What Are Some Of The Limitations And Potential Harms Of The Psa Test For Prostate Cancer Screening
Detecting prostate cancer early may not reduce the chance of dying from prostate cancer. When used in screening, the PSA test can help detect small tumors that do not cause symptoms. Finding a small tumor, however, may not necessarily reduce a mans chance of dying from prostate cancer. Many tumors found through PSA testing grow so slowly that they are unlikely to threaten a mans life. Detecting tumors that are not life-threatening;
that requires treatment.
It Was Estimated That In :
- 115,800 Canadian men would be diagnosed with cancer and 44,100 men would die from cancer.
- 110,000 Canadian women would be diagnosed with cancer and 39,300 women would die from cancer.
- On average, 617 Canadians would be diagnosed with cancer every day.
- On average, 228 Canadians would die from cancer every day.
- Lung, breast, colorectal and prostate cancer are the most commonly diagnosed types of cancer in Canada .;
- These 4 cancers account for about half of all new cancer cases.
- Prostate cancer accounts for one-fifth of all new cancer cases in men.
- Lung cancer accounts for 14% of all new cases of cancer.
- Breast cancer accounts for one-quarter of all new cancer cases in women
- Colorectal cancer accounts for 12% of all new cancer cases.;
What Happens When Prostate Cancer Is Left Untreated
Doru Paul, MD, is triple board-certified in medical oncology, hematology, and internal medicine. He is an associate professor of clinical medicine at Weill Cornell Medical College and attending physician in the Department of Hematology and Oncology at the New York Presbyterian Weill Cornell Medical Center.
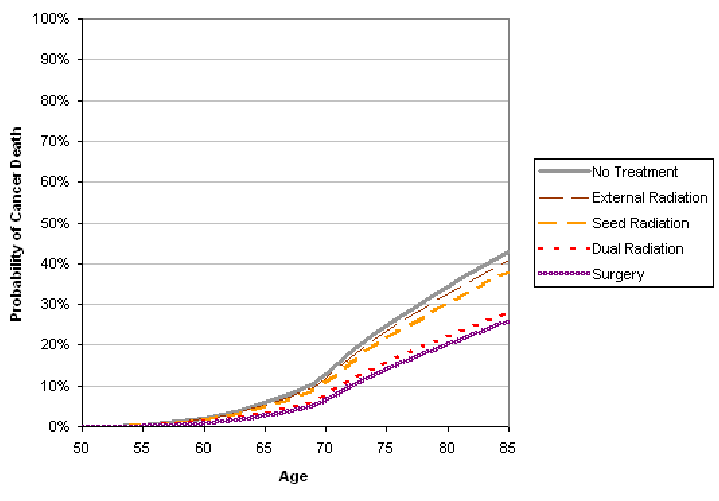
While most men undergo some form of treatment for their prostate cancer, some men today choose to not be treated for their prostate cancer. Instead, they may choose to have their doctors monitor their cancer.
Known as active surveillance, it is common when the cancer is expected to grow slowly based on biopsy results, confined to the prostate, not causing any symptoms, and/or small. In active surveillance, doctors will initiate cancer treatment only if cancer starts growing.
Others men may choose to not undergo cancer treatment because of a short life expectancy or other serious medical problems. They may feel that the risks or side effects of cancer treatment outweigh their potential benefits.
This option is certainly OK and reasonable in the right circumstancesrequiring a careful and thoughtful discussion with your doctor and family.
Read Also: Is Cranberry Juice Good For Prostate Infection
Myth: Prostate Cancer Isn’t Deadly
Fact:;While the five-year survival rate with prostate cancer is very high 90 percent, according to the ACS its still the second leading cause of cancer death in men. The only cancer that kills more men is lung cancer.
Most prostate cancers are what doctors call indolent, which means that they grow slowly and can often be actively monitored over the course of many years without other treatment. But sometimes prostate cancer is aggressive, and grows quickly.
While most men dont have a prostate cancer thats fast and deadly, acknowledges Sartor, it does exist. And you wont know which type you have until its thoroughly checked out.
In other words, assuming prostate cancer isnt serious and not having further testing because of this misconception could be a downright deadly way of approaching the illness.
The dangers and risks of prostate cancer arent distributed evenly among American men, either. The U.S. Department of Health and Human Services Office of Minority Health reports that African-American men are 2.3 times as likely to die from prostate cancer as compared to non-Hispanic white men.
Who Gets This Cancer
Prostate cancer occurs only in men, and it is more common in older men than younger men. It is more likely to occur in men with a family history of prostate cancer and men of African American descent. The rate of new cases of prostate cancer was 111.3 per 100,000 men per year based on 20142018 cases, age-adjusted.
Rate of New Cases per 100,000 Persons by Race/Ethnicity: Prostate Cancer
Males
SEER 21 20142018, All Races, Males
Recommended Reading: Prostate Cancer Ruined My Marriage
What Are The Stages Of Prostate Cancer
Cancer staging is first described using what is called a TNM system. The “T” refers to a description of the size or extent of the primary, or original, tumor. “N” describes the presence or absence of, and extent of spread of the cancer to lymph nodes that may be nearby or further from the original tumor. “M” describes the presence or absence of metastases — usually distant areas elsewhere in the body other than regional lymph nodes to which the cancer has spread. Cancers with specific TNM characteristics are then grouped into stages, and the stages are then assigned Roman numerals with the numerals used in increasing order as the extent of the cancer being staged increases or the cancer prognosis worsens. Prognosis is finally reflected by considering the patient’s PSA score at presentation as well as their Gleason score in assigning a final stage designation.
The American Joint Commission on Cancer system for prostate cancer staging is as follows:
Traditionally, advanced prostate cancer was defined as disease that had widely metastasized beyond the prostate, the surrounding tissue, and the pelvic lymph nodes and was incurable. However, a more contemporary definition includes patients with lower grade disease with an increased risk of progression and/or death from prostate cancer in addition to those with widely metastatic disease.
The National Cancer Institute and the National Comprehensive Cancer Network guidelines on prostate cancer version 2.2017 indicate the following:
What Is A Normal Psa Test Result
There is no specific normal or abnormal level of PSA in the blood, and levels may vary over time in the same man. In the past, most doctors considered PSA levels of 4.0 ng/mL and lower as normal. Therefore, if a man had a PSA level above 4.0 ng/mL, doctors would often recommend a prostate biopsy to determine whether prostate cancer was present.
However, more recent studies have shown that some men with PSA levels below 4.0 ng/mL have prostate cancer and that many men with higher levels do not have prostate cancer . In addition, various factors can cause a mans PSA level to fluctuate. For example, a mans PSA level often rises if he has prostatitis or a urinary tract infection. Prostate biopsies and prostate surgery also increase PSA level. Conversely, some drugsincluding finasteride; and dutasteride;, which are used to treat BPHlower a mans PSA level. PSA level may also vary somewhat across testing laboratories.
Another complicating factor is that studies to establish the normal range of PSA levels have been conducted primarily in populations of White men. Although expert opinions vary, there is no clear consensus regarding the optimal PSA threshold for recommending a prostate biopsy for men of any racial or ethnic group.
In general, however, the higher a mans PSA level, the more likely it is that he has prostate cancer. Moreover, a continuous rise in a mans PSA level over time may also be a sign of prostate cancer.
Read Also: Flomax No Ejaculation
A Look At Prostate Stem Cells
Its now possible to ask whether there are factors that mark high-risk tumors early on. Garraway compares these tiny samples of metastatic tumor cells to non-cancerous prostate tissue, hoping they can provide a clue as to the cause of the formers aggressive behavior.
She does this by focusing on the stem cells normally found in the prostate, which can generate any cell type in this tissue . But stem cells show up in prostate tumors, too. Garraway hypothesizes that these prostate-specific stem cells might have features that make tumors more dangerous. Comparing the genes that are active in both prostate stem cells and cancers gave us ideas about how these more aggressive cancers are co-opting benign stem cell traits. The stem cells primitive embryonic-type properties can facilitate infestation and spreading, she says.
Because prostate stem cells can generate new glands, theyre really good at moving around and invading other parts of the body. And theyre more hardy. They can survive things differentiated cells cant survive, Garraway says. Theyre resistant to radiation and chemotherapy, and they can survive damage to their DNA. We think activating these survival mechanisms supports tumor initiation.
This research is still in the very early stages. Garraway calls it an example of how research and discovery is done, but it shouldnt be considered a potential new therapy for now.
Who Is At Risk For Prostate Cancer
All men are at risk for prostate cancer, but African-American men are more likely to get prostate cancer than other men.
All men are at risk for prostate cancer. Out of every 100 American men, about 13 will get prostate cancer during their lifetime, and about 2 to 3 men will die from prostate cancer.
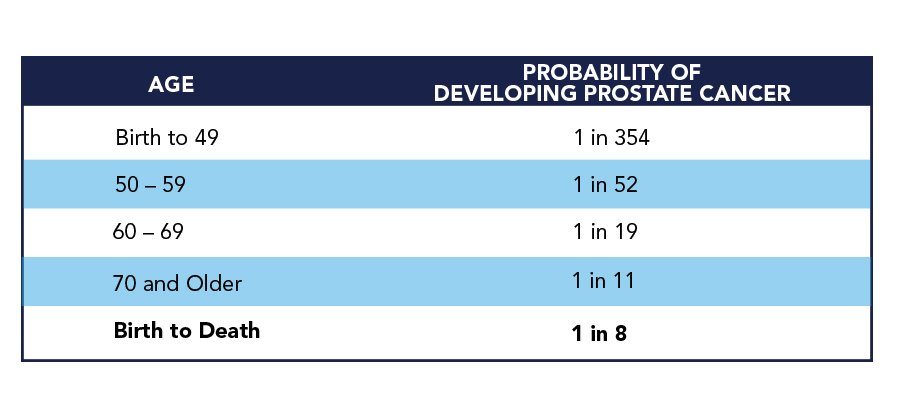
The most common risk factor is age. The older a man is, the greater the chance of getting prostate cancer.
Some men are at increased risk for prostate cancer. You are at increased risk for getting or dying from prostate cancer if you are African-American or have a family history of prostate cancer.
Don’t Miss: Female Equivalent Of Prostate
Are Older Men Undertreated
Schwartz and colleagues reviewed the treatment decisions and factors influencing them in a cohort of men with localized prostate cancer. Age, comorbidity, and Gleason score were found to be independent predictors of suboptimal treatment. It was concluded that most men older than 70 years with moderately or poorly differentiated tumors and no to mild comorbidity were given suboptimal treatment. Most of these men were undertreated, receiving watchful waiting therapy when potentially curative therapy could have been applied. With optimal treatment, clinical outcomes could have been improved.
Thompson and colleagues investigated otherwise healthy octogenarians diagnosed with prostate cancer who underwent radical prostatectomy. At the last follow-up visit, 10 patients had survived more than a decade after surgery, and 3 patients had died within 10 years of surgery. The remaining 6 patients were alive at less than 10 years of follow-up. Seventy-four percent of patients were continent. No patient had died of prostate cancer, and the 10-year, all-cause survival rate was similar to that observed in healthy patients 60 to 79 years old undergoing radical prostatectomy. These findings indicate that careful selection of patients even older than 80 years can achieve satisfactory oncologic and functional outcomes after surgery. It is important to note, however, that the rate of urinary incontinence after surgery exceeds that of younger counterparts.
Understanding The Underlying Causes
For cancer researchers in general, were always seeking out the origins. Where does it start, what cells does it start in, how is it co-opting the processes of normal cells to evade the immune system or invade areas where it shouldnt be? says UCLAs Dr. Garraway. Just like other cancers, the whole idea is to understand the biology of the prostate tumors better so you can find the Achilles heel of that tumor.
The challenge, Garraway tells Ars, is that for a long time, research into what causes prostate cancer growth was focused on the indolent versions of the disease that were curable. More surgeries removed slow-growing tumors, leaving researchers with more access to these tissue samples. Metastatic patients were less likely to undergo surgery because their cancers had spread to other parts of their body, so those samples were studied less often.
For those 10 percent or so who are destined to have this metastatic disease, at least half of them already had spreading of their cancer at diagnosis, she says. They werent surgical candidates, so we werent capturing their tissues. And its a challenge to get enough tissue from a metastatic lesion.
Recommended Reading: Bph And Sexuality
How Does Prostate Cancer Kill You In The End
Prostate cancer is the most common cancer after skin cancer in men in the US and the second leading cause of cancer death. Prostate-specific antigen testing has made the detection of prostate cancer easier in its early stages. Ninety-two out of 100 men get diagnosed when the cancer is limited to the prostate.
Most men are diagnosed with prostate cancer in their senior years; and only 1 out of 36 men die from it. Death from prostate cancer most often happens when cancer has spread to other organs in the body. This is known as the advanced stage of prostate cancer.
The chances of survival decrease as cancer spreads beyond the prostate. If cancer has metastasized to other parts of the body, only three out of 10 men will survive for five years after the diagnosis.
Advanced stage prostate cancer or metastasized prostate cancer
Cancerous cells may spread to organs other than the site of origin. In the case of prostate cancer, this tendency is decreased, but it can happen. Advanced stage prostate cancer is defined based on the Gleason score, which is based on the TNM staging of cancer. T stands for tumor size, N stands for lymph node involvement and M stands for metastasis.
Prostate cancer can kill in the end through metastases that can develop in
Metastasis to the liver can affect the livers ability to filter out toxins from the body. This can eventually lead to jaundice, nausea, loss of appetite and weight loss.
What Is The Outlook For Prostate Cancer
The good news is, rates of prostate cancer have dropped considerably in the United States. The National Cancer Institute reports that in 1992 there were 234 new cases for every 100,000 Americans; now that figure is under 100 per 100,000. Overall, the American Cancer Society projects 164,690 new cases of prostate cancer in 2018 and 29,430 deaths. From a male US population of 161 million, that’s a tiny .02 percent chance of dying from prostate cancer in a given year. Of course, the figures change as you narrow the population based on factors like age, and risk factors like smoking, being overweight and not getting proper exercise. The ACS estimates that 1 in 9 American males will be diagnosed in their lifetime with prostate cancer, and 1 in 41 will die of the disease.
Recommended Reading: What Happens To The Prostate Later In Life
Deaths From Prostate Cancer
Prostate cancer is the second leading cause of cancer death in American men, behind only lung cancer. About 1 man in 41 will die of prostate cancer.
Prostate cancer can be a serious disease, but most men diagnosed with prostate cancer do not die from it. In fact, more than 3.1 million men in the United States who have been diagnosed with prostate cancer at some point are still alive today.
Our team is made up of doctors and;oncology certified nurses with deep knowledge of cancer care as well as journalists, editors, and translators with extensive experience in medical writing.
American Cancer Society. Facts & Figures 2021. American Cancer Society. Atlanta, Ga. 2021.
National Cancer Institute. SEER Cancer Stat Facts: Prostate Cancer. Accessed at https://seer.cancer.gov/statfacts/html/prost.html on March 15, 2019.
Noone AM, Howlader N, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA . SEER Cancer Statistics Review, 1975-2015, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2015/, based on November 2017 SEER data;submission, posted to the SEER web site, April 2018.
American Cancer Society. Facts & Figures 2021. American Cancer Society. Atlanta, Ga. 2021.
National Cancer Institute. SEER Cancer Stat Facts: Prostate Cancer. Accessed at https://seer.cancer.gov/statfacts/html/prost.html on March 15, 2019.
Last Revised: January 12, 2021
Genetic Testing For Prostate Cancer
You may hear a lot about genetics or genomics. Both terms are related to genes and cell DNA, but they are different. These tests are being used to learn more about the DNA of cancer cells, and link DNA mutations with treatments. In the future, genetic testing may be the first step doctors take when diagnosing prostate cancer.
Recommended Reading: Prostaglandins Erectile Dysfunction
Staging Spread And Survival Rates
As with all cancers, doctors use the term stage to describe the characteristics of the primary tumor itself, such as its size and how far prostate cancer has spread when it is found.
Staging systems are complicated. The staging system for most cancers, including prostate cancer, uses three different aspects of tumor growth and spread. It’s called the TNM system, for tumor, nodes, and metastasis:
- T, for tumor describes the size of the main area of prostate cancer.
- N, for nodes, describes whether prostate cancer has spread to any lymph nodes, and how many and in what locations.
- M, for metastasis, means distant spread of prostate cancer, for example, to the bones or liver.
Using the TNM system, each man’s prostate cancer can be described in detail and compared to other men’s prostate cancer. Doctors use this information for studies and to decide on treatments.
As far as survival rates for prostate cancer go, however, the staging system is pretty simple. As we’ve mentioned, in terms of survival rates, men with prostate cancer can be divided into two groups:
Lifetime Risk Of Developing Or Dying From Cancer
The lifetime risk of developing or dying from cancer refers to the chance a person has, over the course of his or her lifetime , of being diagnosed with or dying from cancer. These risk estimates are one way to measure of how widespread cancer is in the United States.
The following tables list lifetime risks of developing and dying from certain cancers for men and women in the US. The information is from the National Cancer Institutes Surveillance Epidemiology and End Results database, and is based on incidence and mortality data for the United States from 2014 through 2016, the most recent years for which data are available.
The risk is expressed both in terms of a percentage and as odds.
- For example, the risk that a man will develop cancer pf the pancreas during his lifetime is 1.66%. This means he has about 1 chance in 60 of developing pancreatic cancer .
- Put another way, 1 out of every 60 men in the United States will develop pancreatic cancer during his lifetime.
These numbers are average risks for the overall US population. Your risk may be higher or lower than these numbers, depending on your particular risk factors.
Don’t Miss: Does An Enlarged Prostate Affect A Man Sexually
