Proton Beam Radiation Therapy
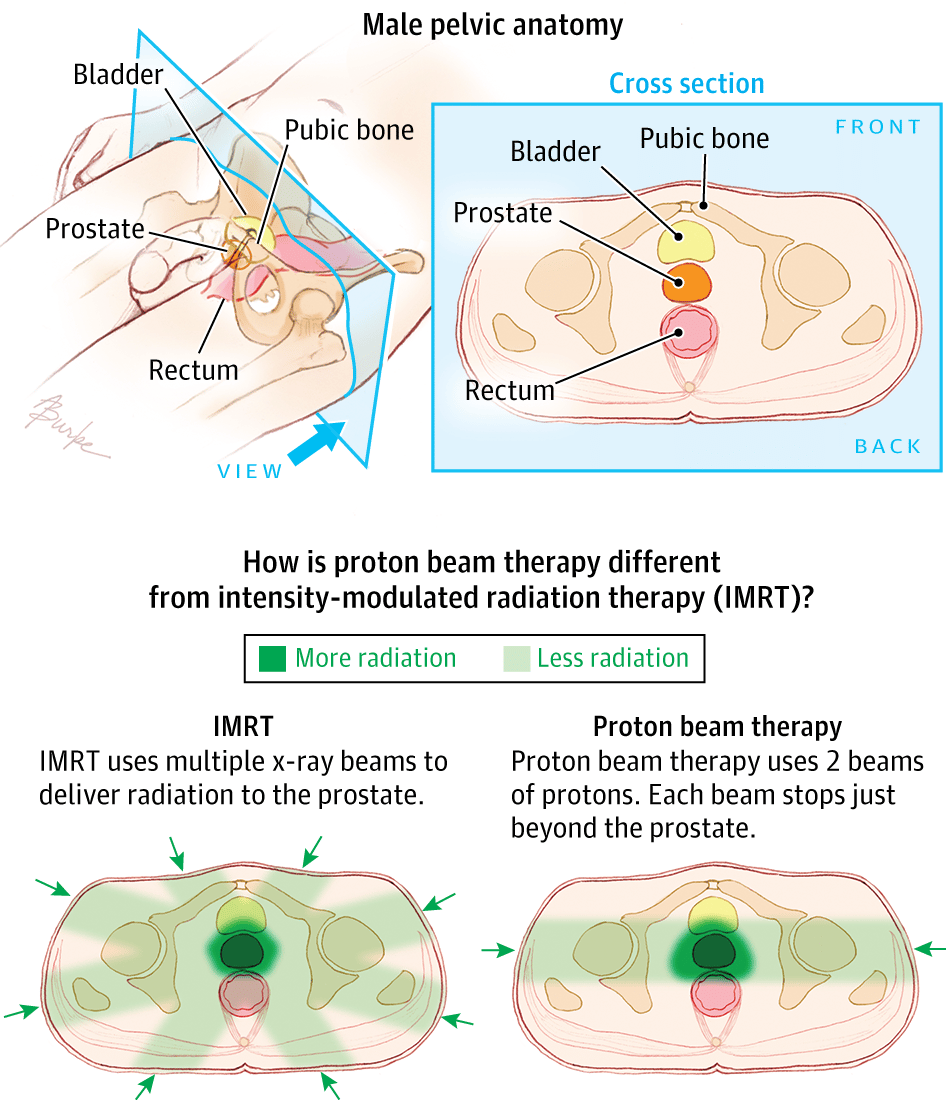
Proton beam therapy focuses beams of protons instead of x-rays on the cancer. Unlike x-rays, which release energy both before and after they hit their target, protons cause little damage to tissues they pass through and release their energy only after traveling a certain distance. This means that proton beam radiation can, in theory, deliver more radiation to the prostate while doing less damage to nearby normal tissues. Proton beam radiation can be aimed with techniques similar to 3D-CRT and IMRT.
Although in theory proton beam therapy might be more effective than using x-rays, so far studies have not shown if this is true. Right now, proton beam therapy is not widely available. The machines needed to make protons are very expensive, and they arent available in many centers in the United States. Proton beam radiation might not be covered by all insurance companies at this time.
Prostate Cancer: Radiation Therapy
Radiation therapy, also called X-ray therapy, uses high levels of radiation to kill prostate cancer cells or keep them from growing and dividing while minimizing damage to healthy cells.
Radiation can be given from a machine outside the body and directed at the prostate . Or a surgeon can place radioactive materials into the tumor . These radioactive materials can be temporary or permanent.
Good Prostate Cancer Care
Your MDT will be able to recommend what they feel are the best treatment options, but ultimately the decision is yours.
You should be able to talk with a named specialist nurse about treatment options and possible side effects to help you make a decision.
You should also be told about any clinical trials you may be eligible for.
If you have side effects from treatment, you should be referred to specialist services to help stop or ease these side effects.
You May Like: How Does A Prostate Massager Work
Uncertainty About Radiation For People With A Higher Risk Of Recurrence
After a diagnosis of early-stage breast cancer, radiation therapy following a lumpectomy is used to reduce the chance that the cancer will come back in the same breast. There are multiple options for breast radiation therapy, including whole-breast radiation and partial-breast radiation, Dr. Salerno said, and the decision of which treatment is most appropriate is made jointly between a patient and their radiation oncologist.
For whole-breast radiation, previous studies have shown that 3 weeks of treatment at slightly higher doses is as safe and effective as conventional whole-breast radiation over 56 weeks.
However, when the trial began a decade ago, this shorter, more intensive course of radiation, known as hypofractionated radiation therapy, had not yet been widely adopted in the United States, according to Lori Pierce, M.D., of the University of Michigan. Dr. Pierce, who was not involved with the trial, provided expert comments on the findings at the ASTRO meeting.
One reason for this slow adoption, Dr. Pierce said, was the uncertainty of whether and how to incorporate a boost of radiation for people who had a higher risk of recurrence.
When Is Radiation Therapy Given
Radiation therapy may be used:
- for localised or locally advanced prostate cancer it has similar rates of success to surgery in controlling prostate cancer that has spread to the lymph nodes
- if you are not well enough for surgery or are older
- after a prostatectomy for locally advanced disease, if there are signs of cancer left behind or the cancer has returned where the prostate used to be
- for prostate cancer that has spread to other parts of the body.
There are two main ways of delivering radiation therapy: from outside the body or inside the body . You may have one of these or a combination of both.
In intermediate and high-risk prostate cancer, radiation therapy is often combined with androgen deprivation therapy .
You May Like: Does Sex Improve Prostate Health
What The Research Shows About Radiation Vs Surgery
The ProtecT trial was a 10-year, randomized clinical study designed to compare radical prostatectomy, external-beam radiotherapy and active surveillance for the treatment of localized prostate cancer.
The results, published in 2016, showed that the rate of disease progression among men assigned to radiotherapy or radical prostatectomy was less than half the rate among men assigned to active monitoring. However, there was no significant difference in survival at the median 10-year follow-up for radiation therapy, surgery or active surveillance.
If youre interested in directly comparing treatment outcomes by treatment method and risk group , the Prostate Cancer Free Foundation provides an interactive graph on its website with information from data obtained from over 129,000 prostate cancer patients over a 15-year period.
As discussed earlier in the sections on the side effects of radiation therapy and surgery, the researchers conducting the ProtecT trial also looked at side effects and quality-of-life issues and found that the three major side effects of these two treatment options that affect quality of life after prostate cancer treatment are urinary incontinence, sexual dysfunction and bowel health.
The trial found that urinary leakage and erectile dysfunction were more common after surgery than after radiation therapy. Gastrointestinal bowel problems were more common after radiation therapy.
Easier To Have Additional Treatment
In a perfect world, all you will need is one treatment. However, cancer is cancer. So, we will follow your PSA to see if there is any sign that the cancer came back.
If the PSA starts to creep up, higher than 0.2, then we can always add radiation later. However, there is some trade off to this in that some of the side effects from radiation can become more common after the prostate has been removed.
Don’t Miss: Pelvic Floor Exercises After Prostate Surgery
A Biopsy Is Done To Diagnose Prostate Cancer And Find Out The Grade Of The Cancer
A transrectal biopsy is used to diagnose prostate cancer. A transrectal biopsy is the removal of tissue from the prostate by inserting a thin needle through the rectum and into the prostate. This procedure may be done using transrectal ultrasound or transrectal MRI to help guide where samples of tissue are taken from. A pathologist views the tissue under a microscope to look for cancer cells.
Sometimes a biopsy is done using a sample of tissue that was removed during a transurethral resection of the prostate to treat benign prostatic hyperplasia.
If cancer is found, the pathologist will give the cancer a grade. The grade of the cancer describes how abnormal the cancer cells look under a microscope and how quickly the cancer is likely to grow and spread. The grade of the cancer is called the Gleason score.
To give the cancer a grade, the pathologist checks the prostate tissue samples to see how much the tumor tissue is like the normal prostate tissue and to find the two main cell patterns. The primary pattern describes the most common tissue pattern, and the secondary pattern describes the next most common pattern. Each pattern is given a grade from 3 to 5, with grade 3 looking the most like normal prostate tissue and grade 5 looking the most abnormal. The two grades are then added to get a Gleason score.
What Are The Types Of Radiation Therapy Used For Prostate Cancer
Radiationtherapy for prostate cancer can be divided into two main categories.
Externalbeam radiation :Using a machine outside the body, beams of radiation are focused on theprostate gland. This can help relieve symptoms such as pain while limiting thedamage to the tissues surrounding the prostate.
The 4methods of external beam radiation are:
- Three-dimensional conformal radiation therapy
- Stereotactic body radiation therapy
- Proton beam radiation therapy
Brachytherapy:Small radioactive pellets are inserted into the prostate, each one about thesize of a grain of rice. About 100 pellets are used to limit the damage tosurrounding tissues and organs. Brachytherapy is most often used forearly-stage cases and is sometimes combined with EBRT. The pellets can eitherbe inserted for a couple of days for high dosages or a few months for lowdosage depending on the patients overall status.
Read Also: How Big Should A Prostate Be
Prostate Cancer Risk Groups
Prostate cancer can be categorised into one of 5 risk groups in the Cambridge Prognostic Group .
Doctors will look at the Grade Group , prostate specific antigen level and tumour stage to decide which CPG group the prostate cancer is.
The risk group of the cancer will help determine which types of treatments will be necessary.
If prostate cancer is diagnosed at an early stage, the chances of survival are generally good.
How Is Prostate Cancer Treated
Lorenzo asked his doctors about survival and side effects and talked to friends and family members before deciding on treatment. He shares his story in this blog post.
Different types of treatment are available for prostate cancer. You and your doctor will decide which treatment is right for you. Some common treatments are
- Expectant management. If your doctor thinks your prostate cancer is unlikely to grow quickly, he or she may recommend that you dont treat the cancer right away. Instead, you can choose to wait and see if you get symptoms in one of two ways:
- Active surveillance. Closely monitoring the prostate cancer by performing prostate specific antigen tests and prostate biopsies regularly, and treating the cancer only if it grows or causes symptoms.
- Watchful waiting. No tests are done. Your doctor treats any symptoms when they develop. This is usually recommended for men who are expected to live for 10 more years or less.
You May Like: What Is The Recovery Time For Prostate Removal
Remission And The Chance Of Recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having no evidence of disease or NED.
A remission can be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. Although there are treatments to help prevent a recurrence, such as hormonal therapy and radiation therapy, it is important to talk with your doctor about the possibility of the cancer returning. There are tools your doctor can use, called nomograms, to estimate someone’s risk of recurrence. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. Learn more about coping with the fear of recurrence.
In general, following surgery or radiation therapy, the PSA level in the blood usually drops. If the PSA level starts to rise again, it may be a sign that the cancer has come back. If the cancer returns after the original treatment, it is called recurrent cancer.
When this occurs, a new cycle of testing will begin again to learn as much as possible about the recurrence, including where the recurrence is located. The cancer may come back in the prostate , in the tissues or lymph nodes near the prostate , or in another part of the body, such as the bones, lungs, or liver . Sometimes the doctor cannot find a tumor even though the PSA level has increased. This is known as a PSA recurrence or biochemical recurrence.
What Is 3d Conformal Radiation Therapy

Itâs a procedure that uses a computer to make a three-dimensional picture of your tumor. It helps your treatment team deliver the highest possible dose of radiation to the tumor while minimizing the damage to normal tissue.
3D conformal radiation therapy uses CT-based treatment combined with three-dimensional images of a prostate tumor. CT is short for computed tomography, which uses X-rays to produce detailed pictures inside the body.
So far, this technique has worked well for localized tumors such as prostate cancer limited to the prostate gland.
Recommended Reading: How To Check My Prostate At Home
Note The Time Of Your Procedure
A staff member from the Admitting Office will call you after 2:00 pm the day before your procedure. If your procedure is scheduled for a Monday, theyll call you on the Friday before.
The staff member will tell you what time to arrive at the hospital for your procedure. Theyll also remind you where to go. If you dont get a call by 7:00 pm, call .
Study Data And Findings
Investigators reviewed data from 143,886 men who were treated for localized prostate cancer at Veterans Affairs medical facilities between 2000 and 2015. The men ranged from 60 to 71 years in age, and came from diverse racial and ethnic backgrounds. Among them, 52,886 were treated with radiation within a year of being diagnosed. The other 91,000 men opted either for surgery over a similar time frame, or chose to have their cancers monitored and treated only when or if routine exams showed signs of progression.
After a median follow-up of nine years, 3% of the radiation-treated men had developed secondary cancers, compared to 2.5% of the men who chose other options. The four most common cancers in the order of how frequently they were detected were bladder cancer, leukemia, lymphoma, and rectal cancer. The risk of developing these secondary cancers increased steadily with time, peaking five to six years after radiation treatment was finished.
Dr. Oliver Sartor, an oncologist at Tulane University School of Medicine in New Orleans who was not involved in the study, says the potential for secondary cancers is an important issue that men should discuss with their doctors when evaluating treatment options.
Read Also: What Side Effects Does Having Your Prostate Removed
Proton Beam Radiati On Therapy
Proton beam radiation therapy capitalizes on a unique physical property of high energy protons generated from a cyclotron. The accelerated charged particles travel through tissue until reaching a depth determined by their energy. Once they reach that depth, the remainder of the radiation dose is deposited in a sharp Bragg peak with no dose going beyond that point. When multiple proton beams are used, a very sharp and tight radiation dose distribution is created. This modality is especially attractive when tumors are in close proximity to sensitive organs. PCa is one of the more common indications in which proton therapy is utilized.
At Washington University in St. Louis we are collaborating with investigators from Massachusetts General Hospital and the Harvard Medical School conducting a randomized clinical trial of IG-IMRT versus proton beam radiation in men with low and intermediate risk PCa. The PARTIQoL trial is seeking to measure and compare relative the impact of the two modalities on patient quality of life after treatment. Figure 1 provides a comparison of these two treatment modalities.
Axial CT slice showing conformality of intensity modulated radiation therapy. Radio-opaque markers are apparent in the anterior aspect of the prostate gland. Axial CT slice showing conformality of proton beam radiation therapy in the same patient as panel a. More sparing of the anterior-lateral rectal wall and less dose to peripheral tissues is apparent.
Prices And Where To Get It
The cost of a radical prostatectomy varies depending on insurance status and location of surgery.
Costs may include hospital fees, anesthesia fees, and surgeon fees. The average cost of hospital fees for prostatectomy in the United States is about $34,000. Anesthesiologist and surgeon fees average about $8,000. What out-of-pocket expenses the person being treated incurs will depend on their insurance.
The location of the procedure can be with a local surgeon, or the person being treated may travel to see a regional or national expert.
Read Also: What Happens In Prostate Cancer
Brachytherapy Or Internal Radiation Therapy
Internal radiation therapy , also known as brachytherapy, involves placing radioactive seeds on the prostate gland inside the body. The seeds are around the size of a grain of rice.
The implant may be temporary or permanent:
- Temporary: The doctor inserts the seeds into a small tube and leaves them there for between 5-15 minutes . A person may need 1-4 sessions, typically over the course of 2 days.
- Permanent: The doctor will place around 1000 radioactive seeds that release radiation for several weeks to months. Often, they leave the seeds in place when not active since they likely will not cause discomfort.
Before inserting the seeds, the doctor will give the patient either a general or local anesthetic. They may use imaging technology to help ensure they position the seeds accurately.
Stereotactic Body Radiation Therapy
This technique uses advanced image guided techniques to deliver large doses of radiation to a precise area, such as the prostate. Because there are large doses of radiation in each dose, the entire course of treatment is given over just a few days.
SBRT is often known by the names of the machines that deliver the radiation, such as Gamma Knife, X-Knife, CyberKnife, and Clinac.
The main advantage of SBRT over IMRT is that the treatment takes less time . The side effects, though, are not better. In fact, some research has shown that some side effects might actually be worse with SBRT than with IMRT.
Don’t Miss: What Is Prostate Gland Hypertrophy
What Is External Beam Radiation Therapy For Prostate Cancer
External beam radiation therapy treats prostate cancer with X-ray beams from a machine. The treatment is painless and only lasts for a few minutes at a time.
Siteman radiation oncologists were among the first in the U.S. to deliver external beam radiation using Intensity-Modulated Radiation Therapy . This technique enhances the delivery of high doses of radiation. In addition, they also use advanced-imaging methods such as MRI and PET scans a technique known as Image-Guided Radiation Therapy to focus treatment on the prostate, thereby reducing radiation delivery to the adjacent bladder and rectum.
Patients who develop a recurrence of their cancers after prior radical prostate surgery can be effectively treated with radiation therapy. If the prostate has been removed, radiation is delivered to the space where the prostate used to be.
Brachytherapy is radiation therapy that comes from a source implanted within the body. There are two different types: low-dose-rate brachytherapy and high-dose-rate brachytherapy.
