Future Treatment Landscape In Nmcrpc
Regarding unmet needs in the treatment space, Berger said that guidance for prescribers on drug-drug interactions is lacking. There are a lot of medications patients are on, whether its antihypertensives, diabetes medications, or cardiovascular medications, especially the anticoagulants that may have some interactions with these medications. And the guidance, as far as what we can glean from the studies, is not always clear about whats safe and what may not be safe, he said.
Another consideration is whether nmCRPC will continue to be a disease state in the future, as next-generation imaging techniques become more prevalent in the treatment landscape and reveal metastasis in patients who would have been formerly considered nonmetastatic.
When you have a scan that can pick up an area of metastasis at 0.2 to 0.3 ng/mL, it may turn out that these patients are metastatic. All of these studies were done with conventional imaging, Berger said. The big question as far as this entire disease state is, will it still be a disease state 5 years from now?
Overall, Berger said clinicians shouldnt shy away from prescribing these medications to their patients, given their tolerability and ease of administration. I would not be afraid of these medications because you can easily add them into your clinical practice without a lot of trepidation, he said.
Remission And The Chance Of Recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having no evidence of disease or NED.
A remission can be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. Although there are treatments to help prevent a recurrence, such as hormonal therapy and radiation therapy, it is important to talk with your doctor about the possibility of the cancer returning. There are tools your doctor can use, called nomograms, to estimate someone’s risk of recurrence. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. Learn more about coping with the fear of recurrence.
In general, following surgery or radiation therapy, the PSA level in the blood usually drops. If the PSA level starts to rise again, it may be a sign that the cancer has come back. If the cancer returns after the original treatment, it is called recurrent cancer.
When this occurs, a new cycle of testing will begin again to learn as much as possible about the recurrence, including where the recurrence is located. The cancer may come back in the prostate , in the tissues or lymph nodes near the prostate , or in another part of the body, such as the bones, lungs, or liver . Sometimes the doctor cannot find a tumor even though the PSA level has increased. This is known as a PSA recurrence or biochemical recurrence.
Treatment Options For Non
Dr Aaron Berger discusses systemic therapy options, treatment selection and monitoring for patients with nonmetastatic castrate-resistant prostate cancer .
Audrey Sternberg: Hello and welcome to this CancerNetwork® OncView program titled, Recent Updates in Treatment of Nonmetastatic Castration-Resistant Prostate Cancer. Im Audrey Sternberg with CancerNetwork®. We have with us today Dr Aaron Berger from Associated Urological Specialists in Chicago, Illinois. Thank you for joining us today, Dr Berger.
Aaron Berger, MD: Thank you. Its a pleasure to be here.
Audrey Sternberg: Lets get started. When youre treating a patient with nonmetastatic castration-resistant prostate cancer, what systemic therapy options are available?
Aaron Berger, MD: Over the last few years, several new options for nonmetastatic castration-resistant prostate cancer have come to market. The first was enzalutamide, or Xtandi, followed shortly thereafter by Erleada, or apalutamide, and then most recently was Nubeqa, or darolutamide. Weve used all of them in our advanced prostate cancer clinic. Its certainly much improved over the previous options that were available as far as first-generation antiandrogen therapies, in which the most recent one was introduced in 1995. There was a long gap in new treatments for this disease state.
This transcript has been edited for clarity.
Related Content:
Recommended Reading: Brca Testing For Prostate Cancer
Early Versus Delayed Treatment
For men who need hormone therapy, such as men whose PSA levels are rising after surgery or radiation or men with advanced prostate cancer who dont yet have symptoms, its not always clear when it is best to start hormone treatment. Some doctors think that hormone therapy works better if its started as soon as possible, even if a man feels well and is not having any symptoms. Some studies have shown that hormone treatment may slow the disease down and perhaps even help men live longer.
But not all doctors agree with this approach. Some are waiting for more evidence of benefit. They feel that because of the side effects of hormone therapy and the chance that the cancer could become resistant to therapy sooner, treatment shouldnt be started until a man has symptoms from the cancer. This issue is being studied.
More Options Lead To More Questions
Elisabeth Heath, M.D., director of prostate cancer research at Karmanos Cancer Institute in Detroit, agreed that the ARASENS results should have an immediate impact on how this form of the disease is treated.
Speaking at the ASCO symposium, Dr. Heath, who was not involved in the study, highlighted an important difference between ARASENS and other trials that tested androgen receptorblocking drugs in men with this form of prostate cancer. In those other trials, she explained, some participants received docetaxel prior to treatment with the androgen receptorblocking drugs rather than at the same time.
Based on the ARASENS results, Dr. Heath said, giving all three treatments simultaneously looks to be the preferred option for some patients.
Dr. Karzai noted that despite there being multiple options to treat metastatic hormone-sensitive prostate cancer, many questions remain. We don’t have guidelines on who should start with what drug and whether one drug is better than another for a patient, she said.
She also pointed out that more research is needed on how the order in which the drugs are given impact their effectiveness and the frequency of side effects.
Additionally, she said, the survival improvement in the ARASENS trial was seen in patients whose cancer had spread in multiple areas beyond the prostate .
We dont know if people with lower-volume benefit from as much as the patients with higher-volume disease do, she said.
Read Also: Best Test To Detect Prostate Cancer
Prognostic Assessment: Is Psadt Enough
Prostate-specific antigen doubling time has been considered a prognostic marker in retrospective studies, but that has been difficult to validate in prospective assessments . The optimal time interval between PSA values for estimating PSADT and its optimal limits still need to be determined.
In the case of M0 CRPC, PSA indirectly monitors tumor activity from the androgen receptor signal, which can correlate with tumor growth. However, it should be noted that PSA decline has not been proven to be a marker of survival or outcome, and androgen receptor downregulation does not always represent tumor cell elimination. In fact, it is acknowledged that some aggressive prostate cancers are low PSA secretors .
Recent studies have shown that PSA levels and PSADT are important tools in prognostic risk assessment in prostate cancer. Baseline PSA level, PSA velocity, and PSADT have been associated with the time to bone metastases, metastasis-free survival , and overall survival in M0 CRPC . However, while PSA levels are clearly defined through testing, a PSADT calculation can be less straightforward.
Bone Protection In Patients Receiving Androgen Blockade
Two drugs, the bisphosphonate zoledronic acid and the RANKL inhibitor denosumab, have been approved to treat osteoporosis secondary to androgen deprivation. Zoledronic acid is administered as an intravenous infusion. Denosumab is administered subcutaneously. These drugs are given along with supplemental vitamin D and calcium. Patients should be monitored regularly for hypocalcemia. Both agents are associated with a low incidence of osteonecrosis of the jaw. Both drugs delay the risk of skeletally-related events by relieving bone pain, preventing fractures, decreasing the need for surgery and radiation to the bones, and lowering the risk of spinal cord compression.
A double-blind, placebo-controlled, multicenter study in men with primary or hypogonadism-associated osteoporosis found that over a 14-month period, treatment with zoledronic acid reduced the risk of vertebral fractures by 67%. New morphometric vertebral fracture occurred in 1.6% of men taking zoledronic acid and in 4.9% taking placebo. Patients receiving zoledronic acid had significantly higher bone mineral density and lower bone-turnover markers. However, the rate of myocardial infarction was higher in the treatment group .
Don’t Miss: What Causes Psa Levels To Go Up After Prostate Removal
Special Situations And Drug Interactions
It is of vital importance to identify and differentiate the unalike clinical situations that we may encounter in our healthcare practice based on the baseline characteristics of the patients. Although we know that the chronological age does not always correspond to the real age of the patient, the tolerance in the elderly may differ from that of younger patients, with different metabolisms. In the same manner, it is important to take into account those patients with significant comorbidity or those who are polymedicated, in which certain nuances must be taken into account when prescribing these treatments .
Maintaining Quality Of Life In Patients With Nmcrpc
The patient with a rising PSA level and no radiologic evidence of metastases is usually asymptomatic from his disease but may exhibit symptoms related to age, chronic, nonmalignant comorbidities, long-term concomitant medications, adverse effects associated with ADT, and drugdrug interactions. Consequently, a consistent goal of initiating pharmacotherapy in nmCRPC should be to delay time to metastases while preserving quality of life as close to pretreatment status as possible .
Second-generation ARIs prolong survival while maintaining HRQoL in patients with nmCRPC. In clinical trials of the three approved ARIs, patient-reported outcomes captured by validated, self-administered questionnaires indicated that no treatment-induced deterioration in quality of life occurred, and that in some instances, improvement was observed in prostate cancer-specific domains .
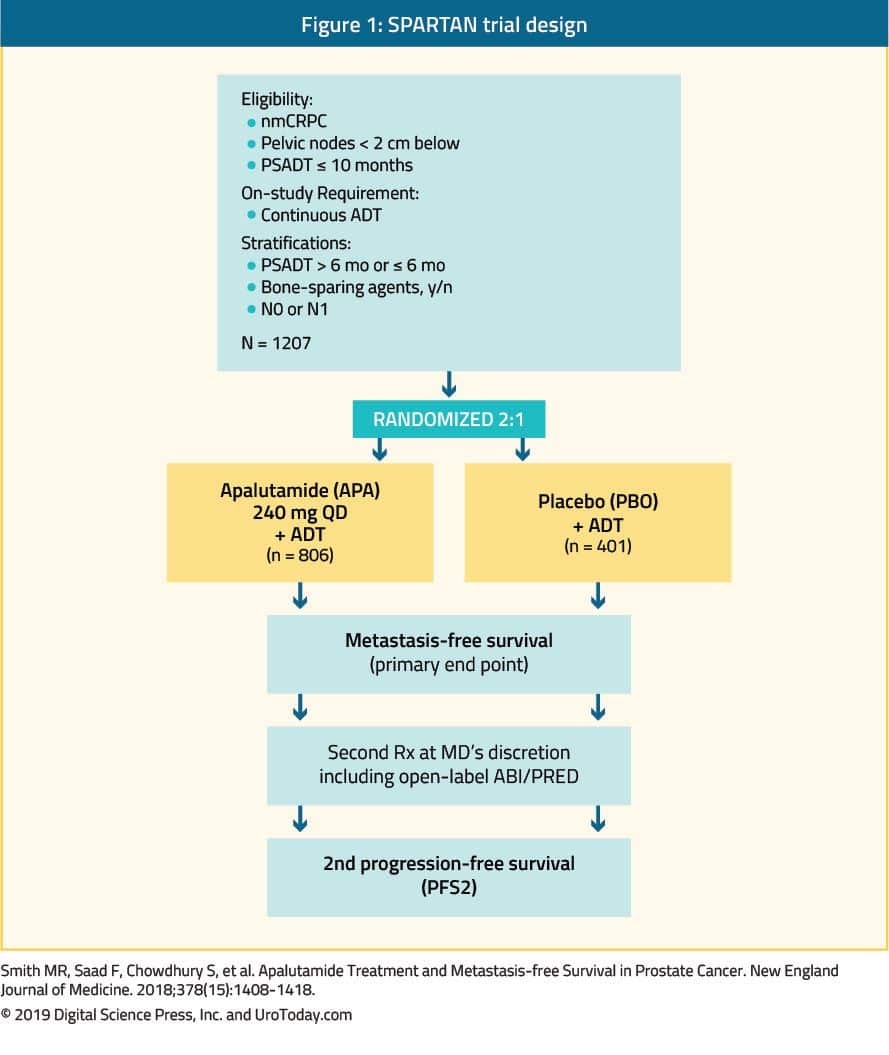
In the SPARTAN trial, the least-squares mean change from baseline showed that HRQoL deterioration was more apparent with placebo compared with apalutamide . In PROSPER, a trend favoring enzalutamide was observed for all domains of the Functional Assessment of Cancer Therapy-Prostate, with the exception of physical well-being . In ARAMIS, time to deterioration of European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire-Prostate Cancer Module outcomes demonstrated statistically and clinically significant delays with darolutamide versus placebo for urinary symptoms .
Don’t Miss: What Is The Purpose Of The Prostate
Ethics Approval And Consent To Participate
The protocol and study materials were reviewed and approved by the Salus Institutional Review Board . All respondents in the qualitative interviews provided written informed consent prior to participating in the interviews. All respondents in the survey provided electronic agreement after reviewing the informed consent form electronically.
Treatment Options For Patients With Nmcrpc
In addition to apalutamide, two other novel AR-targeted therapies enzalutamide and darolutamide were evaluated in nmCRPC and are briefly discussed here.
Recent updated analysis showed that darolutamide significantly delayed pain progression as compared to placebo . The delay in pain progression with darolutamide was maintained beyond end of the study treatment. Darolutamide was associated with delayed time to deterioration of EORTC-QLQ-PR25 outcomes for urinary symptoms and for hormonal treatment-related symptoms as compared to placebo .56
Read Also: What Does Prostate Cancer Mean
Safety Evaluation Of Toxicity
Toxicity was defined according to the NCI Common Toxicity Criteria. Treatment would be stopped for a patient with grade 3â4 toxicity. At that point, patients would be followed weekly until â¤grade 1 and then reinitiate treatment. Therapy would be stopped upon the recurrence of grade 3/4 events and for any toxicity requiring more than four weeks to recover to â¤grade 1.
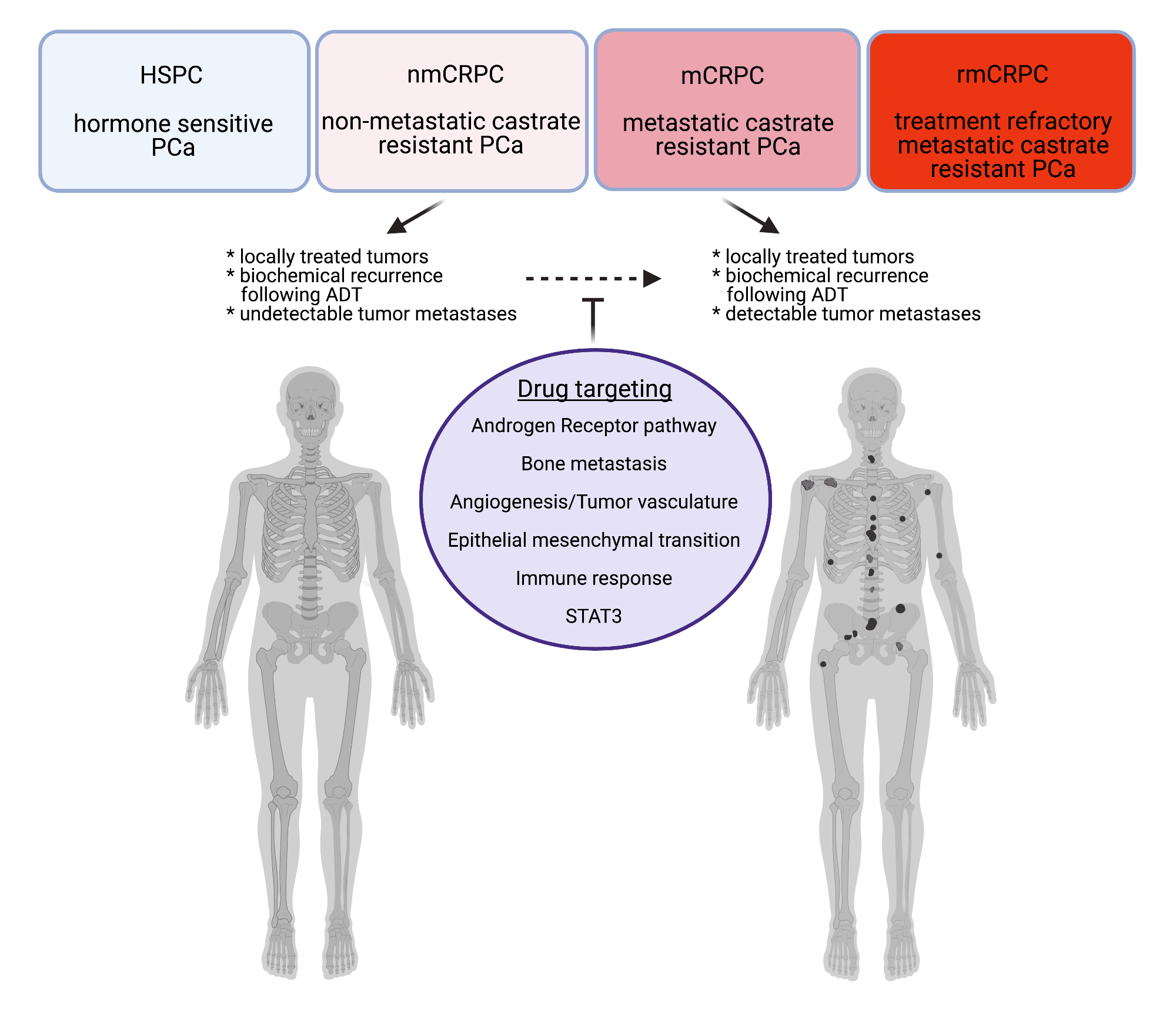
Castrate Resistant Prostate Cancer
Eventually, almost all metastatic prostate cancers become resistant to androgen ablation. In patients with castrate serum testosterone levels , castrate-resistant prostate cancer is defined as 2-3 consecutive rises in PSA levels obtained at intervals of greater than 2 weeks and/or documented disease progression based on findings from computed tomography scan and/or bone scan, bone pain, or obstructive voiding symptoms.
Rarely, a rise in PSA may reflect failure of LHRH treatment to control testosterone secretion, rather than the development of castrate-resistant disease. Therefore, the testosterone level should be measured when the PSA rises. If the serum testosterone level exceeds castrate levels, changing the antiandrogen therapy may drop the PSA and delay the need for other therapy.
Prior to the development of the most recent therapies, the median time to symptomatic progression after a rise in the PSA level of more than 4 ng/mL was approximately 6-8 months, with a median time to death of 12-18 months. Since then, however, the latter figure has increased.
Little information is available about the impact of maintaining hormone suppression when androgen-independent progression occurs, but the general consensus among specialists is that the treatment should continue. The reasoning is that tumor cells are still hormone sensitive and may grow faster if the testosterone is permitted to rise.
Docetaxel
You May Like: How Long Do Side Effects Of Prostate Radiation Last
How Will I Know If I Have Nonmetastatic Castration
Most cases of prostate cancer that are not cured with surgery or radiation will eventually become resistant to the effects of hormone therapy. If this happens, your PSA level might start to rise. A rising PSA level could mean that the cancer is progressing.
Your PSA can be measured with a simple blood test. Your doctor will likely test your PSA level periodically while you are receiving hormone therapy to gauge how well you are responding to it.
A widely accepted definition for rising PSA levels is a 25 percent increase from the lowest point, with a minimum surge of 2 nanograms per milliliter. This rise must be confirmed one to three weeks later.
If your PSA level is rising, your doctor will order scans to see if there is evidence that the prostate cancer has spread somewhere else in your body.
RELATED: 5 Ways to Boost Your Quality of Life During Prostate Cancer Treatment
Toxicity And Disease Status At Follow
Patients were evaluated for toxicities, physical exams, serum PSA, testosterone, CRP, and galectin-3 levels. Complete assessments of disease status included positron emission tomography PETâPSMA scan after six months in patients without clinical or PSA progression or earlier upon clinical or PSA progression.
Also Check: Hot Flashes After Hormone Therapy For Prostate Cancer
Clinical Development Of Apalutamide: Phase I Ii And Iii Data
A total of 1207 patients were randomized in 2:1 fashion to receive apalutamide 240 mg daily or placebo and ADT was continued in both arms during the study. The patients were stratified by PSA-DT , use of bone-sparing agents and classification of nodal status as N0 or N1. The median age of the patients was 74 years , 71.3% had a PSA-DT 6 months, 10.0% used a bone-sparing agent, and 83.6% had N0 nodal status. Most of the patients had previously used a first-generation AR antagonist. At the planned primary analysis, apalutamide demonstrated significant improvement in MFS compared with placebo . Similarly, median PFS was 40.5 months in the apalutamide arm vs 14.7 months in the placebo arm . Of the other exploratory endpoints, apalutamide was associated with improved TTPP , time to symptomatic progression , and time to initiation of cytotoxic chemotherapy . PSA response rate was observed in 90% of patients in the apalutamide group as compared to 2% in the placebo group. The patients in the apalutamide arm reported stable overall health-related QoL as did the patients in the placebo arm. The second PFS was significantly longer in the apalutamide arm than the placebo arm . Of note, the OS data were not mature at the time of publication but apalutamide showed a trend toward improved OS with HR of 0.70. Notably, an exploratory landmark analysis in the SPARTAN trial suggested an association between MFS and OS in high-risk nmCRPC who develop metastases at 6, 9, and 12 months .39
Radiation Therapy Versus Surgery
In 2014, the Agency for Healthcare Research and Quality found insufficient evidence to determine whether any type of radiation therapy results in fewer deaths or cancer recurrences than radical prostatectomy does in patients with clinically localized prostate cancer. The importance of dose escalation in disease control complicates the extraction of meaningful conclusions from current radiation therapy treatments .
Brachytherapy has also been compared with surgery in the management of early-stage disease. Direct comparisons are not readily available, but preliminary data from most centers suggest that permanent prostate implants yield comparable local control and biochemical disease-free rates.
Valid comparisons of surgery and radiation therapy are impossible without data from randomized studies that track long-term survival rather than PSA recurrence. Variation in radiation techniques and dosage administered the variable use of androgen ablation, which improves survival in intermediate- and high-risk disease and the variable impact on the quality of life complicate comparison using uncontrolled studies.
Also Check: Does Radiation Therapy Cure Prostate Cancer
If Treatment Does Not Work
Recovery from cancer is not always possible. If the cancer cannot be cured or controlled, the disease may be called advanced or terminal.
This diagnosis is stressful, and for some people, advanced cancer may be difficult to discuss. However, it is important to have open and honest conversations with your health care team to express your feelings, preferences, and concerns. The health care team has special skills, experience, and knowledge to support patients and their families and is there to help. Making sure a person is physically comfortable, free from pain, and emotionally supported is extremely important.
People who have advanced cancer and who are expected to live less than 6 months may want to consider hospice care. Hospice care is designed to provide the best possible quality of life for people who are near the end of life. You and your family are encouraged to talk with the health care team about hospice care options, which include hospice care at home, a special hospice center, or other health care locations. Nursing care and special equipment, including a hospital bed, can make staying at home a workable option for many families. Learn more about advanced cancer care planning.
After the death of a loved one, many people need support to help them cope with the loss. Learn more about grief and loss.
