Why Is It Important To Know The Risk Level Of Your Cancer
Knowing whether your cancer is low-risk or higher-risk is important when you are making treatment choices.
The risk level of your cancer is based on the results from your tests and examinations, such as the PSA test, digital rectal examination, and prostate biopsy.
- Low-risk means that the cancer isn’t likely to grow right away. There is a chance it may grow so slowly that it never causes symptoms.
- Medium-risk means that the cancer is more likely to grow. Most men will likely need treatment with radiation therapy or surgery.
- High-risk means that the cancer will most likely grow right away. Men will likely need treatment with radiation therapy or surgery.
Your doctor can help you understand your test results and the risk level of your cancer. Then you can compare your treatment options and make the choice that seems best to you.
What Are The Benefits Of Surgery
The success rate for surgery to treat prostate cancer is very high when all the cancer is removed. Surgical treatment is generally safe, with most men making a full recovery within two months after surgery.
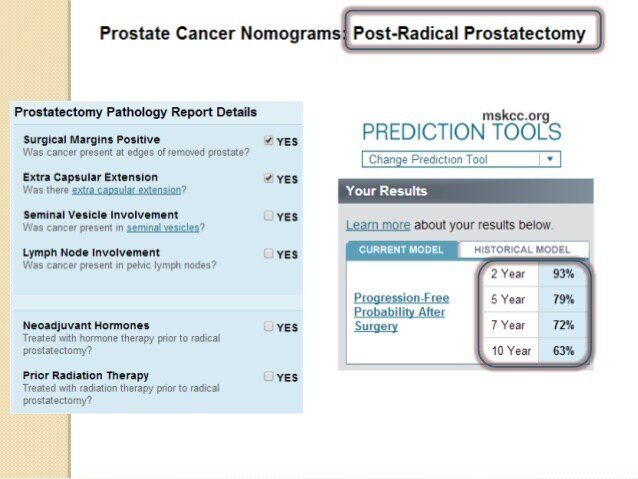
Further, surgery provides information about the exact genetics and state of cancer. Genetic analysis of surgically removed prostate tissue allows doctors to estimate prognosis and plan any complementary treatments.
What Is Prostate Cancer
Prostate cancer develops when abnormal cells in the prostate gland grow in an uncontrolled way, forming a malignant tumour.
Prostate cancer is the second most common cancer diagnosed in men in Australia and the third most common cause of cancer death. It is estimated that 18,110 new cases of prostate cancer will be diagnosed in Australia in 2021. One in 6 men will be diagnosed with prostate cancer by the age of 85. It is more common in older men, with over 63% of cases diagnosed in men over 65 years of age.
Early prostate cancer refers to cancer cells that have grown but do not appear to have spread beyond the prostate.
There are two stages of advanced prostate cancer:
- locally advanced prostate cancer where the cancer has spread outside the prostate to nearby parts of the body or glands close to the prostate
- metastatic prostate cancer where the cancer has spread to distant parts of the body.
The five year survival rate for prostate cancer is 95%.
Recommended Reading: Perineural Invasion Present
Screening For Prostate Cancer
There are no tests available with sufficient accuracy to screen populations of men for early signs of prostate cancer. However, early detection and treatment can significantly improve prostate cancer survival.
The test most commonly used to aid early detection of prostate cancer is the prostate specific antigen blood test. This is not a diagnostic test as it can only indicate changes in the prostate. If you are concerned about prostate cancer you should talk to your doctor and make an informed choice about whether to have one of the tests designed to find early signs of prostate cancer, in view of the potential risks and benefits.
There are no proven measures to prevent prostate cancer.
Radiation Therapy: Effective For Prostate Cancer

Research published in the Journal of Medical Imaging and Radiation Oncology in 2015 shows that external-beam radiation therapy is a highly effective treatment option for prostate cancer.
Men with localised prostate cancer who are treated with external-beam radiation therapy have a cure rate of 95.5% for intermediate-risk prostate cancer and 91.3% for high-risk prostate cancer.
The 5-year survival rate using this treatment is 98.8% overall.
When compared to other common treatment options such as surgery or brachytherapy, external-beam was as effective and in some cases more effective.
A/Prof Tom Shakespeare, Radiation Oncologist at the North Coast Cancer Institute, led the eight year study comparing the effectiveness of external-beam radiation therapy with other common treatment options such as surgery or brachytherapy.
The main outcome that we have seen from this study is that external-beam radiation therapy is one of the most effective treatment options for prostate cancer, he said.
These are great results showing that radiation therapy is as effective, or even better, than other common treatment options such as surgery or brachytherapy.
In fact, based on the literature reviewed, it appears that external-beam radiation therapy is a superior treatment in some cases.
When patients are treated with modern external-beam radiation therapy, the overall cure rate was 93.3% with a metastasis-free survival rate at 5 years of 96.9%.
Unfortunately, this does not always happen.
Read Also: Can Bph Cause Constipation
Radiation Therapy For Prostate Cancer
Radiation therapy techniques have improved over the years. More precise radiation delivery techniques are designed to help spare normal tissue from exposure and reduce the severity of side effects. In addition to the external delivery of radiation, we now also have internal delivery options. In some cases, courses of radiation treatment may be more intense and shorter in duration.
The development and use of hydrogel spacersgel thats inserted between the prostate and the rectummay also reduce damage to tissue surrounding the prostate during radiation, which in turn helps to reduce treatment-associated side effects.
Going Home With A Catheter
You will be discharged from the hospital with a catheter in place to drain urine from your bladder into a bag. The doctor will remove this in the office in five to 14 days. Be sure to clean the catheter where it exits your penis twice a day with soap and water and to empty the bag frequently. The bag should always be positioned lower than your bladder.
On occasion, the catheter may irritate the bladder, causing bladder spasms that can be quite uncomfortable. If these occur, your doctor can prescribe medication that can help. Leakage of urine around where the catheter exits the penis also may occur and can be managed by wearing incontinence pads as described in the next section.
It is normal for your urine to look cloudy for a few weeks after surgery. Occasionally, bleeding may occur around the catheter or be noticed within the urine. This also is common. If you see large clots â more than an inch in length â or if the catheter becomes plugged, contact your doctor. No anesthesia is required for catheter removal, and most patients experience only a little discomfort.
Don’t Miss: External Prostate Massage For Prostatitis
Your Cancer Care Team
People with cancer should be cared for by a multidisciplinary team . This is a team of specialists who work together to provide the best care and treatment.
The team often consists of specialist cancer surgeons, oncologists , radiologists, pathologists, radiographers and specialist nurses.
Other members may include physiotherapists, dietitians and occupational therapists. You may also have access to clinical psychology support.
When deciding what treatment is best for you, your doctors will consider:
- the type and size of the cancer
- what grade it is
- whether the cancer has spread to other parts of your body
Prostate Cancer Survival Trends Over Time
As with most cancers, survival for prostate cancer is improving. However, interpretation of prostate cancer survival trends is difficult as the case-mix on which they are based is likely to have changed over time with earlier diagnoses following the advent of TURP and PSA testing. The detection of a greater proportion of latent, earlier, slow-growing tumours in more recent time periods will have the effect of raising survival rates due to lead-time bias . Lead-time bias for prostate cancer is estimated to be between five and 12 years, varying with a man’s age at screening. Data from the European Randomized Study of Prostate Cancer estimates that for a single screening test, mean lead times are 12 years at age 55 and six years at age 75. Some of the increase may also be attributed to genuine improvements in survival due to more effective treatment, for both early, aggressive prostate cancers and advanced cases.
One-year age-standardised net survival for prostate cancer has increased from 66% during 1971-1972 to 94% during 2010-2011 in England and Wales an absolute survival difference of 28 percentage points.
Prostate Cancer , Age-Standardised One-Year Net Survival, Men , England and Wales, 1971-2011
Prostate Cancer , Age-Standardised Five-Year Net Survival, Men , England and Wales, 1971-2011
Prostate Cancer , Age-Standardised Ten-Year Net Survival, Men , England and Wales, 1971-2011
Recommended Reading: What Is The Va Disability Rating For Prostate Cancer
How Is Prostate Cancer Staged
Prostate cancer is one of the most common types of cancer that develops in men and is the second leading cause of cancer deaths in American men, behind lung cancer and just ahead of colorectal cancer. The prognosis for prostate cancer, as with any cancer, depends on how advanced the cancer has become, according to established stage designations.
The prostate gland is a walnut-sized gland present only in men, found in the pelvis below the bladder. The prostate gland wraps around the urethra and lies in front of the rectum. The prostate gland secretes part of the liquid portion of the semen, or seminal fluid, which carries sperm made by the testes. The fluid is essential to reproduction.
The term to stage a cancer means to describe the evident extent of the cancer in the body at the time that the cancer is first diagnosed.
- Clinical staging of prostate cancer is based on the pathology results, physical examination, PSA, and if appropriate, radiologic studies.
- The stage of a cancer helps doctors understand the extent of the cancer and plan cancer treatment.
- Knowing the overall results of the different treatments of similarly staged prostate cancers can help the doctor and patient make important decisions about choices of treatment to recommend or to accept.
Prostate Cancer Treatment: Radiation Therapy
Radiation, focused as a beam, can be used to kill cancer cells, especially those cells that have migrated from the prostate gland. Beams of radiation can be used to reduce bone pain caused by invasive cancer cells.
Low Dose Rate Brachytherapy
In another type of radiation therapy termed low dose rate brachytherapy, radioactive pellets about the size of a grain of rice are inserted into the prostate.
High Dose Rate Brachytherapy
High dose rate brachytherapy applies more radioactive sources temporarily into the cancerous prostate gland.
Both methods have side effects that can include erectile dysfunction, urinary tract problems, diarrhea, and other side effects.
Don’t Miss: What Happens To The Prostate Later In Life
The Stages Of Prostate Cancer: What You Need To Know
After a prostate cancer diagnosis, your oncologist will refer to the stage of your cancer. All cancers are categorized into four distinct stages, each of which identifies the progress of the growth of cancerous cells within clinically defined standards. These stages help doctors determine the most appropriate care for each patient based on his or her condition, and can also provide easy-to-understand context for your diagnosis. Learn more about the stages of prostate cancer, how each stage will affect your treatment plan and the survival rates for each stage, then contact Regional Cancer Care Associates to schedule a consultation.
Treatment Options For Prostate Cancer
Early-stage prostate cancer is often slow-growing. Here, it is hard to balance treatment benefits against its side effects. Therefore, delaying treatment until there is evidence of cancer progression is one way to avoid unnecessary side effects.
In some cases, a doctor may recommend watchful waiting or active surveillance to avoid unnecessary treatments.
You May Like: Does Enlarged Prostate Affect Ejaculation
How Is Stage 2 Prostate Cancer Treated
Your doctor will recommend treatment based on several factors, including your age, overall health, and whether or not youre having symptoms.
Your doctor might consider active surveillance if you have a slow-growing cancer and no symptoms. That means you wont actually be treating the cancer, but you will be monitoring it carefully with your doctor. This might involve visiting your doctor every six months, which would include a digital rectal exam and PSA testing. You might also need an annual prostate biopsy.
Active surveillance is only an option if you can commit to following up as advised by your doctor. Treatment will be considered if there are any changes.
Treatment may involve a combination of therapies, some of which are:
Long Term Side Effects
Once the inflammation is all healed, there can be some scarring that occurs. This is one way in which the body heals inflammation. Scarring can cause long term side effects. An example would be some scarring of the blood vessels and nerves that control the erections, which would result in erectile dysfunction .
Long term side effects are harder to treat, because it is not easy to treat scar tissue. Treatments like hyperbaric oxygen therapy and laser therapy may be required. As well, long term side effects can be long lasting or permanent.
Fortunately, the most common urinary and rectal side effects with prostate radiation are short term side effects. The only common long term side effect is weakening of the erections. Less common long term side effects are bleeding from the rectum and incontinence .
Q) Will I feel sick while Im on radiation?
A) No. The side effects are mostly in the prostate, rectum, and bladder area.
Q) I have heard that radiation can burn you up. Will I get burns on my skin?
A) No. There is usually no skin reaction from prostate radiation. Occasionally there can be a few pinkish patches that go away in a few weeks.
Q) Will I be able to work? Will I be able to drive? Will I be able to play golf?
A) Yes, yes, yes!
You May Like: What Is Perineural Invasion In Prostate Cancer
Prostate Cancer Is Common With Aging
After skin cancer, prostate cancer is the most common cancer in men. About 1 in 7 men will be diagnosed with prostate cancer in their lifetime. And these are just the men who are diagnosed. Among very elderly men dying of other causes, a surprising two-thirds may have prostate cancer that was never diagnosed.
Only 1 in 36 men, though, actually dies from prostate cancer. That’s because most prostate cancers are diagnosed in older men in whom the disease is more likely to be slow-growing and non-aggressive. The majority of these men eventually pass away from heart disease, stroke, or other causes — not their prostate cancer.
Open Radical Prostatectomy Vs Minimally Invasive Radical Prostatectomy
In 2003, only 9.2% of radical prostatectomies were done using a minimally invasive procedure. By 2007, that number had jumped to 43.2%. In 2009, researchers in Boston reported on a study that compared outcomes, benefits, and complications of open surgery vs. minimally invasive surgery:
- No difference was found in deaths or in the need for additional cancer therapy between the two approaches.
- The median hospital stay was two days for minimally invasive surgery and three days for open surgery.
- 2.7% of men having laparoscopic surgery required a blood transfusion compared with 20.8% of men having open surgery.
- There was more anastomotic stricture — narrowing of the suture where internal body parts are rejoined — for open surgery than for minimally invasive surgery .
- There were fewer respiratory complications with minimally invasive surgery than with open surgery .
- There were lower rates of incontinence and erectile dysfunction with open surgery. The overall rate was 4.7% for laparoscopic surgery and 2.1% for open surgery.
Also Check: Mri Prostate Cpt Code
Learn More About Prostate Cancer Care At Rcca
If youve been diagnosed with prostate cancer or are concerned about potential symptoms, contact RCCA today. Our team of cancer care specialists will assess the stage of your cancer using the latest diagnostic methods and work with you to design a fully individualized care plan that includes advanced treatment options, the potential for clinical trials, and support that addresses physical and emotional well-being. To speak with a representative right away, please call 844-474-6866.
What Are The Stages Of Prostate Cancer
Cancer staging is first described using what is called a TNM system. The “T” refers to a description of the size or extent of the primary, or original, tumor. “N” describes the presence or absence of, and extent of spread of the cancer to lymph nodes that may be nearby or further from the original tumor. “M” describes the presence or absence of metastases — usually distant areas elsewhere in the body other than regional lymph nodes to which the cancer has spread. Cancers with specific TNM characteristics are then grouped into stages, and the stages are then assigned Roman numerals with the numerals used in increasing order as the extent of the cancer being staged increases or the cancer prognosis worsens. Prognosis is finally reflected by considering the patient’s PSA score at presentation as well as their Gleason score in assigning a final stage designation.
The American Joint Commission on Cancer system for prostate cancer staging is as follows:
Traditionally, advanced prostate cancer was defined as disease that had widely metastasized beyond the prostate, the surrounding tissue, and the pelvic lymph nodes and was incurable. However, a more contemporary definition includes patients with lower grade disease with an increased risk of progression and/or death from prostate cancer in addition to those with widely metastatic disease.
The National Cancer Institute and the National Comprehensive Cancer Network guidelines on prostate cancer version 2.2017 indicate the following:
Also Check: Do Females Have Prostate Cancer
Prostate Cancer Patients Who Undergo Surgery Have High Survival Rates
ByLive Science Staff30 May 2013
Men with prostate cancer who undergo surgery to remove their prostate glands have a high survival rate and low rates of cancer recurrence, cancer spread and death, according to new research.
The study included 10,332 men who had the surgery called a radical prostatectomy between 1987 and 2004. Between five and 20 years after having the surgery, 3 percent of those patients died of the cancer, 5 percent saw their cancer spread to other organs and 6 percent had a recurrence of cancer in their prostates, according to researchers from the Mayo Clinic.
“These are excellent survival rates,” said Dr. R. Jeffrey Karnes, a Mayo Clinic urologist, in a statement. “They show that radical prostatectomy is a benchmark for treatment of men with prostate cancer that has not spread.”
Among cancers, prostate cancer has a relatively high survival rate in general. Five years after diagnosis, the survival rate is nearly 100 percent, and 10 years after diagnosis, the survival rate is 90 percent, according to 2010 data from the American Cancer Society.
In the study, the researchers looked at data from 1987 to 2004. During that time, the prostate-specific antigen test was introduced as a method of early detection it was approved by the FDA in 1994.
Before the PSA test existed, prostate cancer was detected by symptoms or by a digital rectal exam, both of which were less likely to detect cancer before it had spread beyond the prostate.
