Modifying Risk Level Classification
The new millennium brought changes as 1) more epidemiological and demographic data accumulated, 2) the nature of PCa was better understood, and 3) sub-radical therapies such as focal ablation or hemi-ablation were developed to offer comparable cancer control but with far fewer side effect risks. A need was seen to add qualifiers to low risk PCa. Thus, the National Comprehensive Cancer Network subdivided this category into very-low and low-risk types to help doctors and patients determine for which men Active Surveillance or a sub-radical treatment would be safe choice.
The NCCN system did not qualify intermediate risk PCa. It differs a bit from DAmico, defining it as stage T2b or T2c, Gleason score of 7, and PSA level 10-20 ng/mL. However, by 2015 it was clear that this category was the largest group of PCa cases with the most heterogeneous disease characteristics. There was a wide range of PCa-specific mortality as well as biochemical or clinical recurrence after radical treatment by prostatectomy, beam radiation, and brachytherapy . Studies began to show that all Gleason 7 is not created equal men with Gleason 3+4=7 had better outcomes than those with Gleason 4+3=7, Therefore, In order to better understand this risk group, new classification systems have been proposed that help reduce its heterogeneity by subdividing men with intermediate-risk prostate cancer into favorable and unfavorable subgroups.
Also Check: Elevated Prostate Levels Blood Test
Agents Related To Bone Health In Crpc
In a multicenter study, 643 men with CRPC and asymptomatic or minimally symptomatic bone metastases were randomized to intravenous zoledronic acid every 3 weeks or placebo.228 At 15 months, fewer men in the zoledronic acid 4-mg group than men in the placebo group had SREs . An update at 24 months also revealed an increase in the median time to first SRE .229 No significant differences were found in OS. Other bisphosphonates have not been shown to be effective for prevention of disease-related skeletal complications. Earlier use of zoledronic acid in men with castration-naïve prostate cancer and bone metastases is not associated with lower risk for SREs, and in general should not be used for SRE prevention until the development of metastatic CRPC.230
The randomized TRAPEZE trial used a 2×2 factorial design to compare clinical PFS as the primary outcome in 757 men with bone metastatic CRPC treated with docetaxel alone or with zoledronic acid, 89Sr, or both.231 The bone-directed therapies had no statistically significant effect on the primary outcome or on OS in unadjusted analysis. However, adjusted analysis revealed a small effect for 89Sr on clinical PFS . For secondary outcomes, zoledronic acid improved the SRE-free interval and decreased the total SREs compared with docetaxel alone.
Database Quality Assurance And Clinical Outcomes
An extensive quality assurance program was initiated to confirm database quality, including various error checking, missing data minimization, and outcome confirmation procedures. Risk stratification categories were calculated from the available information in the ProCaRS database, including GUROC 3-group14 and NCCN 5-group18,19 risk stratification. In terms of GUROC risk stratification, the following risk groups have been defined:
-
Low-risk: 1997 AJCC T1-T2a, prostate-specific antigen â¤10 ng/mL, and Gleason score â¤6
-
Intermediate-risk: 1997 AJCC T1-T2, PSA â¤20 ng/mL, and Gleason score â¤7 not otherwise low-risk
-
High-risk: 1997 AJCC T3-T4 or PSA > 20 ng/mL, or Gleason score 8-10
The current NCCN risk categories18,19 are defined as:
-
Very-low-risk: T1c, Gleason score â¤6, PSA < 10, < 3 biopsy cores positive, â¤50% cancer in each core, and PSA density < 0.15 ng/mL/g
-
Low-risk: T1-T2a, Gleason score 2-6, and PSA < 10 not very-low-risk
-
Intermediate-risk: T2b or T2c, and/or Gleason score 7, and/or PSA 10-20 not low-risk
-
High-risk: T3a, or PSA > 20, or Gleason score 8-10 not very high risk
-
Very-high-risk: T3b-4
Don’t Miss: What Happens When You Get Your Prostate Removed
Cancer Care Ontario/american Society Of Clinical Oncology
In 2016, the American Society of Clinical Oncology endorsed Cancer Care Ontarios guideline on active surveillance for the management of localized prostate cancer. The recommendations include the following:
- Active surveillance is the recommended disease management strategy for most patients with lowrisk localized prostate cancer.
- Because of heterogeneity within this population, factors such as younger age, high-volume Gleason 6 cancer, patient preference, and/or African American ethnicity should be taken into account in the decision to use active surveillance.
- Young patients with high-volume Gleason 6 cancer should be closely scrutinized for the presence of highergrade cancer definitive therapy may be warranted for select patients.
- For patients with limited life expectancy and lowrisk cancer, watchful waiting may be more appropriate than active surveillance.
- Active treatment is recommended for most patients with intermediaterisk localized prostate cancer, but active surveillance may be offered to select patients with lowvolume, intermediaterisk localized prostate cancer.
The guidelines recommend that the active surveillance protocol include the following tests:
Treatment By Cancer Type
NCCN MAKES NO REPRESENTATIONS OR WARRANTIES CONCERNING THE NCCN CONTENT, THE NCCN GUIDELINES OR DERIVATIVE RESOURCES PROVIDED BY NCCN, ALL OF WHICH ARE PROVIDED “AS IS.” NCCN DISCLAIMS ALL WARRANTIES, EXPRESS OR IMPLIED, INCLUDING, WITHOUT LIMITATION, THE IMPLIED WARRANTIES OF MERCHANTABILITY AND FITNESS FOR A PARTICULAR PURPOSE. NCCN DOES NOT WARRANT THE ACCURACY, APPROPRIATENESS, APPLICABILITY OR COMPLETENESS OF THE NCCN CONTENT, THE NCCN GUIDELINES OR ANY DERIVATIVE RESOURCES, NOR DOES NCCN MAKE ANY REPRESENTATIONS REGARDING THE USE OR RESULTS OF THE USE OF THE NCCN CONTENT, THE NCCN GUIDELINES OR ANY SUCH DERIVATIVE RESOURCES.
NCCN EXPLICITLY DISCLAIMS THE APPROPRIATENESS OR APPLICABILITY OF THE NCCN CONTENT, THE NCCN GUIDELINES, AND ANY DERIVATIVE RESOURCES, OR THE USE OR APPLICATION OF THE NCCN CONTENT, THE NCCN GUIDELINES OR ANY SUCH DERIVATIVE RESOURCES, TO ANY SPECIFIC PATIENT’S CARE OR TREATMENT. ANY CLINICIAN SEEKING TO APPLY OR CONSULT THE NCCN CONTENT, THE NCCN GUIDELINES AND/OR ANY DERIVATIVE RESOURCES IS EXPECTED TO USE INDEPENDENT MEDICAL JUDGMENT IN THE CONTEXT OF THE INDIVIDUAL CLINICAL CIRCUMSTANCES TO DETERMINE ANY PATIENT’S CARE OR TREATMENT.
You May Like: Main Symptoms Of Prostate Cancer
Apalutamide In M0 Crpc
The FDA approved apalutamide for treatment of patients with nonmetastatic CRPC on February 14, 2018.195 This approval was based on the phase 3 SPARTAN trial of 1,207 patients with M0 CRPC and PSADT 10 months.196 Participants were stratified according to PSADT , use of bone-sparing agents, and the presence of metastatic pelvic lymph nodes . After median follow-up of 20.3 months, apalutamide at 240 mg/day with ADT improved the primary endpoint of metastasis-free survival over placebo with ADT . No significant difference was seen in OS, although OS data were not mature at the time of final analysis for metastasis-free survival. Adverse events included rash , fracture , and hypothyroidism . Patients with M0 CRPC can be offered apalutamide, if PSADT is 10 months . In a prespecified exploratory analysis of SPARTAN, health-related QOL was maintained in both the apalutamide and placebo groups.197
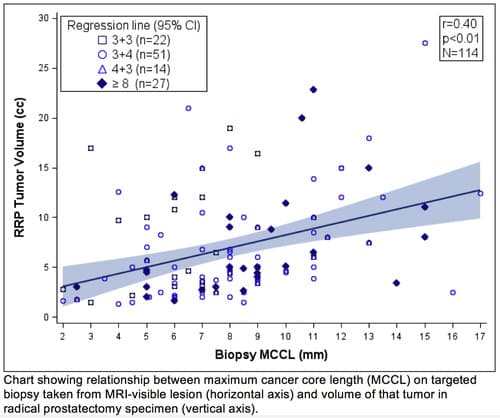
Evidence For Mpmri And Tumor Multigene Molecular Testing
The role of mpMRI in the diagnosis of prostate cancer has become increasingly important in recent years, as reflected in the NCCN and other prostate cancer guidelines.4 mpMRI typically includes diffusion-weighted imaging and/or dynamic contrast-enhanced images in addition to the standard anatomical T2-weighted imaging. The quality mpMRI involves a 3 T magnet. It has a higher signal to noise ratio, allowing quality imaging within a short time and without the use of an endorectal coil .
The NCCN guideline recommendations are based on evidence reviewed and voted on by the guideline panels. This evidence is eventually published in the Discussion section of the guidelines. However, because the NCCN guideline on prostate cancer is updated so frequently, the Discussion section often lags behind the recommendations within the same guideline. In Version 2.2022 , for example, the Discussion section is dated November 17, 2020. Many of the recent updates related to the implementation of mpMRI have been based on its increased availability and ability to stage and characterize prostate cancer.
The NCCN recommendation to use tumor molecular testing is based on the goal of achieving personalized or precision medicine. Molecular testing of a tumor offers the potential to evaluate the biologic behavior of a cancer, which would aid in clinical decision making, the guideline says.
References
You May Like: Is Coffee Good For Prostate
Gene And Protein Tests For Prostate Cancer
For men with prostate cancer that is localized , a major issue is that its often hard to tell how quickly the cancer is likely to grow and spread. This can make it hard to decide if the cancer needs to be treated right away, as well as which types of treatment might be good options.
Some types of lab tests, known as genomic, molecular, or proteomic tests, can be used along with other information to help better predict how quickly a prostate cancer might grow or spread, and as a result, help decide what treatment options might be best and when they should be given. These tests look at which genes or proteins are active inside the prostate cancer cells. Examples of such tests include:
These tests continue to be studied to find more areas where they can be useful in prostate cancer risk and treatment decisions.
African Americans More Likely To Be Reclassified To High Genomic Risk
According to Dr Yamoah, preliminary results showed age to be the only standout variable between races, with a significant difference in age persisting between African-American men and nonAfrican-American men with respect to high genomic risk. The median age for African-American men was 61 years versus 67 years for the nonAfrican-American cohort.
We observed a significant difference in age for men who were clinically classified with early localized disease and yet had high genomic risk for metastatic disease within 5 years, he said. This finding points to an underlining discrepancy in age at diagnosis for African-American men, which may speak to the overall risk for development of prostate cancer in men of African origin. This could also have implications in screening guidelines.
In addition, a race-stratified comparison of NCCN and genomic risk groupings showed that low- and favorable-risk African Americans were more likely to be reclassified as high genomic risk for distant metastasis compared with nonAfrican Americans.
Among nonAfrican-Americans with clinically low-risk disease, we found no patients who were high genomic risk, Dr Yamoah said. In the African-American cohort, however, 20% of clinically low-risk patients were found to have high genomic risk for metastatic disease within 5 years, and this number was even higher for favorable-risk patients.
Don’t Miss: Is Green Tea Good For Prostate
Abiraterone Acetate In M1 Crpc
In April 2011, the FDA approved the androgen synthesis inhibitor, abiraterone, in combination with low-dose prednisone, for the treatment of men with metastatic CRPC who have received prior chemotherapy containing docetaxel.
FDA approval in the postdocetaxel setting was based on the results of a phase 3, randomized, placebo-controlled trial in men with metastatic CRPC previously treated with docetaxel-containing regimens.174,175 Patients were randomized to receive either abiraterone 1,000 mg orally once daily or placebo once daily , and both arms received daily prednisone. In the final analysis, median survival was 15.8 vs 11.2 months in the abiraterone and placebo arm, respectively .175 Time to radiographic progression, PSA decline, and pain palliation also were improved by abiraterone.175,176
The most common adverse reactions with abiraterone/prednisone were fatigue back or joint discomfort peripheral edema diarrhea, nausea, or constipation hypokalemia hypophosphatemia atrial fibrillation muscle discomfort hot flushes urinary tract infection cough hypertension urinary frequency and nocturia dyspepsia or upper respiratory tract infection. The most common adverse drug reactions that resulted in drug discontinuation were increased aspartate aminotransferase and/or alanine aminotransferase , or cardiac disorders .
Can Adt Compensate For Dose Escalation
The Prostate Cancer Study III examined the addition of ADT to SDRT and DERT in intermediate-risk patients . The preliminary results of this trial have now been published in abstract form. A total of 600 patients were enrolled. Intermediate-risk prostate cancer was defined as T1/T2 disease, GS 6, PSA level 1020 ng/mL or T1/T2 disease, GS of 7, PSA level 20 ng/mL. Patients were randomly assigned to one of three arms: 6 months of ADT plus 70 Gy to the prostate , 6 months of ADT plus 76 Gy , or 76 Gy alone . ADT consisted of bicalutamide and goserelin for 6 months. RT was delivered using a 3D conformal technique and started 4 months after the beginning of ADT. Median follow-up was 6.75 years. Primary endpoints were biochemical failure and disease-free survival . Secondary endpoints included OS, as well as hormonal and radiation-related toxicities. Biochemical failure was defined as 2 ng/mL above the PSA nadir.
Donât Miss: Incontinence After Robotic Prostate Surgery
Read Also: Does Caffeine Affect Your Prostate
Enzalutamide In M0 And M1 Crpc
On August 31, 2012, the FDA approved enzalutamide, a next-generation antiandrogen, for treatment of men with metastatic CRPC who had received prior docetaxel chemotherapy. Approval was based on the results of the randomized, phase 3, placebo-controlled trial .186,187 AFFIRM randomized 1,199 men to enzalutamide or placebo in a 2:1 ratio, and the primary endpoint was OS. Median survival was improved with enzalutamide from 13.6 to 18.4 months . Survival was improved in all subgroups analyzed. Secondary endpoints also were improved significantly, which included the proportion of men with > 50% PSA decline , radiographic response , radiographic PFS , and time to first skeletal related event . QOL measured using validated surveys was improved with enzalutamide compared with placebo. Adverse events were mild and included fatigue , diarrhea , hot flushes , headache , and seizures . The incidence of cardiac disorders did not differ between the arms. Enzalutamide is dosed at 160 mg daily. Patients in the AFFIRM study were maintained on GnRH agonist/antagonist therapy and could receive bone supportive care medications. The seizure risk in the enzalutamide FDA label was 0.9% versus 0.6% in the manuscript.186,188
National Comprehensive Cancer Network Recommendations
The NCCN guidelines for prostate cancer include treatment recommendations for CRPC based on the presence or absence of visceral metastases. For the most part, these recommendations are based on high-level evidence and are supported by uniform NCCN consensus .
CRPC without distant metastasis
-
Enrollment in clinical trial is preferred
-
Observation is acceptable
-
Secondary hormone therapy can be considered for patients with prostate-specific antigen doubling < 10 months anti-androgen therapy is acceptable for patients who previously received medical or surgical castration, ketoconazole, corticosteroids, diethylstilbestrol or other estrogens
CRPC with bone metastases
Measures to promote bone health include the following:
-
Zoledronic acid or denosumab
-
Avoidance of invasive dental surgery during treatment
-
Calcium and vitamin D supplements to prevent hypocalcemia during treatment
Radium-233 can be used to treat symptomatic bone metastases without visceral metastases.
Metastatic CRPC with no visceral metastases
-
Sipuleucel-T for asymptomatic or minimally symptomatic patients
-
Abiraterone plus prednisone or enzalutamide for asymptomatic patients
-
Docetaxel with prednisone for symptomatic patients may also be considered in a symptomatic patients with signs of rapid progression
-
Radium-233 for symptomatic patients
-
Secondary hormone therapy or enrollment in clinical trial may be considered
Metastatic CRPC with visceral metastases
-
Other secondary hormone therapy
Also Check: Can A Biopsy Spread Prostate Cancer
Favorable Vs Unfavorable Intermediate
The DAmico risk groups, initially published in 1998, were designed to stratify patients according to the likelihood of biochemical recurrencefree survival after radical prostatectomy or radiotherapy. The current NCCN guidelines are a slight modification of this classification system. However, in 2005 an International Society of Urological Pathology conference was held in order to reach a consensus regarding the grading of prostate cancer. A consensus statement was published in 2005, and as a result of the adoption of this new grading system, the reporting of secondary pattern Gleason grade 4 disease became more prevalent. Several investigators have reported on their observation of grade migration from GS 3+3 to GS 3+4 . This grade migration could cause a number of men who previously would have been categorized as low-risk to be assigned to the NCCN intermediate-risk category because of their GS, thereby improving the prognosis of both groups . Thus, it has been hypothesized that some men with GS 3+4 intermediate-risk prostate cancer may have a low risk of PCSM and higher rates of overall survival , similar to what is seen in patients with low-risk prostate cancer.
Only one intermediate-risk factor .
GS of 3+4=7 or less.
Less than 50% of biopsy cores positive for cancer.
Those who were classified as unfavorable could have any of the following:
More than one intermediate-risk factor.
GS of 4+3=7.
Greater than 50% positive biopsy cores.
New Perspective On Low
The paradigms of prostate cancer detection are changing so that detection of low-risk disease is not followed, and surveillance rather than treatment is offered to those with lower-risk disease, Dr Carroll said. This sentiment was echoed by the chair of the NCCN Prostate Cancer Guideline Committee, James L. Mohler, MD, Associate Director, Translational Research, Roswell Park Comprehensive Cancer Center, Buffalo, NY, who discussed management approaches in prostate cancer.
An alternative to performing biopsies in patients with elevated prostate-specific antigen levels is the use of serum- or urine-based biomarkers that increase the specificity of screening.
What theyre doing is determining which men with an elevated PSA are harboring clinically significant disease, defined by an elevated Gleason score, said Dr Carroll. These tests miss few high-risk cancers, but decrease the biopsy rate by 30% to 40%, he added.
The other big marker right now is multiparametric MRI , Dr Carroll told attendees. Using multiparametric MRI or biomarkers misses only approximately 1% to 2% of high-risk tumors, and even fewer if both tests are used, while avoiding unnecessary biopsies and detecting fewer lower-risk cancers.
In my opinion, very few men with low-risk disease should ever be treated, Dr Carroll posited. Several studies have shown that there is no harm in delaying treatment by up to 2 years, he noted.
Recommended Reading: Immunotherapy For Metastatic Prostate Cancer
European Society For Medical Oncology
The ESMO guidelines include the following treatment recommendations :
- Watchful waiting with delayed ADT for symptomatic progression is an option for men who are not suitable for, or are unwilling to have, radical treatment.
- Active surveillance is recommended for men with low-risk disease.
- Radical prostatectomy or radiation therapy is an option for men with low-risk disease not suitable for active surveillance, and is recommended for men with intermediate-risk disease.
- Primary ADT alone is not recommended as standard initial treatment for non-metastatic disease.
- External beam RT plus ADT is recommended for men with high-risk or locally advanced prostate cancer.
- RP plus pelvic lymphadenectomy is an option for selected men with high-risk disease.
- Men receiving radical RT for intermediate-risk disease should have short-course ADT for 4-6 months.
- Men receiving radical RT for high-risk disease should have long-course ADT .
- Neoadjuvant docetaxel chemotherapy may be offered before RT for young, fit men with very high-risk localized prostate cancer.
- Following RP, patients should have their serum PSA level monitored, with salvage RT recommended in the event of PSA failure.
- Adjuvant postoperative RT after RP is not routinely recommended.
