Molecular Classification Of Multifocal Prostate Cancer
We successfully classified 58% of the cancer samples into one of the TCGA classes . In 2 out of these 106, we saw both overexpression/fusion and somatic point mutations. In total, 52% of all tumor foci could be classified into one class, 36% of the foci did not harbor any of the traits included in the TCGA classification, and 12% had conflicting traits . 20 out of 39 patients had molecular tumor alterations summarized into more than one of the defined classes, 12 patients were defined by a single class and in 7 patients none of the TCGA defined tumor traits were detected.
Figure 1
Molecular classes and clinicopathological information per patient and focus. Each column represents one tumor focus, and neighboring bars derive from the same patient. Each row represents the alterations defining a TCGA molecular class or clinicopathological feature Dark grey background: all samples from the patient have the same molecular class; light grey background: samples from the patient correspond to more than one molecular class; white background: none of the samples from the patient can be assigned to any of the seven TCGA classes. EPE: extra prostatic extension, BCR: biochemical recurrence.
Tests Used To Check The Prostate
This first step lets your doctor hear and understand the “story” of your prostate concerns. You’ll be asked whether you have symptoms, how long you’ve had them, and how much they affect your lifestyle. Your personal medical history also includes any risk factors, pain, fever, or trouble passing urine. You may be asked to give a urine sample for testing.
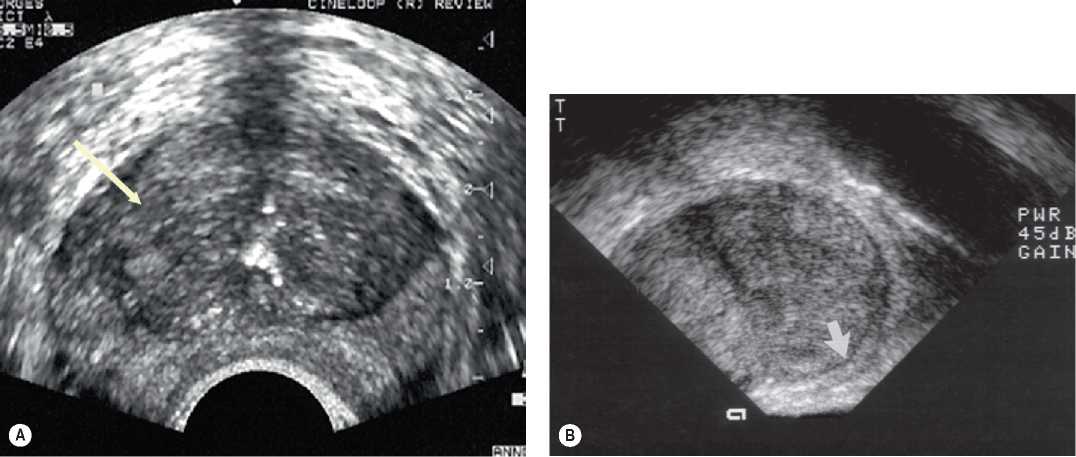
Transrectal Colour Doppler Imaging
Colour Doppler imaging is well established to illustrate macrovascularity and therefore perfusion. PCa has an increased microvessel density compared with healthy prostatic tissue. Therefore, Doppler visualization of streaming blood within the vasculature may aid in detecting and localizing PCa . In addition, the cancer grade correlates positively with the degree of Doppler signal. Other studies have compared Doppler-guided and systematic biopsies with achieving a detection rate of up to 40%.
Corresponding contrast-enhanced colour Doppler US showing clearly more enhancement of the left side . Targeted biopsy confirmed the presence of a Gleason score 3+4 cancer focus.
As a criterion for capsular penetration an increased capsular flow on colour Doppler imaging has been applied. Another study that performed Doppler TRUS staging revealed a sensitivity of 59% for detecting locally advanced disease. In addition, Doppler imaging also aids in differentiating fibrotic tissue from local recurrence of PCa.
You May Like: Does An Enlarged Prostate Affect A Man Sexually
Deformation Of The Prostate Due To Bph
Our model predicted that BPH produces the volumetric expansion of the prostate in the perpendicular direction to the CG border, as depicted in . The PZ was pushed outward from the borders of the growing CG against the prostate external surface and experienced a very slight shrinkage, as the boundary conditions partially enabled outward displacement.
Deformation of the prostate caused by BPH over 1 y. Length of the displacement field vector over original anatomy at t y. Original and deformed geometries of the prostate at t 1 y.
The extremal values of the displacements were attained at the CG borders that are closer to the external surface of the prostate. The maximum total displacement was 0.74 mm. The urethra was displaced posteriorly and its diameter was virtually unaltered.
The hydrostatic stress was compressive within the CG and negligible within the PZ . Positive hydrostatic stress appeared in thin PZ regions between the CG border and the prostate boundary, where tension accumulated as the CG expanded. The Von Mises stress was negligible within the CG, except along the urethra . Within the PZ, the Von Mises stress peaked near the borders of the CG and decreased toward the external surface of the prostate , depending on the distance between them .
Symptoms Of Prostate Cancer
- Frequent urge to pass urine, especially at night
- Weak or interrupted urine stream
- Pain or burning when passing urine
- Blood in the urine or semen
- Painful ejaculation
- Nagging pain in the back, hips, or pelvis
Prostate cancer can spread to the lymph nodes of the pelvis. Or it may spread throughout the body. It tends to spread to the bones. So bone pain, especially in the back, can be a symptom of advanced prostate cancer.
Recommended Reading: Does Cialis Shrink An Enlarged Prostate
During Prostate Tumor Development In Psa
To further explore which biological processes can be associated with tumor development, RNA expression of markers associated with several processes, like senescence, proliferation and angiogenesis, was analyzed. Previously, Chen et al. reported an increased expression of genes involved in the Trp53 dependent cellular senescence response in early hyperplasia stages of tumor development in the related Probasin -Cre targeted Pten knockout mouse model We also observed higher expression of Trp53, Trp53-regulated and Trp53-independent senescence markers Cdkn1a , and Cdkn2a in HP as compared to NP . Surprisingly, an even higher mRNA expression level of these markers was observed in prostate tumors, with significantly higher expression of Cdkn2a and Trp53 in TC2 tumors . The expression of p21 was further validated by IHC showing increased expression of p21 protein in HP and tumor samples compared to NP . Taken together these data indicate that diminished senescence is not a factor involved in tumor development from hyperplasia in the PSA-Cre;PtenLoxP/LoxP model.
Differential expression of markers associated with senescence, proliferation, angiogenesis and apoptosis in TC1 and TC2 prostate tumors as compared to HP/NP in targeted Pten knockout mice.
Prostate Imaging Features That Indicate Benign Or Malignant Pathology On Biopsy
Catherine Elizabeth Lovegrove1,2, Mudit Matanhelia1,2, Jagpal Randeva1,2, David Eldred-Evans1,2, Henry Tam1,2, Saiful Miah1,2, Mathias Winkler1,2, Hashim U. Ahmed1,2, Taimur T. Shah1,2
1Division of Surgery, Department of Surgery and Cancer, Imperial College London 2Imperial Urology, Charing Cross Hospital, Imperial College Healthcare NHS Trust , , UK
Contributions: Conception and design: None; Administrative support: None; Provision of study materials or patients: None; Collection and assembly of data: None; Data analysis and interpretation: None; Manuscript writing: All authors; Final approval of manuscript: All authors.
Correspondence to:
Keywords: Prostate; magnetic resonance imaging ; imaging; quantitative; qualitative; benign; malignant; parametric
Submitted Mar 01, 2018. Accepted for publication Jul 11, 2018.
doi: 10.21037/tau.2018.07.06
Read Also: Prostate Cancer Shortness Of Breath
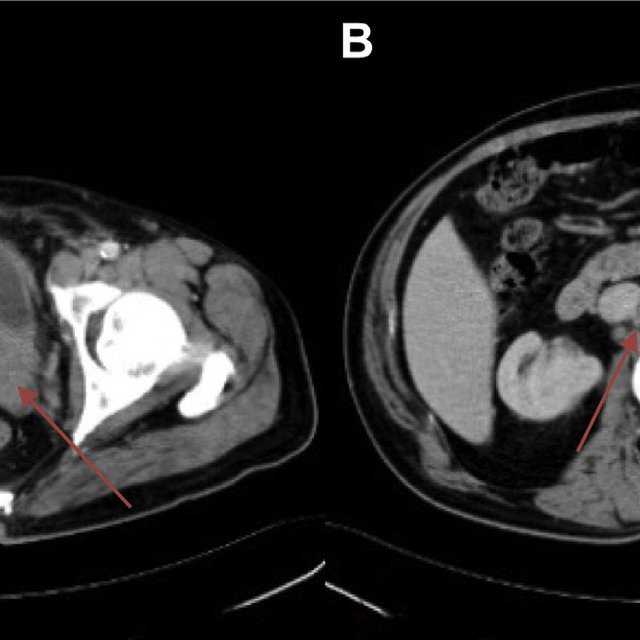
Rectal Gastrointestinal Stromal Tumours
Gastrointestinal stromal tumours are the most common mesenchymal tumours of the gastrointestinal tract accounting for approximately 5% of all sarcomas. The stomach and small bowel are the most commonly involved sites with GIST of the anal canal and rectum only accounting for about 5% of all GISTs in the gastrointestinal tract . They are typically submucosal tumours with usually intact mucosa on pathological and imaging assessment. They are thought to arise from the interstitial cells of Cajal with 95% staining positive for CD 117 9c-KIT and 70% for CD34 . On histology they are a relatively cellular tumour arising from the muscularis propria composed of spindle cells and plump epithelioid cells . They can have variable imaging appearances depending on the presence of necrosis, haemorrhage or cystic change but generally demonstrate a low T1 signal intensity solid component and high T2 signal intensity solid component with post-contrast enhancement. Surgical resection is the mainstay of treatment. The Choi response criteria for GIST, which proposed that tumour attenuation could provide an additional measure of response to imatinib therapy , is used to assess the treatment .
Fig. 22
Bladder Wall Thickening And Hydrocele
In an adequately distended bladder, bladder thickening and trabeculations can be diffuse as in Fig.; or focal. Causes of diffuse bladder wall thickening include bladder outlet obstruction, neurogenic bladder and cystitis. On prostate MRI, the most common cause would be chronic bladder outlet obstruction secondary to prostatomegaly. Focal bladder wall thickening is often concerning for malignancy such as urothelial carcinoma or other bladder neoplasms. Rare causes of focal bladder wall thickening include amyloidosis and malakoplakia.
A hydrocele represents serous fluid within the tunica vaginalis in the scrotum and hence follows fluid characteristics on MRI demonstrating low T1 signal and high T2 signal intensity. If complicated by infection or trauma, they can appear complex with septation or internal debris. Hydroceles, may be acquired or congenital, are common and present with painless enlargement of the scrotum. Congenital hydroceles are more common in children and may be subdivided into communicating or spermatic cord hydrocele . Acquired hydroceles can develop subsequent to trauma, epididymitis, testicular torsion, neoplasm or infarction .
Fig. 16
Sagittal T2W image shows large high T2 signal lesion in the right scrotum in keeping with a hydrocele , thickened bladder wall which is low T2 signal is in keeping with a trabeculated bladder wall with debris . Low T2 signal lesions seen in the prostate represent prostate calcifications as discussed previously in Fig.;
Recommended Reading: Swollen Prostate Constipation
Patient Cohort And Fresh
The total cohort consisted of 571 prostate cancer patients who underwent prostatectomies between 2010 and 2012 at Oslo University Hospital-Radiumhospitalet. Ethical approval for the study was obtained from the regional Ethics Committee South-East Norway . All included patients had acinar adenocarcinomas and informed consent was obtained from all patients before initiation of the study. All methods were performed according to the relevant guidelines and regulations. From this cohort, 39 patients with fresh-frozen cancer samples from at least two clearly distinct cancer foci were selected for this study. From each patient, samples from two or three distinct cancer foci and one corresponding benign tissue sample were included. In total, the sample set consisted of 145 cancer and benign samples representing 85 distinct cancer foci.
From each prostatectomy, three to seven tissue cores with diameter of 6mm were biobanked . The holes were marked and the sections and orientation photographed. Both cancer and benign samples were selected by a pathologist, based on microscopy of hematoxylin and eosin stained sections through formalin-fixed and paraffin-embedded tissue blocks of the remaining tissue. Samples were considered benign if they had no tumor tissue present around the site of the sample used for DNA and RNA extraction.
Total RNA and DNA were isolated from all samples using the AllPrep DNA/RNA/miRNA Universal Kit according to the manufacturers protocol.
Determining Clinically Significant Prostate Cancer
Clinically significant prostate cancer is frequently categorized according to three main prognostic factors as defined by Stamey and Epstein :
- Gleason score 7 or greater ;
- Extraprostatic tumor extension ;
- Tumor volume on whole-mount prostatectomy >0.5 cm3 .
This definition is derived from the seminal work of Hanahan and Weinberg . These lesions exhibit more malignant behaviour and are more likely to warrant treatment compared to smaller, less aggressive tumours that can be inconsequential . The parameters used to define clinically significant prostate cancer aid in prognostication of prostate cancer. However, these parameters are not used in isolation for clinical decision making where further patient characteristics including comorbidities, age, performance status and patient choice will further contribute.
Don’t Miss: Does Enlarged Prostate Cause Constipation
Expression Array Analysis Of Different Metastatic Tissues
We next sought to determine whether the heterogeneity in histology and phenotype was mirrored by heterogeneity in gene expression. With expression array data that we have previously generated , we performed hierarchical clustering of the 16 metastatic samples from six cases in the rapid autopsy series. The metastatic adenocarcinoma samples were highly heterogeneous . Only two metastases from a patient with small-cell histology demonstrated comparable cDNA expression results . With the ONCOMINE database, we found that these tumors exhibited a similar expression pattern as small-cell lung cancer .
Hierarchical clustering of 16 hormone-refractory metastatic prostate tumors from the rapid autopsy series demonstrates a small subset of genes that were specifically overexpressed in the small-cell phenotype but not in the more typical glandular adenocarcinoma .
Enlarged Prostate Treatments In The Pipeline
Researchers continue to investigate new therapies for enlarged prostates. “Another category of drugs is under development,” says Slawin. “We’ve come a long way in treating BPH. It’s no longer the life-threatening disease it once was. Now, in treatment, we’re working on quality of life issuesââ¬Â¦ reducing side effects of treatment.”
Also being studied is a procedure called water-induced thermotherapy , an experimental procedure that involves destroying excess prostate tissue utilizing heated water and an air-filled balloon, which protects normal prostate tissue. The procedure is performed with only local anesthesia. Results may not be fully apparent for three to four months. However, preliminary studies examining WIT have shown positive results, with a near doubling in urine flow. However, the American Urological Association has not thus far endorsed WIT as a viable treatment option for symptoms of BPH.
Don’t Miss: External Prostate Massage For Prostatitis
Testing Options For Prostate Cancer
There is no one age for prostate cancer testing, but the American Cancer Society makes recommendations about screenings. According to the ACS, patients in any of these groups should consider asking their doctor about testing:
- Men age 50 or older who have an average risk of prostate cancer and a life expectancy of at least 10 more years
- Men age 45 or older with a high risk, including African-American men and those with a first-degree relative who had prostate cancer before age 65
- Men age 40 or older who have a higher risk, such as more than one first-degree relative diagnosed with prostate cancer at an early age
Talking With Your Doctor
Different kinds of doctors and other health care professionals manage prostate health. They can help you find the best care, answer your questions, and address your concerns. These health care professionals include:
- Family doctors and internists
- Physician assistants and nurse practitioners
- Urologists, who are experts in diseases of the urinary tract system and the male reproductive system
- Urologic oncologists, who are experts in treating cancers of the urinary system and the male reproductive system
- Radiation oncologists, who use radiation therapy to treat cancer
- Medical oncologists, who treat cancer with medications such as hormone treatments and chemotherapy
- Pathologists, who identify diseases by studying cells and tissues under a microscope
View these professionals as your partnersâexpert advisors and helpers in your health care. Talking openly with your doctors can help you learn more about your prostate changes and the tests to expect.
Recommended Reading: Enlarged Prostate Sexuality
Selection Of Stem Cells Transit Amplifying Cells And Committed Basal Cells
Following trypsinisation of primary cultures, cells were first selected using collagen adherence. stem cells and transit amplifying cells are 21integrinhi and committed basal cells are 21integrinlo. A stringent selection of TA cells can be achieved with 5 min adherence to collagen I. Any non-adherent cells can be passed on to another plate, then any cells not adhered after 20 min are the committed basal cells. A slightly less stringent selection of TA cells can be achieved with a 20 min adherence where any non-adherent cells represent the committed basal population. This latter selection can be used when trying to achieve maximum stem cell yield. To select stem cells, positive selection using a CD133 microbead kit was used.
Transcriptomic Heterogeneity In Multifocal Prostate Cancer
1Department of Urology, Michigan Medicine, Ann Arbor, Michigan, USA.
2University of Michigan Rogel Cancer Center, Ann Arbor, Michigan, USA.
3Department of Pathology, Michigan Medicine, Ann Arbor, Michigan, USA.
4Department of Urology, Medical University Vienna, Vienna, Austria.
5Department of Urology, Rennes University Hospital, Rennes, France.
6Department of Radiology, Michigan Medicine, Ann Arbor, Michigan, USA.
7Department of Pathology, Medical University Vienna, Vienna, Austria.
8Department of Pathology, Rennes University Hospital, Rennes, France.
9Department of Radiation Oncology, Michigan Medicine, Ann Arbor, Michigan, USA.
10Michigan Center for Translational Pathology, Ann Arbor, Michigan, USA.
11Department of Pathology and Laboratory Medicine, Weill Cornell Medicine, New York, USA.
12Department of BioMedical Research, University of Bern, Bern, Switzerland.
Address correspondence to: Ganesh S. Palapattu, Department of Urology, University of Michigan, 1500 E. Medical Center Drive, TC 3875/SPC 5330, Ann Arbor, Michigan 48109-5330, USA. Phone: 734.763.9269; Email: . Or to: Scott A. Tomlins, Department of Pathology, University of Michigan, 1500 E. Medical Center Drive, 7322 Cancer Center, SPC 5948, Ann Arbor, Michigan 48109-5948, USA. Phone: 734.764.1549; Email: .
SSS and DHH contributed equally to this work.
Find articles bySalami, S.in: |PubMed |
1Department of Urology, Michigan Medicine, Ann Arbor, Michigan, USA.
SSS and DHH contributed equally to this work.
Also Check: Can Bph Cause Constipation
Computer Simulations Suggest That Prostate Enlargement Due To Benign Prostatic Hyperplasia Mechanically Impedes Prostate Cancer Growth
See allHide authors and affiliations
Somatic Mutations Of Spop Foxa1 And Idh
Somatic point mutations in SPOP were found in six cancer samples from five foci in five patients. Eight samples from seven foci in six patients had point mutations in FOXA1. The same mutation in IDH1 was identified in two samples from one focus within a single patient . All mutations were validated by Sanger sequencing .
Read Also: Prostate Cancer Ruined My Marriage
Haematospermia With And Without Stone In Seminal Vesicles
On T2W images, seminal vesicles appear as high-intensity sac-like structures and can be easily differentiated from significantly lower signal intensity of periprostatic fat. On T1W images, this signal pattern is reversed, and seminal vesicles have lower signal intensity compared to periprostatic fat .
Haematospermia is the presence of blood in the seminal fluid. Normal appearances of the seminal vesicles are grape-like clusters with high T2 signal intensity of internal content and low T2 signal intensity of the wall. The size of normal seminal vesicles is highly variable. Given blood has intrinsic high T1 signal; this is on its own a benign and usually straightforward diagnosis to make. However, high T1 signal can also be seen in the seminal vesicles with no haematospermia due to proteinaceous content. Haematospermia is usually a benign and self-limiting condition commonly seen in young sexually active males but albeit invokes anxiety in the patient and referrer.
Fig. 1
Haematospermia Axial T1W image shows intrinsic T1 hyperintensity within the right seminal vesicle . b Axial T2W image shows corresponding T2 hypointensity in this region in keeping with blood products . c Coronal T2W and axial T2W images in a different patient show rounded low T2 signal intensity lesions, in the right seminal vesicle in and bilaterally in but larger in the right seminal vesicle, in keeping with stones
