What Are The Benefits Of Brachytherapy
If you want to avoid surgery or being treated with a radiation beam from a machine, then you might consider brachytherapy, Dr. Ciezki says.
Its a relatively fast treatment that doesnt require an incision or stitches. It typically has fewer side effects in the rectum and bladder, and its less costly than other radiation-based treatment options, he says.
This is a very minor procedure and it is performed in one day, he says. Typically, the concern with external beam radiation is that you can get rectal and bladder bleeding. But the rates of those side effects with brachytherapy are much lower.
Risks And Complications Of Brachytherapy
Some side effects occur immediately after your treatment or a few weeks later. In general, they are temporary, can last a few months and gradually disappear in the year following the end of treatment.
Short-Medium term
The side effects of brachytherapy are similar to those of external radiotherapy, but differ slightly. Piercing the prostate several times causes it to swell. This can cause urinary problems, the symptoms of which can manifest by:
- frequent urges to urinate, especially at night
- urge to urinate
- difficulty urinating with a weaker jet
- burning sensations during urination, sometimes even complete blockage of urine
Pain in the perineum, blood in the urine or sperm, transient erection problems may occur following treatment.
Irritation of the bowels and rectal disorders, such as inflammation of the rectum, are uncommon. On the other hand, though very rare, diarrhea, anal irritation, or rectal bleeding may occur in the months following treatment.
Side effects may be greater if brachytherapy is high dose and complementary to external beam radiotherapy.
Long Term
Long-term effects can appear months or years after treatment. Side effects vary but can include:
- Erectile dysfunction
- Significant decrease in ejaculate and infertility
- Risk of urinary incontinence or symptoms of chronic urinary obstruction are rare .
Which Is The Best Ldr Boost For Prostate Cancer
Currently, LDRBT alone should be offered to lowrisk prostate cancer patients, as well as EBRT alone, and/or RP. For patients with intermediaterisk prostate cancer choosing EBRT with or without ADT, BT boost should be offered.
PSA drop is different after radiation for prostate cancer Radiation, whether beam radiation or brachytherapy , causes a lowering of PSA about 12-14 months later. This is because radiation gradually exerts damaging pressure on PCa DNA so cells begin to die off. Also, they are unable to reproduce themselves.
Don’t Miss: Female Equivalent Of Prostate
Who Qualifies For Hdr Prostate Brachytherapy Focal Therapy
Patients who have a local only recurrence after previous radiation therapy are potentially candidates for “focal salvage”. In this type of treatment only the area of recurrence is treated rather than retreating the entire prostate gland. The rationale for this is that the majority of men who develop a local recurrence after radiation do so at the site of where the most dominant focus of disease was at the beginning of treatment. The goal of focal salvage is to cure the patient of his disease while limiting the risk of both short and long term side effects. Focal therapy in the up-front setting with no previous treatment is not currently standard of care and is best pursued on a clinical trial.
The physician determines whether HDR monotherapy or combination therapy is appropriate for the patient during his initial consultation.
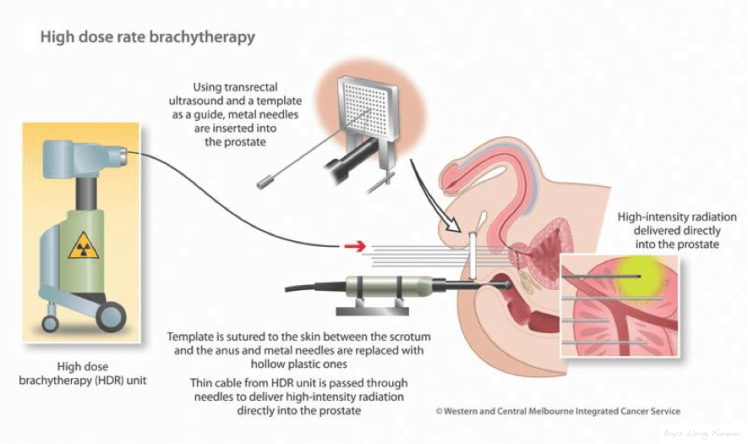
Below is an example of the standard template that we use for prostate brachytherapy here at UCLA.
Once the flexiguides are in position the template is sutured to the perineum to stabilize the implant.
A camera is used to look into the bladder to ensure appropriate placement of the flexiguides and then a foley catheter is left in the bladder.
After a brief stay in the recovery room the patient has a CT simulation where the placement of the flexiguides is confirmed. Once the images of the implant are obtained the patient waits for the customized treatment plan to be generated.
Effects On The Bladder
These can be a problem after brachytherapy. If you already have difficulties passing urine, you will not usually have brachytherapy, as it may make bladder problems worse.
It is normal to see some blood in your urine and semen for a few weeks after treatment. If bleeding gets worse or you have large clots, tell your doctor straight away. Drinking plenty of water helps flush your bladder and prevent blood clots.
You may also:
- have discomfort or pain passing urine
- need to pass urine urgently and more often.
Drinking plenty of water and avoiding caffeine and alcohol will help improve these symptoms.
Not being able to pass urine
Brachytherapy may cause swelling of the prostate. This may make it difficult to pass urine. If this happens, you may need to have a catheter put in your bladder until the swelling goes down.
Sometimes radiotherapy can narrow the urethra . This causes difficulties with passing urine. This may happen weeks, months or even years after treatment finishes. A stricture can be treated by passing a thin, plastic tube through the urethra to widen it.
See also
Recommended Reading: What Happens After Chemo For Prostate Cancer
Biochemical Control And Overall Prostate Cancer
The number of patients who showed biochemical failure was higher in the HDR-BT+EBRT group than in the LDR-BT group . The actuarial 5-year biochemical failure-free survival rates were 96.3% and 95.7% in the HDR-BT and LDR-BT groups, respectively. The corresponding values were 100% and 96.5% in the low-risk groups 97.4% and 97.1% in the intermediate-risk groups and 95.7% and 94.9% in the selected high-risk group, respectively. IPTW correction indicated no significant difference in all groups .
Figure. 2
Biochemical control rates between HDR-BT with EBRT and LDR-BT with or without EBRT. Biochemical control rates between HDR-BT with EBRT and LDR-BT with or without EBRT in the total population. Low risk group. Intermediate group. Lower titer of intermediate group. Higher titer of intermediate group. High risk group. bNED=no biochemical evidence of disease.
The 5y-bNED in the HDR+EBRT, LDR+EBRT, and LDR alone groups were 96.3%, 95.5%, and 97%, respectively . The corresponding values were 97.4%, 94.7%, and 96.6% in the intermediate-risk group and 95.7%, 95.5%, and 100% in the high-risk group, respectively .
Figure 3
Biochemical control rates among three groups . Biochemical control rates between HDR-BT with EBRT and LDR-BT with or without EBRT in the total population. Low risk group. Intermediate group. Lower titer of intermediate group. Higher titer of intermediate group. High risk group. bNED=no biochemical evidence of disease.
Figure 4
When Does The Psa Drop After Brachytherapy
PSA drop is different after radiation for prostate cancer Radiation, whether beam radiation or brachytherapy , causes a lowering of PSA about 12-14 months later. This is because radiation gradually exerts damaging pressure on PCa DNA so cells begin to die off. Also, they are unable to reproduce themselves.
Recommended Reading: Does Enlarged Prostate Affect Ejaculation
When Does The Bounce Show Up After Brachytherapy
Thus, the greater the presence of T cells before treatment, the more likely there will be a significant anti-tumor immune response when the effects of radiation wear off due to the natural decay of the radioactive isotopes used in brachytherapy. This is why it takes 1-2 years for the bounce to show up.
Inflammation Of The Back Passage
Inflammation of the back passage is a long term side effect. Proctitis can cause a feeling of wanting to strain whether or not you actually need to pass a bowel movement. You might also have bleeding from your back passage or a slimy mucous discharge.
Bleeding is usually slight but can be more severe for some people. Talk to your radiographer or nurse if you have proctitis. They might suggest you use treatments such as steroid suppositories for a short time. This might reduce the inflammation.
Recommended Reading: What Is Perineural Invasion In Prostate Cancer
Indications For High Dose Rate Brachytherapy
Currently, the main indication for HDR brachytherapy is in the context of safe dose escalation to the prostate, for intermediate- and high-risk disease in which pelvic treatment is required and the radiation dose is limited by bowel tolerance. In these circumstances, the HDR is given as a boost treatment to the prostate together with EBRT to the pelvis. This has gained National Institute for Health and Clinical Excellence approval since 2005 . Although there are reports of using HDR brachytherapy as monotherapy, this tends to be reserved for lower-risk disease and should be considered investigational at this stage.
What Are The Pros And Cons Of Brachytherapy
Brachytherapy is highly effective at treating prostate cancer. But its main benefit is that it limits radiation exposure to the surrounding areas. The normal structures around the prostate get close to no radiation, which is really dramatic, and that’s why people tolerate these treatments so well, Horwitz said.
Recommended Reading: Prostate Cancer Perineural Invasion Radical Prostatectomy
Permanent Or Low Dose Rate Brachytherapy
Low dose rate brachytherapy, often called by its acronym LDR , uses very low levels of radiation. Radiation is emitted from small radioactive sources containing radioiodide Iodine-125.
These sources look like grains of rice and are permanently implanted into the prostate. The radiation gets weaker with time and after 6 months 95% of the radioactive material is used up. Permanent implants do not cause any longterm problems.
This form of treatment is recommended for patients who have been diagnosed with a localized prostate cancer that is still relatively early stage , growing slow and thus at a low risk of progression and low PSA rate. Brachytherapy may be an option for cancers of intermediate risk of progression , but patients are selected according to a highly specific criteria.
Treatment For A Rising Psa After Brachytherapy

A PSA test measures prostate-specific antigen levels in the blood. Benign enlargement of the prostate, inflammation of the prostate, and prostate cancer can all cause a high PSA.
PSA levels sometimes rise after brachytherapy. However, your doctor wont recommend further cancer treatment based on this test alone. Theyll look for a rising trend in PSA over time and consider other factors, such as imaging tests, before recommending further treatment.
Even if your doctor cant see cancer cells with imaging, they may recommend you undergo treatment again based on a risk-benefit analysis. The benefit of catching all the cancer may outweigh the risk of additional treatment.
Recommended Reading: What Is Perineural Invasion In Prostate Cancer
Who Is Eligible For Brachytherapy
Brachytherapy is widely used to treat men with all different stages of prostate cancer. Brachytherapy alone is used for men with early-stage and some intermediate risk prostate cancers and in combination with intensity modulated radiation therapy for men with larger prostate cancers. All men should be evaluated to see if it is a good treatment option for them. However, it may not be ideal for men who already have significant urinary issues such as frequency, urgency, or incomplete emptying, since those may be exacerbated by brachytherapy treatments. For patients with larger prostate glands, it can also be harder to accurately place the radiation.
According to Horwitz, there are some instances where traditional, noninvasive radiation therapies may be preferable.
The brachytherapy implant is a small surgical procedure, but it does involve anesthesia, he said. So for people who have a cardiac history, it may not be as safe for them. In addition, people using blood thinners may want to opt for a less invasive treatment.
But if a person is relatively healthy and it’s safe for them to have anesthesia, then they can do either.
Benefits Of Brachytherapy For Prostate Cancer
Brachytherapy for prostate cancer is internal irradiation of the prostate. This treatment option is primary in case of non-metastatic cancer. It allows preserve the prostate and avoid complications. Brachytherapy is an alternative therapy to radical prostatectomy.
The advantages of brachytherapy in case of prostate cancer are the following:
- minimally invasive procedure
- A patient is under general anesthesia. The operating area is sterilized.
- A doctor inserts the catheter to withdraw the urine.
- The special probe is placed in the rectum to make images of operation and transmit them on the screen.
- A specialist inserts 15-30 needles into the prostate. Their quantity depends on the prostate size.
- Through each needle it is possible to place 1-6 radioactive seeds.
- The brachytherapy for prostate takes 1-2 hours.
- Then a patient is hospitalized. The next day after brachytherapy, a doctor examines mans health and removes the catheter. A patient returns home.
Process of brachytherapy for prostate cancer
Also Check: Can Prostate Issues Cause Erectile Dysfunction
Don’t Miss: Va Disability Rating For Prostate Cancer
Back To Top31 Effectiveness Of Monotherapy
Methods
Between January 1996 and December 2003, 117 consecutive patients were treated with a series of 2 HDR implants to minimize injury to normal tissue. The procedures were performed approximately 1 week apart to allow recovery of normal tissue effects of treatment. Three doses of HDR were delivered during each implant. The risk group characteristics were T1c and T2 , Gleason 6 and 7, PSA < 10 and 10-20. The risk group profile was low in 75% and intermediate in 25% of cases. The total HDR dose was escalated from 36 to 43.5 Gy over the course of our experience, since we observed excellent tolerance to therapy. The planning volume was calculated at least 5mm beyond the prostate capsule in order to encompass possible microscopic extensions of disease. The posterior margin or treatment varied according to the proximity of the anterior rectal wall to minimize side effects. The normal tissue dose constraints were anterior rectum 80% , bladder 85%, and urethra 108%. Median follow-up duration was 2 years and the mean was 2.5 years. Three different definitions of PSA progression were studied. They were the ASTRO definition , two consecutive rises of at least 0.5 ng/ml, and nadir +2 ng/ml. Morbidity analysis was based upon RTOG criteria.
Results
The CET HDR Monotherapy protocol is safe and effective therapy for low and early intermediate risk group prostate cancer.
Advantages of HDR Monotherapy
Pioneer In Prostate Cancer Treatment Leads Data
With over 6000 prostate cancer brachytherapy procedures to date and thousands of IMRT patients, Dr. John Sylvester is a leading authority on research to combat this deadly disease. He recently shared his thoughts on the most effective treatment combinations, and recommendations to patients on how to ensure they are receiving the highest-quality treatment.
Dr. John Sylvester
Citing a study he worked on in 2009, Dr. Sylvester believes that a radioactive seed treatment known as Brachytherapy, combined with external beam radiation treatment, had the highest success rate in intermediate risk patients compared to all other treatments, and that this success rate is significantly higher than surgery, external beam radiation, or proton beam radiation alone.
Brachytherapy is a treatment where tiny radioactive seeds are implanted into the prostate to perform a much more targeted form of treatment and limit radiation exposure to areas outside of the cancer. Dr. Sylvester broke down how well this technique performs in combination with other treatments, as opposed to utilizing surgery or external beam radiation alone.
Also Check: Low Dose Cialis For Prostate
Back To Top73 Radiograph Based Dosimetry
| Fig 6: This is an “AP” radiograph of a CET prostate implant. The blue markings are the rectal outline and dose calculation points for the bladder, urethra and rectum. “Dummy” markers are inserted in the catheters. Contrast is introduced into the bladder . Contrast is also used to inflate the foley balloons in the bladder and rectal catheters. The bladder catheter is made of a radio-opaque material to see the urethra clearly. Notice how the catheters can be made to flare in order to encompass any extracapsular extension. |
| Fig 7: This is a lateral of the CET prostate implant. The physicians try to lift the prostate away from the rectum to help achieve low rectal doses. Notice how the tips of the catheters are against the bladder. This ensures that any tumor in the base of the gland is adequately treated, yet by adjusting the time the source spends in the tip “dwell” positions, the bladder doses are controlled. |
Will I Experience Discomfort After Treatment
You may experience on or more of the following side effects:
- Bruising may appear on the testicles or penis immediately after treatment or several days later. This is normal and usually not very painful. To relieve bruising, apply ice to the affected area and take pain killers.
- Blood can be found in your urine a few hours or a few days after your treatment. This is normal. If you see small clots or lumps of blood in your urine, drink a lot of water and it should pass.
- In the month following your treatment, you may need to urinate more often. You may also feel a slight burning sensation when urinating. If this is the case, speak with your doctormedication can help.
- Bowel movements may cause some pain if your anus is irritated. Some people will also have diarrhea. These rare side effects go away about 5 weeks after treatment, but can occasionally recur.
Important
If you are unable to urinate, call your radiation oncology clinic. Outside business hours, call 9-1-1 to get emergency medical help or go to the hospital emergency department.
Also Check: Is Cranberry Juice Good For Prostate Infection
Radioactive Seed Therapy Returns 80
Active retiree Larry Fenster is a problem-solver. So when he was diagnosed with prostate cancer, he searched for solutions. Mr. Fenster, 80, soon found out that he was a prime candidate for brachytherapy . The treatment would allow him to avoid surgery and traditional radiation therapy.
For several years, the Manhasset resident an avid golfer who enjoys traveling with his wife watched his concentration of PSA rise from a normal score below 4.0 nanograms per milliliter all the way up to 10.
A prior biopsy did not show cancer, but his urologist, Robert Waldbaum, MD, of Northwell Healths Smith Institute for Urology, ordered parametric magnetic resonance imaging .
The scan revealed a mass in Mr. Fensters prostate, and a directed re-biopsy confirmed that he had Stage II cancer. Dr. Waldbaum referred him to Louis Potters, MD, Northwells chair of radiation medicine and deputy physician-in-chief of radiation medicine for the health systems Cancer Institute.
