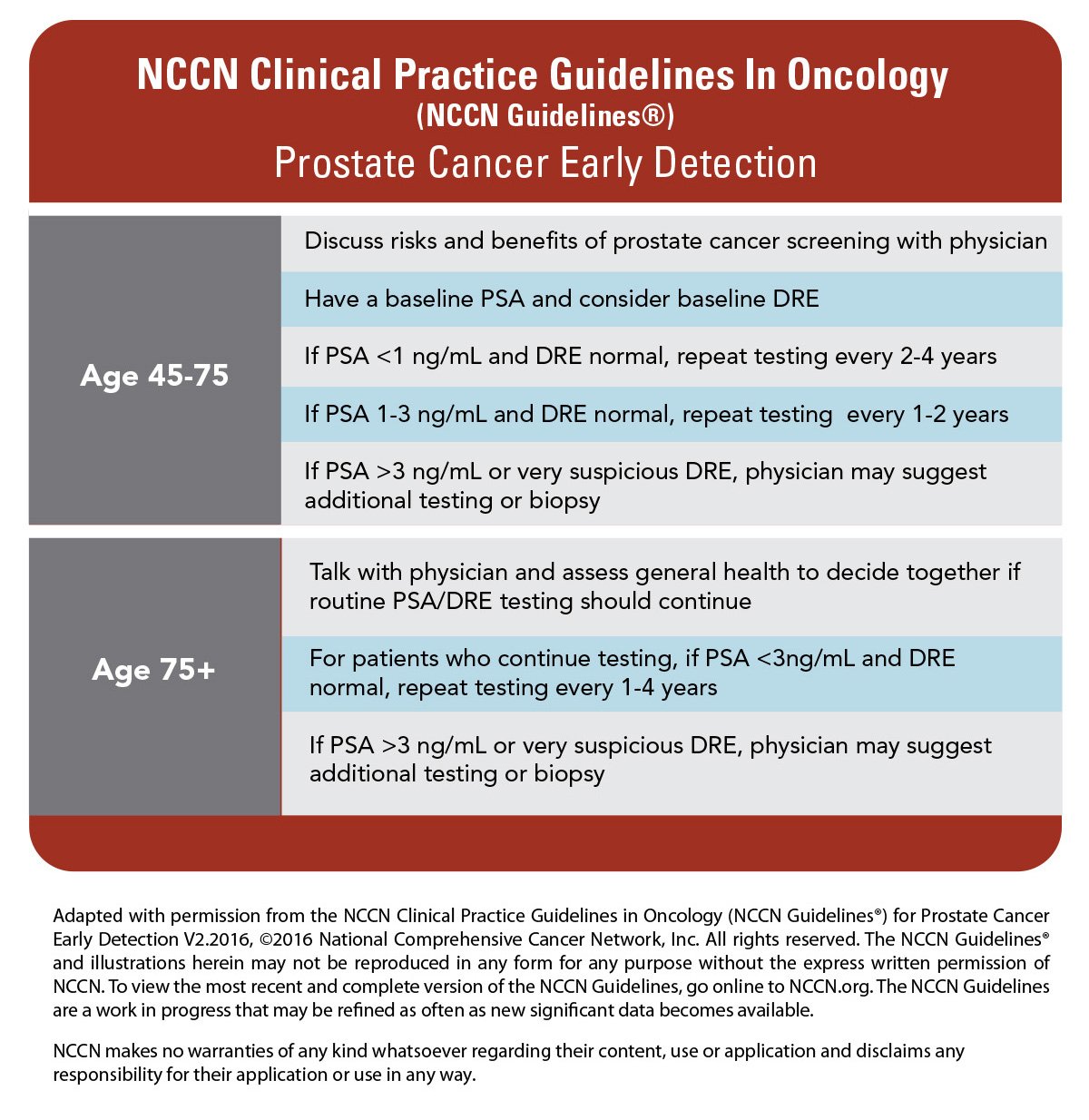
- The PSA blood test: Several factors can influence PSA levels found in a blood test. Evidence-based guidelines are updated frequently and help to identify those who are the best candidates for a blood screening. Men should talk with their physician about PSA results and appropriate course of action.
- The digital rectal exam: While the idea of a DRE is daunting to many men, it is actually very simple, quick and results in little to no discomfort. This exam can help physicians feel for irregularities or hard areas that could indicate cancer.
Nursing Allied Health And Interprofessional Team Monitoring
One of the major concerns regarding prostate cancer screening is overdiagnosis, which involves overtreatment of low-grade prostate cancer and decreasing the quality of life of the patient by adding treatment-associated side effects and psychological harm when in reality, cancer would not have caused any clinical problems in the patient. This outcome can be overcome by active surveillance . Active surveillance is one of the management strategies in which a super select group of low-grade cancer patients are under close monitoring and followed through their disease course with the expectation to intervene only if cancer progresses. This approach will lead to the avoidance of treatment-associated side effects in such patients. This monitoring is only achievable by cumulative efforts and coordination of care amongst the interdisciplinary team members.
Don’t Miss: Why Do You Get Prostate Cancer
Benefits And Risks Of Prostate Cancer Screening
Most any medical decision comes with benefits and potential risks, and prostate cancer screening is no exception. Prostate cancer may spread to other parts of the body, which may make it more difficult to treat. The benefits of prostate cancer screening include:
- Early diagnosis while the cancer is still small and localized
- The ability to make informed treatment decisions
- The ability to start treatment before the prostate cancer has the chance to spread
Some potential risk factors for prostate cancer screening and subsequent treatment include:
- False positives: A PSA result may be abnormal even though cancer isnt present, which may lead to:
- Emotional distress
- An unnecessary prostate biopsy, which may cause side effects, including infection, discomfort and bleeding
The doctor can explain how these benefits and harms may apply to the patients health and well-being.
New Prostate Cancer Screening Guidelines Released
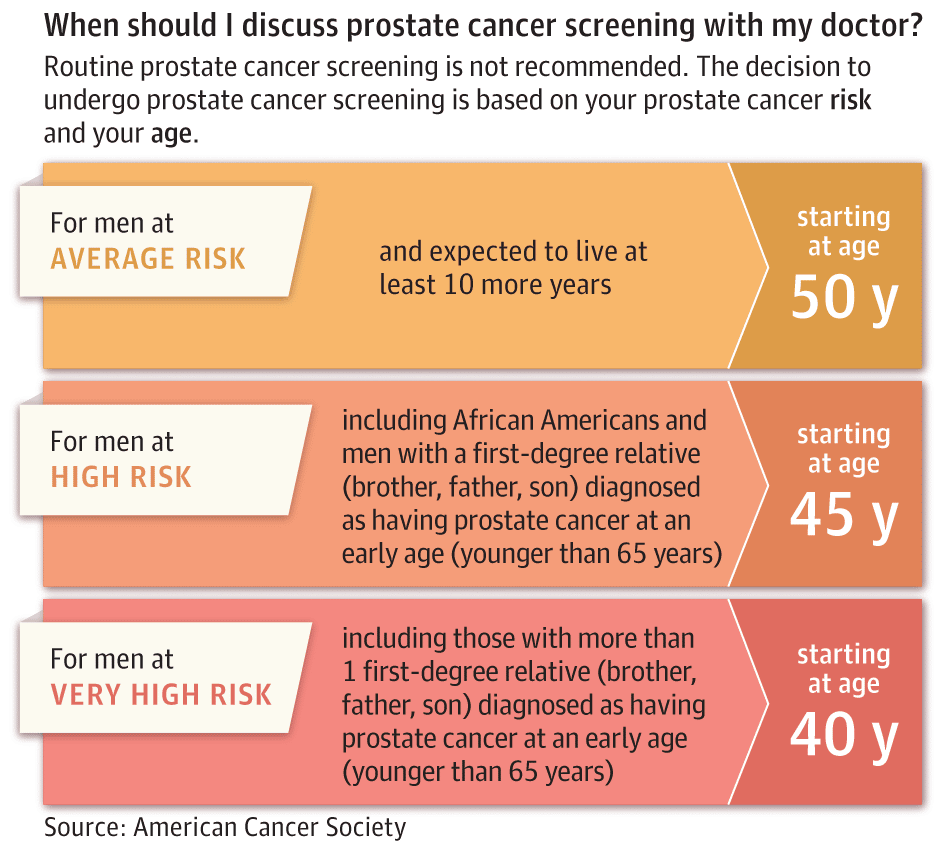
Prostate cancer is the second most common cancer among men, and one in seven men will be diagnosed with it during his lifetime. Screening, or early detection in men without symptoms, can identify men who are at risk for problems related to prostate cancer and may benefit from additional testing. PSA remains the primary screening tool, which is a blood test that measures the level of a specific protein produced by cells of the prostate gland. But many considerations come into play on whether a man should have PSA screening at all.
Explains Dr. Elias Hyams, a urologist with ColumbiaDoctors, the faculty practice of Columbia University Irving Medical Center. Urologists interpret PSA levels in the context of other risk factors such as age, ethnicity, family history, and the prostate exam. From there we determine the need for additional testing.
You May Like: How Many Stages Of Prostate Cancer Are There
Screening Tests Have Risks
Decisions about screening tests can be difficult. Not all screening tests are helpful and most have risks. Before having any screening test, you may want to discuss the test with your doctor. It is important to know the risks of the test and whether it has been proven to reduce the risk of dying fromcancer.
Screening By Serum Psa
The prostate-specific antigen test has been examined in several observational settings for initial diagnosis of disease, as a tool in monitoring for recurrence after initial therapy, and for prognosis of outcomes after therapy. Numerous studies have also assessed its value as a screening intervention for the early detection of prostate cancer. The potential value of the test appears to be its simplicity, objectivity, reproducibility, relative lack of invasiveness, and relatively low cost. PSA testing has increased the detection rate of early-stage cancers, some of which may be curable by local-modality therapies, and others that do not require treatment. The possibility of identifying an excessive number of false-positive results in the form of benign prostatic lesions requires that the test be evaluated carefully. Furthermore, there is a risk of overdiagnosis and overtreatment . Randomized trials have therefore been conducted.
Read Also: What Does Prostate Inflammation Feel Like
Main Characteristics And Limitations Of The Trials
Figure 2 provides an overview of the trialsâ characteristics and the patients included. All trials had methodological limitations. In the CAP trial only 36% of men randomised to the screening arm actually underwent PSA testing , while about 10-15% in the non-screening arm were actually tested . CAP also differed from other large scale trials in that it used one-time screening, whereas others used repeated screening with intervals varying from annual to every two years or more.
Characteristics of patients and trials included in systematic review of the use of the prostate-specific antigen test for prostate cancer screening.1
The Prostate, Lung, Colorectal and Ovarian Cancer Screening trial conducted in the US21 lacked allocation concealment, and rates of PSA testing in the non-screening arm exceeded 50%, possibly as high as 80%.22
The European Randomised Study of Screening for Prostate Cancer was conducted in eight European countries.5 There was possibly inadequate allocation concealment, and there are concerns that groups may have received different quality of treatment for prostate cancer . Nevertheless, the systematic review authors judged the ERSPC trial to be the one that was probably least affected by bias. Based on a predefined sensitivity analysis,1 the BMJ Rapid Recommendations panel decided to appraise both the summary of the whole body of evidence as well as selected data at lower risk of bias from the ERSPC study .
Inadequate Evidence Of Benefit Associated With Screening For Prostate Cancer Using Prostate
The evidence is insufficient to determine whether screening for prostate cancer with prostate-specific antigen or digital rectal exam reduces mortality from prostate cancer. Screening tests can detect prostate cancer at an early stage, but it is not clear whether earlier detection and consequent earlier treatment leads to any change in the natural history and outcome of the disease. Observational evidence shows a trend toward lower mortality for prostate cancer in some countries, but the relationship between these trends and intensity of screening is not clear, and associations with screening patterns are inconsistent. The observed trends may be due to screening or to other factors such as improved treatment. Results from randomized trials are inconsistent.
Magnitude of Effect: Uncertain.
- Study Design: Evidence obtained from randomized trials and from observational and descriptive studies .
- Internal Validity: Fair.
- External Validity: Poor.
Harms
Magnitude of Effect: 20% to 70% of men who had no problems before radical prostatectomy or external-beam radiation therapy will have reduced sexual function and/or urinary problems.
- Study Design: Evidence obtained from cohort studies, case-control studies, and randomized controlled trials.
- Internal Validity: Good.
- External Validity: Good.
References
Don’t Miss: Metastatic Castration Resistant Prostate Cancer Life Expectancy
Harms Of Screening And Treatment
False-positive PSA test results are common and vary depending on the PSA cutoff used and frequency of screening. After 4 PSA tests, men in the screening group of the PLCO trial had a 12.9% cumulative risk of receiving at least 1 false-positive result and a 5.5% risk of having at least 1 biopsy due to a false-positive result.47 Men with false-positive PSA test results are more likely than control participants to worry specifically about prostate cancer, have a higher perceived risk for prostate cancer, and report problems with sexual function for up to 1 year after testing.48 In 1 study of men with false-positive PSA test results, 26% reported that they had experienced moderate to severe pain during the biopsy men with false-positive results were also more likely to have repeated PSA testing and additional biopsies during the 12 months after the initial negative biopsy.49 False-negative results also occur, and there is no PSA level that effectively rules out prostate cancer. This has, in part, led to recommendations for doing prostate biopsy at lower PSA thresholds than previously used in randomized screening trials .
Radiation therapy is associated with a 17% absolute increase in risk for erectile dysfunction and an increased risk for bowel dysfunction compared with watchful waiting after 1 to 10 years the effect on bowel function is most pronounced in the first few months after treatment.9, 10
Fewer Incidence Of Cancer Moderate
©BMJ Publishing Group Limited.
Disclaimer: This infographic is not a validated clinical decision aid. This information is provided without any representations, conditions or warranties that it is accurate or up to date. BMJ and its licensors assume no responsibility for any aspect of treatment administered with the aid of this information. Any reliance placed on this information is strictly at the user’s own risk. For the full disclaimer wording see BMJ’s terms and conditions:
Don’t Miss: Can Urgent Care Treat Prostatitis
Potential Harms Of Screening And Treatment
Potential Harms of Screening and Diagnosis
In addition to the ERSPC and PLCO trials, the USPSTF examined the results of a good-quality cohort study embedded within the ProtecT trial , a fair-quality cohort study conducted in the US Department of Veterans Affairs health system, as well as a report on complications of prostate biopsy from the ERSPC Rotterdam site to understand the potential harms of screening and diagnosis.3
In the large RCTs, one-fourth to one-third of men offered PSA-based screening had at least 1 positive screening test result. In the PLCO trial, 13% of men had undergone at least 1 biopsy. In the ERSPC trial, nearly 28 biopsies were performed for every 100 men randomized to screening.3 In the ProbE trial, 7.3% of men reported moderate or greater pain, 5.5% reported moderate to severe fever, and 26.6% reported troublesome hematospermia within the 35 days after biopsy.28 Complications from transrectal prostate biopsy resulted in 1.3% of men in the UK cohort, 1.6% of men in the VA cohort, and 0.5% of men in the Rotterdam cohort requiring hospitalization.30-32 In these studies, two-thirds to three-fourths of biopsies demonstrated that the PSA screening test was a false positive.3
Potential Harms of Treatment
In several studies, men older than 70 years had a significantly increased risk of medical complications and perioperative mortality after radical prostatectomy compared with younger men.3
Prostate Cancer Screening Patient Version
On This Page
Screening is looking for cancer before a person has any symptoms. This can help findcancer at an early stage. When abnormaltissue or cancer is found early, it maybe easier to treat. By the time symptoms appear, cancer may have begunto spread.
Scientists are trying to better understand whichpeople are more likely to get certain types of cancer. They also study the thingswe do and the things around us to see if they cause cancer. Thisinformation helps doctors recommend who should be screened for cancer, whichscreening tests should be used, and how often the tests should be done.
It is important to remember that your doctor does not necessarilythink you have cancer if he or she suggests a screening test. Screeningtests are given when you have no cancer symptoms. Screening tests may be repeated on a regular basis.
If a screening test result is abnormal, you may need to have more tests done to find out if you have cancer. These are called diagnostic tests.
Read Also: What Causes Prostate To Enlarge Mayo Clinic
At What Age Should You Get Screened For Prostate Cancer
The following prostate cancer screening guidelines apply to men expected to live at least ten years.
Men ages 45 to 49 should have a baseline PSA test.
- If the PSA level is 3 ng / mL or higher, men should talk with their doctor about having a biopsy of the prostate.
- If the PSA level is between 1 and 3 ng / mL, men should see their doctor for another PSA test every two to four years.
- If the PSA level is less than 1 ng / mL, men should see their doctor for another PSA test between the ages of 51 and 55.
Men ages 50 to 59 should have their PSA level checked.
- If the PSA level is 3 ng / mL or higher, men should talk with their doctor about having a biopsy of the prostate.
- If the PSA level is between 1 and 3 ng / mL, men should see their doctor for another PSA test every two to four years.
- If the PSA level is less than 1 ng / mL, men should see their doctor for another PSA test at age 60.
Men ages 60 to 70 should have their PSA level checked.
- If the PSA level is 3 ng / mL or higher, men should talk with their doctor about having a biopsy of the prostate.
- If the PSA level is between 1 and 3 ng / mL, men should see their doctor for another PSA test every two to four years.
- If the PSA level is less than 1 ng / mL, no further screening is recommended.
Men ages 71 to 75 should talk with their doctor about whether to have a PSA test. This decision should be based on past PSA levels and the health of the man.
There Is No Standard Or Routine Screening Test For Prostate Cancer
Although there are no standard or routine screening tests for prostate cancer, the following tests are being used or studied to screen for it:
Digital rectal exam
Digital rectal exam is an exam of the rectum. The doctor or nurse inserts a lubricated, gloved finger into the lower part of the rectum to feel the prostate for lumps or anything else that seems unusual.
Prostate-specific antigen test
A prostate-specific antigen test is a test that measures the level of PSA in the blood. PSA is a substance made mostly by the prostate that may be found in an increased amount in the blood of men who have prostate cancer. The level of PSA may also be high in men who have an infection or inflammation of the prostate or benign prostatic hyperplasia .
A PSA test or a DRE may be able to detect prostate cancer at an early stage, but it is not clear whether early detection and treatment decrease the risk of dying from prostate cancer.
Studies are being done to find ways to make PSA testing more accurate for early cancer detection.
Read Also: When Should You Get A Prostate Exam
Patient Population Under Consideration
This recommendation applies to adult men in the general US population without symptoms or a previous diagnosis of prostate cancer. It also applies to men at increased risk of death from prostate cancer because of race/ethnicity or family history of prostate cancer. The sections below provide more information on how this recommendation applies to African American men and men with a family history of prostate cancer.
Harms Of Detection And Early Treatment
The USPSTF found convincing evidence that treatment for prostate cancer detected by screening causes moderate-to-substantial harms, such as erectile dysfunction, urinary incontinence, bowel dysfunction, and death. These harms are especially important because some men with prostate cancer who are treated would never have developed symptoms related to cancer during their lifetime.
There is also adequate evidence that the screening process produces at least small harms, including pain and discomfort associated with prostate biopsy and psychological effects of false-positive test results.
Don’t Miss: Prostate Surgery Cost In Mexico
