What Will The Patient Experience After Surgery
We usually take our patients to our intensive care unit immediately after surgery and follow them there for about 6-8 hours. Then we take the patient to his single room in the service. After coming to the patients room, the patient starts taking nourishment orally.
If the bowel sounds of the patient can be heard on the morning of the 1st postoperative day, the patient begins to consume fluid foods. If the patient has pain, painkillers are administered . We ask patients not to walk around as much as possible.
Patients usually switch to normal eating on that day. On the 2nd postoperative day, the drain of the patient is removed and he is discharged if there are no complications.
Recommended Reading: Best Supplement For Enlarged Prostate
Risks Of The Procedure
As with any surgical procedure, certain complications can occur. Somepossible complications of both the retropubic and perineal approaches to RPmay include:
Some risks associated with surgery and anesthesia in general include:
-
Reactions to medications, such as anesthesia
-
Difficulty with breathing
One risk associated with the retropubic approach is the potential forrectal injury, causing fecal incontinence or urgency.
There may be other risks depending on your specific medical condition. Besure to discuss any concerns with your doctor prior to the procedure.
What Are The Advantages Of Laparoscopy
As is the case with other minimally invasive procedures, laparoscopic prostate removal has significant advantages over traditional surgery:
- Laparoscopy can shorten your hospital stay to 1 or 2 days. About 50% of men are discharged one day after surgery.
- There is much less bleeding during the operation.
- You are less likely to need prescription painkillers after you leave the hospital. Patients often need nothing more than Tylenol.
- At your follow-up appointment 1 week after surgery, the tube, or catheter, draining your bladder will be removed if there are no signs of other problems. Occasionally, the catheter remains in place for another week, as with conventional surgery.
- About 90% of patients can return to work or resume full activity in only 2 to 3 weeks.
You May Like: Can You Beat Stage 4 Prostate Cancer
Prostate Surgery Complications And Risks
Surgery is an inherently risky medical procedure. However, for prostate cancer treatment, surgery can be the most effective choice for eradicating malignant tumors without the painful side effects of chemotherapy and radiation therapy.
Among the more serious risks associated with surgical treatment is the possibility of infection at the incision site. Such infections are often the primary cause of serious complications which may hamper a quick and uneventful recovery.
The da Vinci system greatly mitigates the risk of infection during robotic prostate surgery.
First, the size of the incision is significantly smaller with robotic prostate surgery than with the traditional procedure. A standard, non-robotic prostate surgery requires a six- to eight-inch vertical incision to the abdomen. A large, open incision increases the patients susceptibility to bacterial infection during and after the surgery.
Post-operative infections are more common than intra-operative infections, as hospital rooms are not maintained at the same level of sterility in which operating rooms are. The da Vinci robotic prostate surgery system utilizes a much less invasive technique requiring four to five small incisions, each less than two inches.
These smaller incisions will heal significantly faster than the large incision needed in traditional surgery.
Other prostate surgery complications may be:
What Types Of Surgery Are There
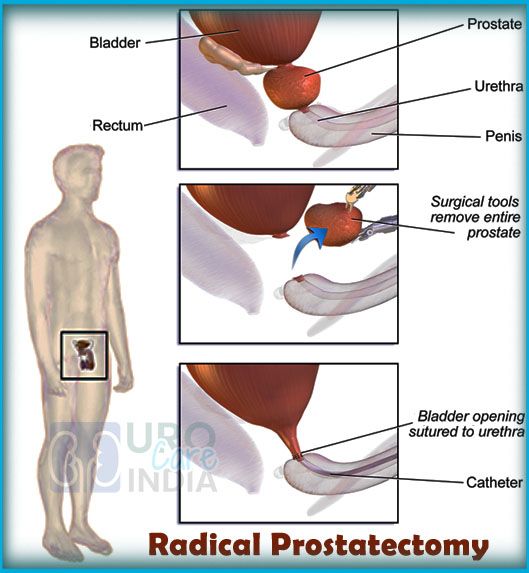
Radical prostatectomy involves removing the prostate, part of the urethra and the seminal vesicles. After the prostate is removed, the urethra will be rejoined to the bladder and the vas deferens will be sealed.
Some people are able to have nerve-sparing surgery, which aims to avoid damaging the nerves that control erections. Your doctor will discuss whether this is an option for you. Nerve-sparing radical prostatectomy is more suitable for lower-grade cancers and is only possible if the cancer is not in or close to these nerves. It works best for those who had strong erections before diagnosis. Problems with erections are common even if nerve-sparing surgery is performed.
Cancer cells can spread from the prostate to nearby lymph nodes. For intermediate-risk or high-risk prostate cancer, nearby lymph nodes may also be removed .
Recommended Reading: What Is Scraping Of The Prostate
* Minimal Blood Loss With Da Vinci Robotic
The average estimated blood loss per patient averages 116 cc. This volume is roughly the 1/3 of the volume of a 12 oz. soda can. Estimated Blood loss has ranged for robotic patients from 25cc to a maximum of 400 cc in the 1st 100 patients. Because of these low blood losses, none of these men required a blood transfusion, nor were they asked to donate autologous blood prior to surgery.
What Is The Procedure
Laparoscopic radical prostatectomy is a surgical procedure whose main aim is to remove the prostate and other adjacent organs.
During surgery, the prostate, seminal vesicles and part of the ductus deferens are removed.
The patient is put under general anaesthetic. The surgeon inserts instruments through the abdominal wall via very small incisions rather than the longer incision used in open surgery.
A microscopic video camera on one of the instruments films the inside of the patients body and is used by the medial team performing the surgery.
Like any operation, there are risks associated with this medical procedure, such as:
- Complications, like allergic reactions, related to the anaesthetic
- Adjacent organ lesions
However, keyhole surgery is much less invasive and aggressive compared to other more radical treatments, such as classical open surgery.
After the operation, patients sometimes complain about urinary incontinence and erectile dysfunction. Normally, these gradually wane over time. If they persist, it is important to discuss the symptoms with the doctor following the case or at specialist centres treating prostate cancer and its consequences.
Also Check: How Long Does Erectile Dysfunction Last After Prostate Surgery
Msks Approach To Radical Prostatectomy
Our prostate surgery team includes experts in several techniques, including robot-assisted surgery, open surgery, and laparoscopic surgery. Regardless of which surgical approach you choose, our goal is to remove your cancer completely and preserve normal urinary and sexual function.
With all surgical approaches, weve developed and use innovative techniques to preserve the tiny nerves and blood vessels attached to the prostate that help control erections. These and other advances have made some of the complications of prostate cancer surgery less common and more manageable and can spare nerves from damage. Well work closely with you and your medical team to manage any short- or long-term side effects you may experience.
Ultimately, youll help determine which approach your surgeon takes.
Indications For Laparoscopic Surgery
The treatment is suitable for the same situations as classical open surgery, with no limits in terms of prostate volume, PSA or Gleason grading .
The inclusion criteria are the same as other curative techniques. This technique should be considered for patients with clinically localised tumours or, in some cases, locally advanced tumours .
The PSA level and Gleason grading are important prognostic indicators that should be incorporated into instruments like the classic Partin tables tools used to ascertain a patients likelihood of having a localised, locally advanced or advanced tumour.
This data, together with information obtained from a digital rectal exam, details such as the patients age, additional test results and even new tumour markers, allow assessment of the probability of a localised tumour at a more advanced stage and calculation of the risk of curing the illness or its evolution or recurrence.
Various prognostic indicators are available and accessible online that can be used for this purpose relatively simply.
Want to know more about laparoscopic surgery?
Recommended Reading: What Is The Normal Level For Prostate
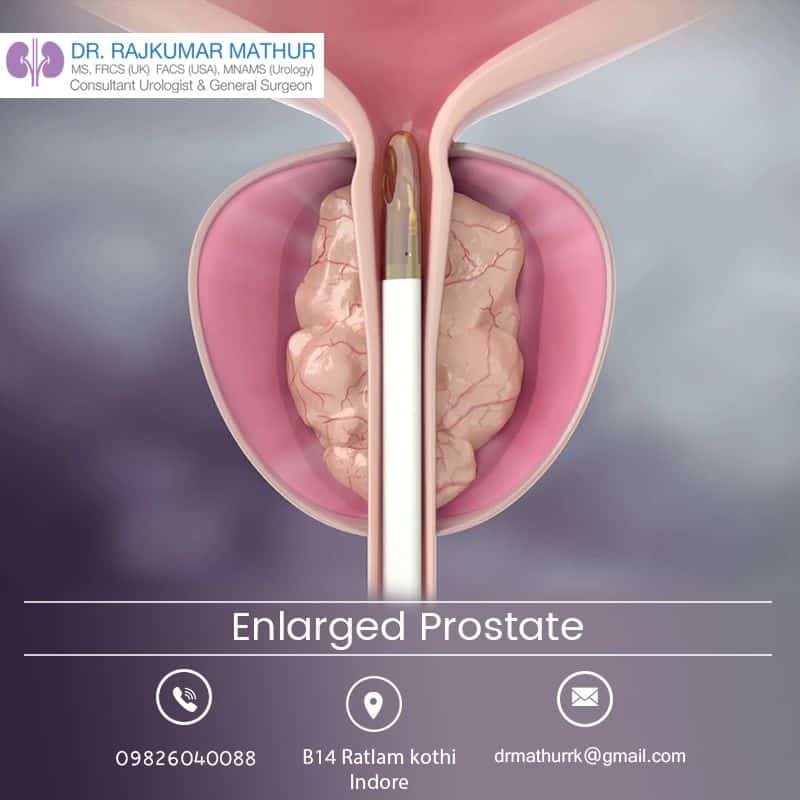
Transurethral Resection Of The Prostate
In most cases, doctors use this procedure to help people with something called benign prostatic hyperplasia , an enlargement of the prostate that isn’t cancer.
People with prostate cancer have TURP done to ease symptoms like trouble peeing. Doctors don’t use this surgery to try to cure the cancer.
A surgeon removes the inner portion of your prostate gland that surrounds something called the urethra. That’s the tube where the urine leaves your bladder. Then they’ll pass a tool called a resectoscope past the tip of your into the urethra. From there, they’ll either send electricity through a wire to heat the area up or use a laser to vaporize or cut tissue.
How Long Does Laparoscopic Prostatectomy Surgery Take
The time required to perform a laparoscopic radical prostatectomy can vary from between 2 hours 30 minutes and 3 hours 30 minutes depending on the anatomy of each individual, the size of the prostate and if it is required to remove other surrounding tissues.
Most patients can go home the day after the intervention, so the hospital stay is minimal, although rest at home is required. Two or three weeks are enough to return to daily activities completely. The treating physician will be in charge of indicating how much time is necessary based on the postoperative check-ups.
Another important factor is the placement of a catheter to urinate without straining the urethra after surgery.
With conventional techniques the catheter must remain inside the patients penile urethra for about two or three weeks since the degree of trauma to the tissues was greater.
However, with laparoscopic prostate surgery it is possible to remove the bladder catheter on the third day after the intervention.
Read Also: What Happens When A Man’s Prostate Is Removed
Quicker Recovery Period After Robotic Prostatectomy
When a physician determines robotic prostatectomy is the best prostate cancer treatment option, da Vincis robotic technology optimizes the chances of a quicker recovery time as opposed to traditional surgical prostatectomy. The smaller incisions required to maneuver the operating arms heal much faster require fewer sutures, and, therefore, are less vulnerable to tearing or infection.
The precise movements of the robotic arms allow a more targeted approach for cleaner removal of malignant tissue and reducing damage to healthy tissue during robotic prostate surgery. The operating arms of the da Vinci Surgical System are designed to avoid contact between the operating instruments and the walls of the incision. All of these advantages translate to a speedier and less worrisome recovery period.
Prostate surgery recovery time is substantially improved in comparison to open prostatectomy. As mentioned earlier, the much larger incision required in open surgery means pain is greater and recovery takes longer. Dr. Samadis prostate surgery takes just 1.5-2 hours and almost all of his patients return home the day after having a robotic prostatectomy. Around 80% of open prostatectomy patients leave the hospital within the first week.
What Are The Advantages Of This Procedure
Traditional surgery for tumor removal requires an eight-inch incision, at a minimum. The minimally invasive technique requires four or five tiny incisions for the surgical instruments. Laparoscopic prostatectomy offers surgeons unparalleled visualization of the pelvic area, thus permitting precise removal of the prostate. Patients also experience significantly less blood loss.
- Additionally, patients benefit from:
- Reduced hospital stay and faster healing
- Less postoperative pain
- Quicker return to normal activity and work
- Smaller incisions and less scarring
Don’t Miss: What Is The Best Prostate Massager
Patient Positioning And Abdominal Access
Regardless of the technique used, the patient is placed in the supine position with the head down. This head-down position allows for gravity to facilitate the natural retraction of the pelvic tissues. If the procedure is to be performed transperitoneally, a periumbilical incision is made to provide access for the initial laparoscopic port. A Veress needle or Hasson-type trocar is used to establish pneumoperitoneum and to facilitate the laparoscopic survey of the abdomen. The Veress needle is an ideal access device when the patient has no history of abdominal surgery. In patients who have undergone previous abdominal surgery, particularly involving infraumbilical incisions, the Hassan trocar is ideal for direct visualization and confirmation of entrance into the peritoneal cavity.
Carbon dioxide is then insufflated into the abdomen to achieve pneumoperitoneum. If a Veress needle was used for initial access, it is replaced by a 12-mm radially dilating laparoscopic trocar. The 3-dimensional robotic laparoscope is then inserted through the infraumbilical trocar site, and a laparoscopic survey of the abdomen and pelvis is performed. If the procedure is to be performed extraperitoneally, the first steps for access consist of a small incision and development of the extraperitoneal space.
When You Might Have A Radical Prostatectomy
Your doctor might recommend a radical prostatectomy if:
- your cancer hasn’t spread outside the prostate gland. This is localised prostate cancer
- your cancer has broken through the covering of the prostate and spread to the area just outside the prostate gland. This is locally advanced prostate cancer
- you are well enough to have this operation
The aim of a radical prostatectomy operation is to cure prostate cancer.
Read Also: Can Enlarged Prostate Cause Blood In Urine
Robotic Radical Prostatectomy Versus Laparoscopic Or Open Surgery
Robotic radical prostatectomy offers significantly lower operative times and blood loss than laparoscopic or open surgery. Catheterization times and hospital stay are also superior to those associated with open and laparoscopic approaches. The learning curve is less with robotic assistance compared with laparoscopy. The one significant question that remains unanswered pertains to the cost-effectiveness of robotic prostatectomy compared with open and laparoscopic radical prostatectomy.
A randomized controlled phase 3 study by Yaxley et al that compared robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy reported that both techniques had similar functional outcomes at 12 weeks. Urinary function scores and sexual function scores were not significantly different between these two groups at 6- and 12-weeks post-surgery.
Early functional results are are summarized in Table 4 below.
Table 4. Outcomes of Functional Parameters Using Robotic Radical Prostatectomy
|
Series |
|
|
Badani et al |
2766 |
|
Ahlering et al |
|
|
96% at 6 mo |
|
|
IIEF = International Index of Erectile Function. |
Preliminary results from the above series show that oncologic and functional results following robotic prostatectomy compare very favorably with those of either open or laparoscopic radical prostatectomy. The margin rates and rates of prostate-specific antigen recurrence are similar, but potency and continence rates are better than those of open and laparoscopic approaches.
Procedure And Technique: What Is Laparoscopic Prostate Surgery
Previous preparation
Before surgery, the surgeon performs a series of consultations to examine the patient and order imaging studies such as MRIs and ultrasound of the pelvic region. This is used to assess the condition of the prostate and anticipate what the surgery will be like. Some blood tests are also indicated to determine blood chemistry through a complete blood count.
Depending on the patient and their previous pathologies , the doctor may also order an electrocardiogram or a pulmonary function test to assess the patients health status.
In addition to this, it is also recommended that the patient modify some habits and lifestyles such as:
- Stop taking anticoagulant drugs such as aspirin or warfarin .
- Stop consuming pain relievers and non-steroidal anti-inflammatory drugs.
- Maintain a liquid or semi-liquid diet in the 24 hours prior to surgery to prepare the intestines and prevent diarrhea due to the effect of local anesthesia.
- After midnight the day before surgery, it is recommended to drink very little fluids. A few small sips of water will be enough to quench your thirst should it appear.
- Abstinence from alcohol, tobacco and any type of narcotic is probably also indicated. Quitting smoking is key to helping the body and the tissues manipulated in the surgery perceive better blood flow and oxygen supply to accelerate the recovery process.
How is anesthesia for surgery?
This pre-anesthetic evaluation also serves to rule out any hypersensitivity to it.
You May Like: Can You Milk Your Prostate
Caring For The Catheter
You will be discharged with a Foley catheter, a tube that continuously drains urine from your bladder into a bag and that you will use for seven to 10 days. Before you leave the hospital, your nurse will teach you how to empty and care for your catheter and drainage bag. The catheter works with gravity and should be draining urine at all times, so you have to keep the drainage bag below your bladder at all times, even when you shower. If your urine is not draining, lower the bag and check the connection for kinks or loops. Loops can cause an air lock that prevents drainage. You can also try emptying the bag. Then try briefly disconnecting the catheter from the clear plastic tubing to allow a little air into the system. Your nurse will show you how to do this before your discharge.
To prevent infection, you must keep your catheter clean. This section explains how to clean the catheter, the area around the catheter and the drainage bag. It also explains how to apply your leg bag and secure the catheter to your leg.
We will provide most of the supplies you need to care for your catheter. They include:
- StatLock Foley catheter securement device
- Shaving supplies
You should empty the catheter bag when it’s half full. This helps prevent air locks from developing in the tubing.
To apply the leg bag:
Looking For Prices And Information
Use our virtual assistant and receive in your email everything related to the treatments that interest you. Budgets, recovery times, hospitalization, financing possibilities month by month, etc.
In just a few minutes and without any commitment.
En cumplimiento del Reglamento General de Protección de Datos le informamos que los datos por Vd. proporcionados serán objeto de tratamiento por parte de Andromedi con la finalidad de prestarle el servicio solicitado y/o contratado. Los datos no se cederán a terceros salvo en los casos en que exista una obligación legal. Para más información puede consultarla pinchando aquí.
Don’t Miss: How Often Should You Test For Prostate Cancer
