How Will I Know That My Hormone Therapy Is Working
Doctors cannot predict how long hormone therapy will be effective in suppressing the growth of any individual mans prostate cancer. Therefore, men who take hormone therapy for more than a few months are regularly tested to determine the level of PSA in their blood. An increase in PSA level may indicate that a mans cancer has started growing again. A PSA level that continues to increase while hormone therapy is successfully keeping androgen levels extremely low is an indicator that a mans prostate cancer has become resistant to the hormone therapy that is currently being used.
Neoadjuvant Or Adjuvant Androgen Deprivation Therapy For Rp
Neoadjuvant or adjuvant ADT with RP may have benefits in some patients with local or locally advanced PCa, where there is evidence that this approach provides a significant survival advantage . The European Association of Urology guidelines recommend that adjuvant ADT be offered upon detection of nodal involvement during RP .
Read Also: Homeopathic Treatment For Prostate Cancer
Cancer That Is Thought To Still Be In Or Around The Prostate
If the cancer is still thought to be just in the area of the prostate, a second attempt to cure it might be possible.
After surgery: If youve had a radical prostatectomy, radiation therapy might be an option, sometimes along with hormone therapy.
After radiation therapy: If your first treatment was radiation, treatment options might include cryotherapy or radical prostatectomy, but when these treatments are done after radiation, they carry a higher risk for side effects such as incontinence. Having radiation therapy again is usually not an option because of the increased potential for serious side effects, although in some cases brachytherapy may be an option as a second treatment after external radiation.
Sometimes it might not be clear exactly where the remaining cancer is in the body. If the only sign of cancer recurrence is a rising PSA level , another option for some men might be active surveillance instead of active treatment. Prostate cancer often grows slowly, so even if it does come back, it might not cause problems for many years, at which time further treatment could then be considered.
Factors such as how quickly the PSA is going up and the original Gleason score of the cancer can help predict how soon the cancer might show up in distant parts of the body and cause problems. If the PSA is going up very quickly, some doctors might recommend that you start treatment even before the cancer can be seen on tests or causes symptoms.
Also Check: Non Metastatic Prostate Cancer Treatment
What To Ask When Your Psa Is Rising After Initial Treatment
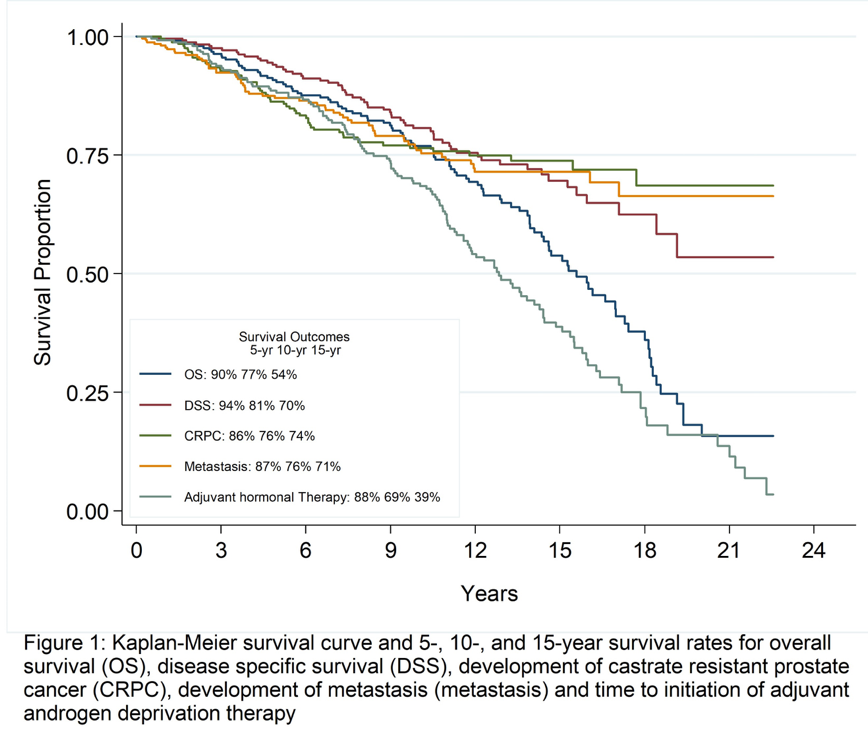
For the majority of men, prostate cancer is treatable and curable and does not come back after initial treatment. However, about 25%33% of men with prostate cancer will experience a recurrence of their cancer after surgery or radiation. Some of these men can still be cured with additional treatment, but some men develop a form of prostate cancer that, while not curable, remains TREATABLE for a very long time.
Below is a list of questions to ask when your PSA is rising after initial treatment.
What If The Treatment Stops Working
Sometimes prostate cancer doesn’t respond to hormone therapy or other treatments, or it stops responding after a period of success. So many new treatments are available for recurrent prostate cancer that you still have a lot of options.
Your doctor might recommend one of these treatments:
Sipuleucel-T . This is a prostate cancer vaccine. It boosts your immune system response to help it attack cancer cells.
Immunotherapy. Pembrolizumab takes the brakes off of your immune system so that it can fight the cancer better.
Targeted therapy. Olaparib and Rucaparib are drugs called PARP inhibitors. They prevent cancer cells from repairing their damaged DNA. When cancer cells can’t fix themselves, they die. These drugs are for people who have mutations in the BRCA genes.
Another option is to enroll in a clinical trial. These studies test out new treatments, including cancer vaccines and drugs called monoclonal antibodies, that are being reviewed for safety and effectiveness. The experimental treatments you get in a clinical trial might work better against your cancer than treatments you’ve already tried, but they have yet to be approved for wider use.
Recommended Reading: What Is Stage 9 Prostate Cancer
Are There Different Types Of Hormone Therapy For Prostate Cancer
Yes. There are several different ways to block the secretion of testosterone, including the surgical removal of the testes, drugs known as LHRH agonists, and drugs called LHRH antagonists. These are considered standard hormone therapy. Another class of medications that can be used in combination with standard hormone therapy is called antiandrogens.
In the past decade, newer medicines called androgen directed therapies have been approved for certain states of advanced prostate cancer.
Salvage External Beam Radiotherapy For Prostate Cancer After Radical Prostatectomy
James B. Yu, MD, MHSOncology
This article defines the biochemical recurrence of prostate cancer, distinguish SRT from ART, outline the evidence for SRT, and makes recommendations with regard to radiotherapy volume and dose.
Prostate cancer is the second most common cause of cancer death in American men. What to do when prostate cancer recurs months or years after a patient undergoes radical prostatectomy is an area of active research. Patients who underwent radical prostatectomy without immediate adjuvant radiation therapy but subsequently have evidence of recurrent disease are candidates for Salvage Radiation Therapy . Though there are three prospective randomized trials illustrating the efficacy of post-operative ART for selected patients, similarly strong evidence is lacking for SRT. In this article, we define the biochemical recurrence of prostate cancer, distinguish SRT from ART, outline the evidence for SRT, and make recommendations with regard to radiotherapy volume and dose. We discuss the known side effects from SRT, weigh the cost and benefit of SRT, and discuss possible tools that may improve the cost/benefit ratio for SRT by helping to select patients whom SRT may be more likely to benefit.
Don’t Miss: How To Fix Enlarged Prostate
Additional Treatment After Surgery
Additional treatment can come with one of two approaches: treatment given as adjuvant therapy , or as salvage therapy . In the modern era, most additional treatment is given as salvage therapy because firstly this spares unnecessary treatment for men who would never experience recurrence, and secondly because the success rates of the two approaches appear to be the same.
Regardless of whether an adjuvant or salvage therapy approach is taken, the main treatment options following biochemical recurrence are:
- Radiotherapy this is the commonest approach. Because scans dont show metastatic deposits until the PSA is more than 0.5 ng/ml and because radiotherapy is more effective when given before this level is reached, the radiotherapy energy is delivered to the prostate bed. This is because we know that this is the commonest site of recurrence in most men, and that 80% of men treated in this way will be cured.
- Active surveillance this is appropriate for a very slowly-rising PSA in an elderly patient who has no symptoms.
- Hormonal therapy in many ways this is the least appealing option as it causes symptoms but does not cure anyone, although it does control the recurrence and lower the PSA.
What Should My Psa Level Be After Treatment
Following surgery , your PSA number should be undetectable after about a month. This is effectively zero PSA, but may not get all the way to zero, given the sensitivity of the test and the fact that other proteins may be misread as PSA proteins. The most widely accepted definition of a prostate cancer recurrence after surgery is a PSA of 0.2 ng/mL or greater on at least two separate occasions.
If youve had radiation therapy, your PSA will likely not drop to zero, as there is some normal, healthy prostate tissue that remains after treatment. Instead, there is a different low PSA level for each patient, called a nadir. The most widely accepted definition is a PSA that has risen from nadir by 2 ng/mL or more. Either way, its important to always use the same lab, if possible, for all of your PSA tests because PSA values can fluctuate somewhat from lab to lab. Defining failure after other forms of therapy like brachytherapy seeds or cryotherapy is more challenging, but similar to that used with external radiation.
If your PSA is rising but doesnt quite meet these definitions, your doctor may recommend an evaluation to see whether your prostate cancer has recurred.
Also Check: Prostate Cancer To Bone Cancer
What Is Hormone Therapy For Prostate Cancer
Hormone therapy is a key treatment strategy for prostate cancer that has recurred following treatment for localized disease. Testosterone is a male hormone that fuels the growth of prostate cancer cells. The goal of hormone therapy is to stop the production and/or interfere with the effects of testosterone. However, not all prostate cancer cells are sensitive to decreases in testosterone levels, and, over time, the cancer can adapt to survive in a low-testosterone environment. Therefore, hormone therapy is a treatment for prostate cancer but does not cure the disease. The decision to start hormone therapy is individualized, based on your PSA, the PSA doubling time, whether the cancer has spread visibly or caused symptoms, and the potential side effects and risks involved with this type of therapy.
What Does Psa Velocity Mean
PSA velocity or PSA doubling time, both of which measure the rate at which your PSA rises, can be a very significant factor in determining is the aggressiveness of your cancer. Men with a shorter PSA doubling time or a more rapid PSA velocity after initial therapy tend to have more aggressive disease, and are therefore more likely to need more aggressive therapies. Likewise, men who have recurrence soon after surgery have a higher risk of aggressive disease.
Also Check: Are Eggs Bad For The Prostate
Treatments For Recurrent Prostate Cancer
Recurrent prostate cancer is cancer that comes back after it has been treated. Recurrent prostate cancer is also diagnosed when theprostate-specific antigen level starts to rise quickly after initialtreatment but there are no other signs of cancer. This is called a biochemicalrecurrence or PSA failure.
The following aretreatment options for recurrent prostatecancer. Your healthcare teamwill suggest treatments based on your needs and work with you to develop atreatment plan. The type of treatment that you receive will depend on:
- the treatments youve already had
- where the cancer comes back
- whether the cancer has spread
- your overall healthand whether you have other illnesses
- your age and life expectancy
- your personal preferences
Also Check: Is Prostate Cancer Genetically Inherited
Im Worried About All The Side Effects From Prostate Cancer Medications What Can I Do
Carefully review the side effect profile of the different hormone therapy regimens, and discuss with your health care team potential ways to minimize the effects. In the end, its important that you not only understand the value of the therapy in the management of your prostate cancer, but also that you learn how to live your life as best as possible while fighting the disease.
Recommended Reading: What Age Do Doctors Check Prostate
Evaluation Of Local And Lymph Node Involvement Recurrence By Choline Pet Tracers
18F-fluorodeoxyglucose PET imaging is a well-established tool in radiation therapy planning, extensively used in many tumor types. The lack of FDG avidity in most PCa has motivated the search for alternative metabolic tracers, and among them, the most commonly used are choline tracers. Three main choline-based PET tracers exist, namely, 11C-choline, 18F-methylcholine, and 18F-ethylcholine: regardless of the slight chemical differences impacting overall distribution and the lack of formal comparative studies, available data suggest that their diagnostic performance is overall similar . 11C-acetate is another tracer, less commonly used in PCa, sharing with choline tracers a similar distribution, and being transformed to phosphatidylcholine after uptake . Studies have shown that performance is similar to 18F-choline .
The literature on the use of choline PET in recurrent PCa is vast but inhomogeneous, and for this reason, its use in recent guidelines is suggested but not established, yet. Two recent meta-analyses have tried to overcome this limitation, with encouraging and converging results when selecting studies with common inclusion criteria, protocols, and standard of reference . Both analyses obtained pooled sensitivities and specificities above 85% in patients with biochemical recurrence. For local recurrence, in particular, the sensitivity was 61% and the specificity 97% .
Management Of Biochemically Recurrent Prostate Cancer After Local Therapy: Evolving Standards Of Care And New Directions
Channing J. Paller, MD, and Emmanuel S. Antonarakis, MD
Clinical Advances in Hematology & Oncology
Channing J. Paller, MD, and Emmanuel S. Antonarakis, MD
Drs. Paller and Antonarakis are Assistant Professors of Oncology at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins, in Baltimore, Maryland.
Address correspondence to: Emmanuel S. Antonarakis, MD, Assistant Professor of Oncology, Prostate Cancer Research Program, Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins, 1650 Orleans Street, CRB1-1M45, Baltimore, MD 21231 Phone: 443-287-0553 Fax: 410-614-8397 E-mail: eantona1@jhmi.edu
Introduction
Fewer than 12% of the 241,700 men expected to have been diagnosed with prostate cancer in the United States in 2012 will die from this disease.1 Many more patients will experience rising prostate-specific antigen levels following local therapy, a condition known as biochemical recurrence . Physicians treating patients with BCR face a difficult set of decisions in attempting to delay the onset of metastatic disease and death while avoiding over-treating patients whose disease may never affect their overall survival or quality of life. In this generally healthy population, effective management requires that physicians evaluate PSA levels, as well as clinical and radiologic indicators, in order to balance the morbidity and efficacy of proposed treatments against the risks of metastatic progression.
Defining Biochemical Recurrence
Selection of Hormonal Agents
Recommended Reading: What Is The Survival Rate Of Metastatic Prostate Cancer
What Factors Determine The Likelihood Of Recurrence
Several signs can point to a prostate cancer that has come back or spread, including:
- Lymph node involvement. Men who have cancer cells in the lymph nodes in the pelvic region may be more likely to have a recurrence.
- Tumor size. In general, the larger the tumor, the greater the chance of recurrence.
- Gleason score. The higher the grade, the greater the chance of recurrence. Your doctor can tell you your score when the biopsy results come back from the laboratory.
- Stage. The stage of a cancer is one of the most important factors for selecting treatment options, as well as for predicting future outlook of the cancer.
Recurrent Prostate Cancer After Radiation Therapy
Once a patient has received radiation therapy to the prostate gland, more radiation therapy typically cannot be given to the same area safely. Systemic treatment with ADT is the mainstay of treatments for individuals with recurrent prostate cancer following primary treatment with radiation. Rarely, surgeons have removed the prostate gland for persistent cancer after radiation therapy. Other surgeons have used cryosurgery, which is a local treatment where the prostate gland is frozen with a probe. Complications of surgery or cryosurgery, however, tend to be more frequent in patients previously treated with radiation therapy. If a patient is not a candidate for these types of local therapies or ADT other systemic treatments like chemotherapy or immunotherapy are used.
Don’t Miss: What Is The Scale For Prostate Cancer
What Is Intermittent Hormone Therapy
With intermittent hormone therapy, the LHRH agonist is used for 612 months, during which time a low PSA level is maintained. The drug is stopped until the PSA rises to a predetermined level, at which point the drug is restarted. During the drug holidays in between cycles, sexual function and other important quality of life measures might return. However, this approach is not right for all patients, and a patient-by-patient approach should be used based on response to and tolerability of hormone therapy.
Why Does Breast Cancer Come Back After Treatment
Even with the best treatment, cancer can come back. If just a few cancer cells remain in your body after your initial treatment, those cells can spread through the blood or lymph system and grow. This may happen from a few months to many years after the first diagnosis.
If your breast cancer has come back, you may second-guess your previous treatment choices. But the fact is, there is no guarantee with any treatment. Now it is time to make new decisions and explore other treatment options.
Recommended Reading: Can Prostate Cancer Metastasis To The Colon
Recommended Reading: Can Cancer Return After Prostate Removal
Can I Have Radiation Therapy First And Then Surgery
With modern radiation therapy techniques, local tissue damage is often kept at a minimum, and surgeons at some of the larger cancer centers have been seeing improved results with salvage prostatectomy performed after radiation. But even under the best of circumstances, post-radiation surgery is a very difficult operation to perform, and few surgeons across the country perform it regularly.
Timing And Duration Of Adt
Physicians wishing to treat BCR prostate cancer patients with ADT face 2 key timing questions: 1) whether to initiate ADT immediately upon PSA recurrence or to defer its use until after clinical/radiographic progression occurs, and 2) whether to use continuous administration of ADT or intermittent cyclic administration of ADT. As of December 2012, the American Society of Clinical Oncology had not provided definitive guidelines addressing either of these questions. We will review the relevant clinical trial data that may guide clinicians with respect to these 2 issues.
You May Like: Green Light Laser Surgery For Prostate
How Does Hormone Therapy For Prostate Cancer Work
LHRH, or luteinizing-hormone releasing hormone, is one of the key hormones released by the body that initiates the production of testosterone.
LHRH Agonists: One of the most common hormone therapies in prostate cancer involves blocking the release of LHRH through the use of agonists . LHRH agonists cause a testosterone flare reaction, which is an initial transient rise in testosterone that happens over the first week or two after the first treatment.
LHRH Antagonists: These are a class of medications that can block LHRH from stimulating testosterone production without causing an initial testosterone surge.
