Mri And Targeted Biopsy As Accurate As Current Standard For Prostate Cancer Diagnosis
Results from the phase 3 PRECISE trial showed that MRI with targeted biopsies matched or exceeded the accuracy of the current standard for detecting clinically significant prostate cancer.
Results from the phase 3 Prostate Evaluation for Clinically Important Disease: MRI vs Standard Evaluation Procedures trial showed that MRI with targeted biopsies matched or exceeded the accuracy of the current standard for detecting clinically significant prostate cancer.1
The current standard, a systematic 12-core transrectal ultrasound-guided biopsy , can potentially lead to overdiagnosis in low-risk prostate cancer and underdiagnosis in some cases of higher risk prostate cancer.2 Repeat biopsies, overtreatment of insignificant disease, and delayed or misdiagnosis of clinically significant disease can result.
Authors of the new study, which was published in JAMA Oncology, aimed to find out whether MRI-TBxonly targeting lesions with a Prostate Imaging Reporting and Data System version 2.0 score of 3 or greaterwould be noninferior to the 12-core TRUS-Bx in detecting International Society of Urological Pathology grade group 2 or greater prostate cancer.
The study included biopsy-naïve patients suspected of having prostate cancer who were told to undergo a biopsy. Criteria included:
References
2. Churukanti G, Siddiqi MM.MRITRUS fusion biopsy versus 12-core systematic biopsy. Nat Rev Urol. Published online June 16, 2015. doi:10.1038/nrurol.2015.143
Imaging Tests For Prostate Cancer
Imaging tests use x-rays, magnetic fields, sound waves, or radioactive substances to create pictures of the inside of your body. One or more imaging tests might be used:
- To look for cancer in the prostate
- To help the doctor see the prostate during certain procedures
- To look for spread of prostate cancer to other parts of the body
Which tests you might need will depend on the situation. For example, a prostate biopsy is typically done with transrectal ultrasound and/or MRI to help guide the biopsy. If you are found to have prostate cancer, you might need imaging tests of other parts of your body to look for possible cancer spread.
The imaging tests used most often to look for prostate cancer spread include:
What Is A Prostate Biopsy
There are two main types of prostate biopsies transrectal ultrasound guided biopsies and transperineal biopsies. As the former tends to be more common, well focus on this method.
biopsies use ultrasound guidance with a biopsy tool to snip core samples from the prostate gland. An ultrasound probe and biopsy tool are introduced into the rectum where a biopsy needle penetrates the rectal wall and enters the prostate. The procedure is repeated up to 12 times.
Transrectal prostate biopsies are outpatient or in-office procedures that require only numbing medicine. Passing a needle through the rectum and into the prostate places you at risk of infection. To minimize the risk of infection, urologists commonly prescribe antibiotics beforehand.
Other complications from prostate biopsies include:
- Blood in urine, semen, and stool
- Pain
You May Like: Does Enlarged Prostate Affect Ejaculation
Diagnosing Clinically Significant Rather Than Advanced Prostate Cancer
The spectrum effect tells us that using evidence from PSA screening or LUTS survey data from the general population to inform diagnostic practice in primary care may not result in the right answer, and possibly leads to the wrong question .
Studies including populations of men with LUTS attending primary care, not cited in Jákupsstovu and Brodersens insightful article about the perils of prostate cancer overdiagnosis in men with LUTS , show that men who attend their GP with LUTS are at a higher risk of prostate cancer than those who dont . They show that men attending primary care with LUTS are at higher risk of prostate cancer than asymptomatic screened men or men from the general population asked if they suffer LUTS. The difference is the higher prior odds of prostate cancer in men visiting their GP with LUTS: men who choose to visit their GP with LUTS are different from those that dont. Whilst the risk may be higher, these studies do not document the method used to assess the LUTS present or differentiate clinically significant from non-significant cancers. They are reliant on routinely collected primary care records data without linkage to stage and grade information from the cancer registry.
Dr Brian D Nicholson GP, Clinical Researcher, University of Oxford.Dr Samuel W D Merriel, NIHR Academic Clinical Fellow in General Practice, Honorary Lecturer, University of Bristol.
Competing interests: No competing interests
06 May 2018
Will The Mri Be Done With An Endorectal Coil Or An External Pelvic Coil
Some radiology practices use an endorectal coil a probe-like device covered with latex which is inserted into the rectum and helps provide high-quality images of the prostate. With a newer, high-quality MRI system, endorectal coils are not necessary and an external pelvic coil can be used instead, eliminating patient discomfort while maintaining high quality images.
Recommended Reading: Does An Enlarged Prostate Affect A Man Sexually
What Is An Mri
What makes an MRI different from other medical imaging techniques like X-rays and CT scans? X-rays take projection images of hard tissues like bones, while CT scans take images of both hard bony tissues and soft tissue. Both systems use ionizing radiation, which passes through the body to create images that are transferred to photographic film or to a video monitor.
An MRI works differently. Magnetic resonance imaging uses a magnetic field to create sound waves that are received, digitized, and displayed in real-time. When tissue is abnormal, its composition changes, so the images reflect damaged areas.
Overlap With Benign Conditions
MRI derived parameters are reflective of pathologically determined characteristics of prostate cancer, however, there is great overlap with benign conditions, such as benign prostate hyperplasia, inflammation or fibrosis. These benign abnormalities have been implicated as sources of false-positive MR imaging findings or poor radiologic-pathologic volumetric correspondence . These issues are at most applicable to PI-RADS 3 lesions, as shown by the high rate of benign outcomes of targeted biopsies: prostate cancer was not detected in respectively 61% and 71% in men with first biopsies and previous negative biopsies .
Don’t Miss: What Is The Definition Of Prostate
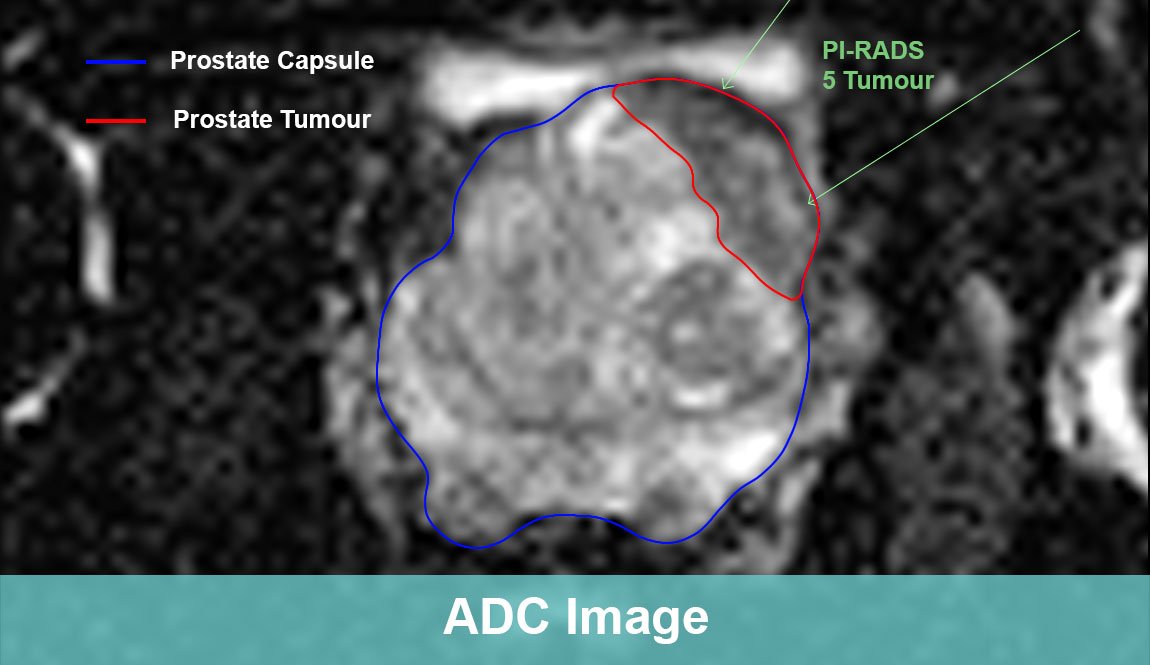
What Is A Pi
In a PI-RADS category 3 lesion, the presence of csPCa is considered to be equivocal, as defined by the PI-RADS v2 guidelines . For lesions located in the peripheral zone of the prostate, the dominant MRI sequence in PI-RADS v2 is DWI and reconstructed apparent diffusion coefficient . Lesions are characterized as focal mildly to moderately hypointense on ADC, and isointense to mildly hyperintense on high b-value DWI. This is in combination with heterogeneous signal intensity or non-circumscribed, rounded, and moderate hypointensity on T2w images, and specifically excludes lesions with characteristics that qualify as PI-RADS 2, 4, or 5. No focal enhancement on DCE MRI should be visualized .
Figure 1
For lesions located in the transition zone, the dominant sequence in PI-RADS v2 is T2w sequence . Signal intensity in a lesion should be visually compared to the average signal of normal transition zone. Lesions are characterized as heterogeneous signal intensity with obscured margins , together with focal mildly to moderately hypointense on ADC, and isointense to mildly hyperintense on high b-value DWI. Focal enhancement on DCE MRI may be present .
Figure 2
Magnetic Resonance Imaging And Pre
The MRI protocol included T2-weighted imaging , diffusion-weighted imaging from which apparent diffusion coefficient maps were constructed, and dynamic contrast-enhanced imaging, according to the PI-RADS v2 guidelines . Detail of acquisition parameters are presented in the supplementary material . MRI was performed on a 3-T system using a 32-channel pelvic phased-array coil. All MRIs were reviewed by one urogenital radiologist with over 6 years of prostate MRI experience. Individual lesions were scored according to the PI-RADS v2 5-point Likert scale for high-grade PCa. Visible MRI lesions with a PI-RADS score from 3 to 5 were defined as suspicious and delineated. The fusion technique of MRI and TRUS was used to perform targeted biopsies of all suspicious lesions, identified on MRI. The suspicious MRI lesions, delineated on DICOM images, were targeted with a maximum of four cores under ultrasound guidance. Experienced operators performed the biopsy procedures. One expert uropathologist reviewed biopsy specimens according to the ISUP 2014 modified Gleason Score .
Read Also: Ejaculation Problems With Tamsulosin
What Combined Strategies In Pi
In the setting of suspicious imaging findings, it is accepted that MRI cannot negate the need for biopsy. Histopathological proof by targeted biopsies is necessary due to the high false-positive rate of MRI . If additional information can help to clarify further risk of suspicious lesions on MRI, the number of biopsies and false positive results can be reduced. Several strategies of combining additional information to MR imaging are under investigation. They may demonstrate a benefit in making a decision about which patient needs a biopsy and concurrently help avoid unnecessary biopsies. Studies on the added value in classifying further risk of PI-RADS category 3 lesions are limited.
Citation Doi And Article Data
Citation:DOI:Dr Marcin CzarnieckiRevisions:see full revision historySystems:
- Prostate Imaging Reporting and Data System version 2.1
- PI-RADS version 2.1
- Prostate Imaging Reporting and Data System
- PIRADS
- PI-RADS
PI-RADS is a structured reporting scheme for multiparametric prostate MRI in the evaluation of suspected prostate cancer in treatment naive prostate glands. This article reflects version 2.1 , published in 2019 and developed by an internationally representative group involving the American College of Radiology , European Society of Urogenital Radiology , and AdMeTech Foundation 6.
Recommended Reading: Is Zinc Good For Prostate
Medical History And Physical Exam
If your doctor suspects you might have prostate cancer, he or she will ask you about any symptoms you are having, such as any urinary or sexual problems, and how long you have had them. You might also be asked about possible risk factors, including your family history.
Your doctor will also examine you. This might include a digital rectal exam , during which the doctor inserts a gloved, lubricated finger into your rectum to feel for any bumps or hard areas on the prostate that might be cancer. If you do have cancer, the DRE can sometimes help tell if its only on one side of the prostate, if its on both sides, or if its likely to have spread beyond the prostate to nearby tissues. Your doctor may also examine other areas of your body.
After the exam, your doctor might then order some tests.
Also Check: Will Bacterial Prostatitis Go Away
Genenutrient Interaction In Prostate Cancer
Genetic studies have identified susceptibility genes for familial prostate cancer, which encode an interferon-inducible ribonuclease and subunits of the macrophage scavenger receptor. Somatic silencing of a glutathione S-transferase , capable of defending against oxidant cell and genome damage, has been found in almost all prostate cancer cases. Proliferative inflammatory atrophy lesions are found adjacent to prostatic intraepithelial neoplasia and carcinoma in situ. These PIA lesions contain activated inflammatory cells, and proliferating epithelial cells appear likely to be precursors to prostatic intraepithelial neoplasia lesions and prostatic carcinomas. Emerging hints that prostate inflammation may contribute to prostatic carcinogenesis provide additional research directions for examining the effects of diet and exercise, altering dietary patterns, or adding antioxidant nutrients to the diet.
Nutritional Factors
Obesity and Prostate Cancer
The association of obesity with prostate cancer is somewhat controversial, most likely due to misassignment of body mass index and prostate cancer. In one study among men in China, it was found that men in the highest quartile of waist-to-hip ratio had an almost threefold increased risk for developing prostate cancer, suggesting a relationship to metabolic syndrome and insulin resistance, as discussed later in this chapter .
Mohsen Beheshti, … Werner Langsteger, in, 2018
Recommended Reading: Is Zinc Good For The Prostate
Developing Timely Care For Prostate Cancer Patients With A Pi
Patients who receive an intermediate score of the Prostate Imaging Reporting and Data System scale, or PI-RADS 3, have a substantial chance of developing clinically significant prostate cancer, new research shows.
However, PI-RADS v2 doesnt provide guidelines to aid in clinical decision-making for patients with intermediate scores, making it more difficult to develop a timely plan for care, said Fatima Salah, MD, a clinical fellow at Brigham and Womens Hospital in Boston, and colleagues in her RSNA 2020 session, Understanding Prostate MR PI-RADS 3: A Longitudinal Study.
Those patients are more challenging, Dr. Salah said. PI-RADS 3 is a common category but its problematic because there are no specific guidelines for what the next steps should be.
PI-RADS is used to standardize interpretation of prostate MRI, improve early diagnosis and treatment, and reduce unnecessary biopsies. In the PI-RADS scale, each lesion is assigned a score from 1 to 5 indicating the likelihood of clinically significant cancer.
PI-RADS 1: clinically significant cancer is highly unlikely to be present
PI-RADS 2: clinically significant cancer is unlikely to be present
PI-RADS 3: the presence of clinically significant cancer is equivocal
PI-RADS 4: clinically significant cancer is likely to be present
PI-RADS 5: clinically significant cancer is highly likely to be present
FATIMASALAH, MD
PI-RADS 3 Patients Require Plan for Care Management
For More Information
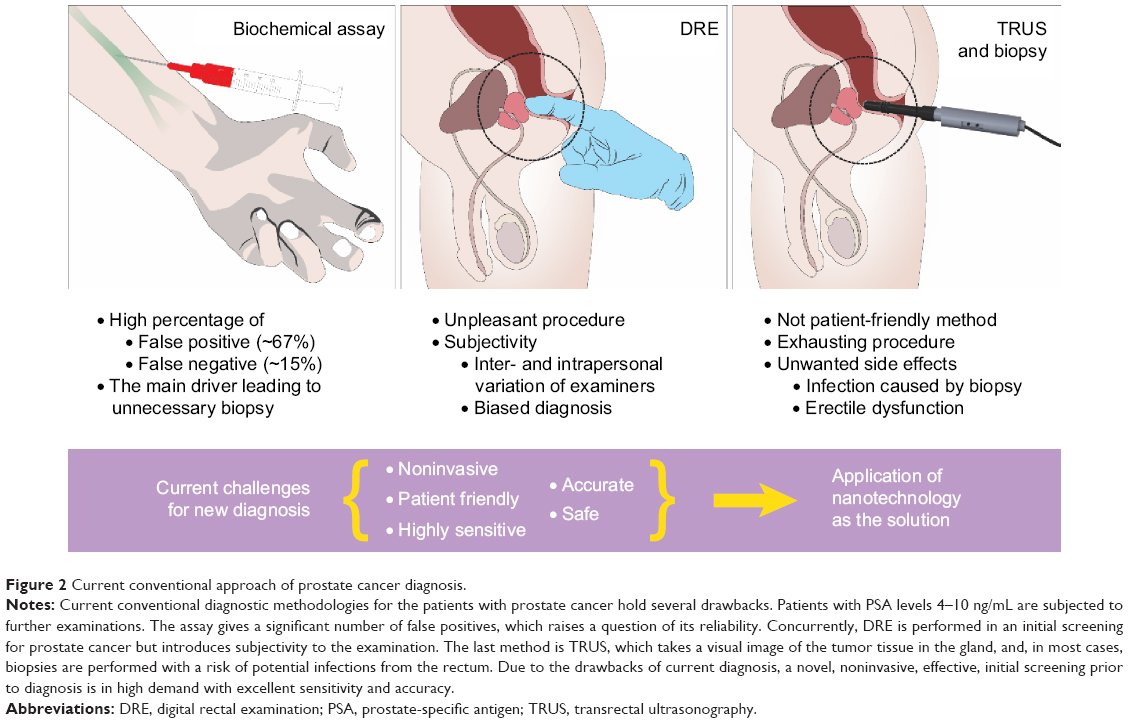
Diagnosis Of Prostate Cancer
When a digital rectal exam or a PSA test reveal abnormal results, the next step is further testing to determine whether prostate cancer is present, or another cause may be to blame.
Your doctor will evaluate your test results and any symptoms you may be experiencing and recommend the next tests you may need. The most common diagnostic tests for the prostate include:
Ultrasound: A transrectal ultrasound involves inserting a small ultrasound probe into the rectum. The ultrasound machine sends out sound waves and then measures the echoes that bounce back off body structures to create an image of the landscape of the structure. It can provide images that show the extent of prostate enlargement or abnormalities.
MRI: Magnetic resonance imaging is sometimes used to create a more detailed set of images than an ultrasound can provide. Results will be reported as a PI-RADS score.
- PI-RADS 1: very lowclinically significant cancer is highly unlikely to be present
- PI-RADS 2: lowclinically significant cancer is unlikely to be present
- PI-RADS 3: intermediatethe chance of clinically significant cancer is neutral
- PI-RADS 4: highclinically significant cancer is likely to be present
- PI-RADS 5: very highclinically significant cancer is highly likely to be present
Regardless of which procedure is used to take a sample, the prostate tissue is then examined under a microscope by a pathologist, to confirm the presence or absence of cancerous cells.
Also Check: Prostate Cancer Osteoblastic Or Osteolytic
Getting The Results Of The Biopsy
Your biopsy samples will be sent to a lab, where they will be looked at with a microscope to see if they contain cancer cells. Getting the results usually takes at least 1 to 3 days, but it can sometimes take longer. The results might be reported as:
- Positive for cancer: Cancer cells were seen in the biopsy samples.
- Negative for cancer: No cancer cells were seen in the biopsy samples.
- Suspicious: Something abnormal was seen, but it might not be cancer.
If the biopsy is negative
If the prostate biopsy results are negative , and the chance that you have prostate cancer isnt very high based on your PSA level and other tests, you might not need any more tests, other than repeat PSA tests sometime later.
But even if many samples are taken, biopsies can still sometimes miss a cancer if none of the biopsy needles pass through it. This is known as a false-negative result. If your doctor still strongly suspects you have prostate cancer , your doctor might suggest:
- Getting other lab tests to help get a better idea of whether or not you might have prostate cancer. Examples of such tests include the Prostate Health Index , 4Kscore test, PCA3 tests , and ConfirmMDx. These tests are discussed in Whats New in Prostate Cancer Research?
- Getting a repeat prostate biopsy. This might include getting additional samples of parts of the prostate not biopsied the first time, or using imaging tests such as MRI to look more closely for abnormal areas to target.
Prostate cancer grade
Gleason score
Should We Redefine Pi
PI-RADS v2 seeks to define the five assessment categories in a way that maintains a balance between achieving high sensitivity for GS 7 tumors and avoiding an excessive number of biopsies that are benign or harbor low-grade tumor. Criteria for upgrading a lesions assigned category, based on combinations of multiple suspicious findings, are intended to help improve the sensitivity of individual PI-RADS assessment categories for csPCa. As such, for a lesion located in the peripheral zone, the assessment category matches the score assigned based on DWI, regardless of the assessment based on other pulse sequences. However, if the lesion is assigned with PI-RADS category 3 and the DCE score is also positive, than the overall category should be upgraded from 3 to 4 .
Table 2et al.
Read Also: Perineural Invasion Prostate
Prostate Mri Can Help Differentiate Between Harmless And Aggressive Cancers Preventing The Overdiagnosis Of Low
There are two forms of prostate cancer: aggressive and harmless. Fortunately, out of all prostate cancer cases, only a fraction will be aggressive and clinically significant. The majority will never impact the well-being or life expectancy of a patient.
Prostate MRI can help reduce the number of men who are over-diagnosed by 5%.
A prostate MRI scan enables radiologists to better differentiate between aggressive and harmless cancers by providing information about a tumors size, density, and proximity to the bloodstream. One study comparing prostate MRI to biopsy found MRI scans to correctly diagnose 93% of tumors, whereas biopsy correctly diagnosed only 48%. Identifying non-threatening forms of prostate cancer helps decrease the risk of overdiagnosis and overtreatment.
But do keep in mind that MRIs can be complex images for radiologists to interpret. Coupling a prostate MRI with a subspecialty second opinion from a fellowship-trained radiologist can help maximize the advantages and efficacy of the screening. This can be done completely online and is especially recommended for scans that indicate the possibility of aggressive prostate cancer.
CONNECT WITH A SPECIALIST
Take Charge of Your Health
Get a second opinion from a radiology specialist in 3 easy steps.
