How Does Hormone Therapy Work Against Prostate Cancer
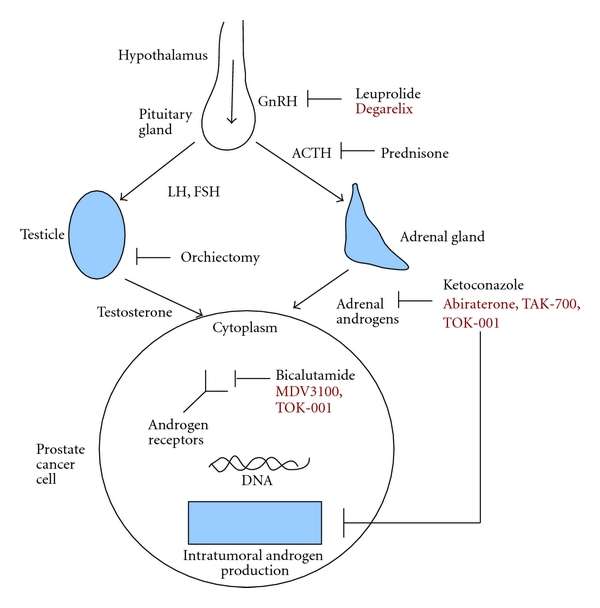
Early in their development, prostate cancers need androgens to grow. Hormone therapies, which are treatments that decrease androgen levels or block androgen action, can inhibit the growth of such prostate cancers, which are therefore called castration sensitive, androgen dependent, or androgen sensitive.
Most prostate cancers eventually stop responding to hormone therapy and become castration resistant. That is, they continue to grow even when androgen levels in the body are extremely low or undetectable. In the past, these tumors were also called hormone resistant, androgen independent, or hormone refractory however, these terms are rarely used now because the tumors are not truly independent of androgens for their growth. In fact, some newer hormone therapies have become available that can be used to treat tumors that have become castration resistant.
Improving How Long Patients Live
The ENZAMET trialfunded in part by the drugs manufacturer, Astellas Pharma, as well as government health agencies in Canada and Australiaenrolled more than 1,100 men with hormone-sensitive metastatic prostate cancer. The men were randomly assigned to ADT combined with enzalutamide or with any of three other androgen-blocking drugs.
At a median follow-up of nearly 3 years, men who received ADT plus enzalutamide had a 33% reduced risk of death, with 80% still alive compared with 72% of men treated with ADT plus another antiandrogen drug, reported the trials lead investigator, Christopher Sweeney, M.B.B.S., of the Dana-Farber Cancer Institute.
Men in the enzalutamide group also had better clinical progression-free survival , which the research team defined as the time until the return of disease-related symptoms, the detection of new metastases on imaging scans, or the initiation of another cancer treatment for prostate cancer, whichever came first. At 3 years, 63% of men in the enzalutamide group were alive without clinical progression of their disease, compared with 33% in the standard treatment group.
Although enzalutamide appeared to be effective regardless of whether men had high- or low-volume disease, one apparent differentiating factor was planned early treatment with docetaxel. Nearly half of the men in both treatment groups received early treatment with docetaxel and, for those men, enzalutamide was not associated with longer overall survival.
How Do I Know If My Cancer Is Hormone
Your doctor can find out by testing your cancerâs cells. Theyâll take a small piece of your tumor, called a biopsy. It goes to a lab for testing. The lab technician will use a microscope to look at the cells in the sample. If they see a lot of receptors on them, that means your tumor is hormone-sensitive.
Don’t Miss: Can Prostatitis Affect Bowel Movements
Is Triple Therapy The New Standard For Metastatic Hormone
touchREVIEWS in Oncology & Haematology
Abstract:
Overview
The treatment of metastatic hormone-sensitive prostate cancer has rapidly changed over the last decade. Currently, standard of care options for first-line treatment are androgen deprivation therapy in combination with either docetaxel chemotherapy or an androgen receptor pathway inhibitor such as abiraterone, enzalutamide or apalutamide. Recent results from both the PEACE-1 and ARASENS trials show an overall survival and progression-free survival benefit from the addition of an androgen-receptor pathway inhibitor for patients in whom the SOC option of ADT plus docetaxel has been chosen in de novo metastatic hormone-sensitive prostate cancer, with a more pronounced benefit in those with high-volume metastatic disease. However, many clinicians now preferentially use ADT plus an androgen-receptor pathway inhibitor as SOC first-line treatment, and no prospective trial has addressed whether there is a benefit from the addition of docetaxel to this version of SOC combination therapy. The benefit of triplet combination therapy in those with recurrent or low-volume metastatic disease is less clear and longer follow-up is required before conclusions can be drawn about these patient groups.
Keywords
Abiraterone acetate, apalutamide, darolutamide, docetaxel, enzalutamide, metastatic hormone-sensitive prostate cancer, triplet combination therapy
Article:
What Are Male Sex Hormones
Hormones are substances that are made by glands in the body. Hormones circulate in the bloodstream and control the actions of certain cells or organs.
Androgens are a class of hormones that control the development and maintenance of male characteristics. The most abundant androgens in men are testosterone and dihydrotestosterone .
Androgens are required for normal growth and function of the prostate, a gland in the male reproductive system that helps make semen. Androgens are also necessary for prostate cancers to grow. Androgens promote the growth of both normal and cancerous prostate cells by binding to and activating the androgen receptor, a protein that is expressed in prostate cells . Once activated, the androgen receptor stimulates the expression of specific genes that cause prostate cells to grow .
Almost all testosterone is produced in the testicles a small amount is produced by the adrenal glands. Although prostate cells do not normally make testosterone, some prostate cancer cells acquire the ability to do so .
You May Like: Does Ejaculation Cause Prostate Inflammation
The Current Landscape Of Metastatic Hormone Sensitive Prostate Cancer: Treatment Utilization And Future Directions
Introduction
Comparison of Approved Agents in mHSPC space
BJU InternationalJAMA Oncology
Real-world Utilization of Novel Agents
Upcoming Trials
any
Key Factors Associated With Adt Alone Use: Adt Alone Vs Chemotherapy Or Nha
Examining the key clinical reasons for treatment choice revealed that physicians prescribed ADT alone vs chemotherapy to significantly higher proportions of patients with a poor performance status , who wanted to maintain/improve their QoL , who may have compliance challenges , who could not tolerate adverse events , or with bone only disease . The only significant difference between ADT alone vs NHA in terms of key clinical reasons for treatment choice was for treatment is suitable for patients who may have compliance challenges, with physicians prescribing ADT alone rather than NHA to a significantly higher proportion of patients . All key clinical reasons for treatment choice for ADT alone vs NHA or chemotherapy are presented in Fig. .
Also Check: Metastatic Castration Resistant Prostate Cancer Life Expectancy
When Is Hormone Therapy Used
Hormone therapy may be used:
- If the cancer has spread too far to be cured by surgery or radiation, or if you cant have these treatments for some other reason
- If the cancer remains or comes back after treatment with surgery or radiation therapy
- Along with radiation therapy as the initial treatment, if you are at higher risk of the cancer coming back after treatment
- Before radiation to try to shrink the cancer to make treatment more effective
The Role Of Surgery Radiotherapy And Ablation In Oligometastatic Prostate Cancer
The concept of oligometastatic prostate cancer is an evolving paradigm, principally as a result of the rapid advancement of diagnostic and molecular-imaging modalities. As imaging techniques have become more sensitive, the detection of previously occult prostate cancer raises the question of whether patients with low-volume metastatic disease should be treated with targeted therapy, observation, or systemic therapy, as described above. In men with mHSPC there are two related, but independent, questions: first, is there benefit with treatment of the primary tumor in patients with low volume metastatic disease and second, is there benefit with treatment of metastatic disease sites?
With regard to the first question, a SEER analysis of 8185 men diagnosed with metastatic prostate cancer from Culp et al found that definitive treatment of the prostate with radical prostatectomy or local radiation conferred a significant OS and DSS benefit .37 Men undergoing local treatment of the prostate also experienced fewer local symptoms and complications of disease progression.
SWOG 1802 is an ongoing study that sets out to compare OS, PFS, and rate of symptomatic local progression utilizing standard systemic therapy with or without local therapy in men with mHSPC.40 Randomized prospective trials such as this will better clarify the subset of patients who may benefit from local treatment in the face of metastatic disease.
Don’t Miss: My Husband Is Dying Of Prostate Cancer
Definitive Treatment Is Beneficial Only In Patients With Low
Not only systemic pharmacotherapy, but radiation to the prostate also improves OS in low-volume disease. The recent high-quality RCTs, STAMPEDE and Hormonal Therapy Versus Hormonal Therapy Plus Local External Radiation Therapy in Patients With Primary Diagnosed Metastasized Prostate Cancer , concluded that adding radiation therapy to the prostate in mCSPC patients receiving ADT did not further improve their OS, the primary endpoint. In contrast, subgroup analyses by metastatic burden in the STAMPEDE trial showed OS benefit for patients with low-volume disease . The HORRAD trial also showed a similar trend without statistical significance in patients with < 5 metastatic lesions. Meta-analysis of 2 RCTs that involved 2493 patients suggested that ADT plus EBRT to the prostate was associated with improved OS as compared to ADT alone in men with low-volume metastatic burden however, this result was not observed in those with high-volume disease . Prostatectomy may also improve the oncologic outcomes in patients with oligometastatic prostate cancer. The definitive treatments, either radiation or prostatectomy, may be associated with survival benefit in patients with low metastatic burden. The results of several ongoing clinical trials on the benefit of prostatectomy and radiation to the prostate are expected to provide more information on this subject.
Who Is A Candidate
Most men with advanced prostate cancer are candidates for hormone therapy. Its usually considered when prostate cancer has spread beyond the prostate, and surgery to remove the tumor is no longer possible.
Prior to starting treatment, youll need to have a liver function test along with a blood test to make sure your liver can break down the medications properly.
Currently, enzalutamide is only approved for use in men with prostate cancer that has already spread to other parts of the body, and who no longer respond to medical or surgical treatments to lower testosterone levels.
In some cases, prostate cancer cells can resist hormone treatments and multiply even in the absence of male hormones. This is called hormone-resistant prostate cancer. Men with hormone-resistant prostate cancer arent candidates for further hormone therapy.
Don’t Miss: Is Cayenne Pepper Good For Your Prostate
Ethics Approval And Consent To Participate
Data collection was undertaken in line with the European Pharmaceutical Marketing Research Association guidelines . The questionnaires used in the Prostate Cancer DSP were reviewed and given exemption by the Western Institutional Review Board . The survey was performed in full accordance with relevant legislation at the time of data collection, including the US Health Insurance Portability and Accountability Act 1996 and the Health Information Technology for Economic and Clinical Health Act legislation . Data were collected according to market research guidelines hence, no source validation was possible or required. Data were collected in such a way that patients and physicians could not be identified directly all data were aggregated, de-identified and anonymized before receipt by Adelphi Real World and therefore informed consent from individual patients was not required.
Orteronel Misses Goal In Metastatic Hormone
Significant improvement seen in progression-free survival, but not overall survival, with addition of orteronel to androgen deprivation therapy
- HealthDay
You’ve saved your first item
You can find your saved items on your dashboard, in the “saved” tab.
You’ve recommended your first item
Your recommendations help us improve our content suggestions for you and other PracticeUpdate members.
You’ve subscribed to your first topic alert
What does that mean?
Read Also: Is Fish Oil Linked To Prostate Cancer
Many Choices Now For Men With Metastatic Hormone
Based on the recently published ENZAMET, ARCHES, and TITAN trials,1-3 we now have several choices of systemic combination therapies for men with metastatic hormone-sensitive prostate cancer. Today, men are faced with decisions of androgen-deprivation therapy alone or combinations with abiraterone, docetaxel, enzalutamide, or apalutamide, and there are now additional complex decisions around triple combination or sequential therapy with induction androgen-deprivation therapy/docetaxel plus a potent androgen-receptor inhibitor or whether single-agent chemotherapy or androgen-receptor inhibitor use with androgen-deprivation therapy is sufficient. These decisions are presently based on costs, availability and approvals, disease risk/volume, patient age and comorbidity, and of course shared decision-making.
Andrew J. Armstrong, MD, ScM, FACP
Complexity of Treatment Decisions
In ENZAMET and the global phase III ARCHES trial, there are clear benefits overall with enzalutamide/androgen-deprivation therapy over androgen-deprivation therapy alone. There are also clearly significant improvements in overall survival, delays in clinical disease progression and radiographic progression-free survival, time to symptomatic skeletal events, and time to the need for further systemic therapy with enzalutamide use early. These results are similar with apalutamide in the TITAN trial.
What About Androgen-Deprivation Therapy Alone?
Selecting Treatments Based on More Than Efficacy Alone
REFERENCES
How Prostate Cancer Is Treated
In cancer care, different types of doctorsincluding medical oncologists, surgeons, and radiation oncologistsoften work together to create an overall treatment plan that may combine different types of treatments to treat the cancer. This is called a multidisciplinary team. Cancer care teams include a variety of other health care professionals, such as palliative care experts, physician assistants, nurse practitioners, oncology nurses, social workers, pharmacists, counselors, dietitians, physical therapists, and others.
The common types of treatments used for prostate cancer are described below. Your care plan may also include treatment for symptoms and side effects, an important part of cancer care.
Treatment options and recommendations depend on several factors, including the type and stage of cancer, possible side effects, and the patients preferences and overall health.
Cancer treatment can affect older adults in different ways. More information on the specific effects of surgery, chemotherapy, and radiation therapy on older patients can be found another section of this website.
Because most prostate cancers are found in the early stages when they are growing slowly, you usually do not have to rush to make treatment decisions. During this time, it is important to talk with your doctor about the risks and benefits of all your treatment options and when treatment should begin. This discussion should also address the current state of the cancer:
Also Check: How To Hit The Prostate
Drugs That Stop Androgens From Working
Anti-androgens
For most prostate cancer cells to grow, androgens have to attach to a protein in the prostate cancer cell called an androgen receptor. Anti-androgens are drugs that also connect to these receptors, keeping the androgens from causing tumor growth. Anti-androgens are also sometimes called androgen receptor antagonists.
Drugs of this type include:
- Flutamide
They are taken daily as pills.
In the United States, anti-androgens are not often used by themselves:
- An anti-androgen may be added to treatment if orchiectomy or an LHRH agonist or antagonist is no longer working by itself.
- An anti-androgen is also sometimes given for a few weeks when an LHRH agonist is first started. This can help prevent a tumor flare.
- An anti-androgen can also be combined with orchiectomy or an LHRH agonist as first-line hormone therapy. This is called combined androgen blockade . There is still some debate as to whether CAB is more effective in this setting than using orchiectomy or an LHRH agonist alone. If there is a benefit, it appears to be small.
- In some men, if an anti-androgen is no longer working, simply stopping the anti-androgen can cause the cancer to stop growing for a short time. This is called the anti-androgen withdrawal effect, although it is not clear why it happens.
Newer anti-androgens
Enzalutamide , apalutamide and darolutamide are newer types of anti-androgens.
These drugs are taken as pills each day.
Hormone Sensitive Prostate Cancer Market Overview
Prostate cancer is a general term used for diseased condition in which abnormal cells grow and invade in uncontrolled manner in the prostate. Prostate cancer inhibits production of male sex hormones and ultimately blocks the action of androgen. The androgen is also responsible for the growth of prostate cancer.
Androgen binds with the receptors and stimulates the expression of specific genes that would be responsible for prostate cancer. However, androgen suppression hormonal therapies are commonly used for the treatment of this cancer. These therapies acts by reducing the production of androgen by the testicles or by blocking the action of androgen in the body.
There is an opportunity for the growth of hormone sensitive prostate cancer owing to the rapidly aging population which is the major cause of prostate cancer.
Don’t Miss: What Is The Male Prostate
Intermittent Versus Continuous Hormone Therapy
Most prostate cancers treated with hormone therapy become resistant to this treatment over a period of months or years. Some doctors believe that constant androgen suppression might not be needed, so they advise intermittent treatment. This can allow for a break from side effects like decreased energy, sexual problems, and hot flashes.
In one form of intermittent hormone therapy, treatment is stopped once the PSA drops to a very low level. If the PSA level begins to rise, the drugs are started again. Another form of intermittent therapy uses hormone therapy for fixed periods of time for example, 6 months on followed by 6 months off.
At this time, it isnt clear how this approach compares to continuous hormone therapy. Some studies have found that continuous therapy might help men live longer, but other studies have not found such a difference.
