Excision Of The Neurovascular Bundle At Radical Prostatectomy In Cases With Perineural Invasion On Needle Biopsy
Holmes GF, Walsh PC, Pound CR, Epstein JI.
Urology. 1999;53:752756 .
Holmes and colleagues retrospectively reviewed 80 men, all with PNI on prostate needle biopsy, who subsequently underwent radical prostatectomy with or without neurovascular bundle excision. The presence and location of extraprostatic extension and margin status, presence of seminal vesicle invasion, lymph node metastasis, neurovascular bundle status, and location of extraprostatic tumor were evaluated. Extraprostatic extension was present in 62 of these men with biopsy PNI, compared with 36% of all the men undergoing radical prostatectomy at the same institution over the same period.
Several conclusions can be drawn from the data of Holmes and associates. PNI does seem to confer an increased risk of extraprostatic extension of tumor. However, in a previous study, Epstein and associates found that men with isolated extraprostatic extension at radical prostatectomy had a 41% to 77% likelihood of biochemical recurrence- free survival a decade after surgery. Thus, the increased extraprostatic tumor extension posed by the presence of biopsy PNI should not serve as a contraindication to radical prostatectomy.
Radiation Of Drg Decreases Gdnf Secretion
Conditioned media from radiated DRG was collected 8 days following radiation exposure and assayed for GDNF. Single-fraction doses from 416 Gy decreased measured GDNF to undetectable levels as compared with non-radiated DRG . The assay limit of detection was 31 pg/mL.
The reduction of PNI resulting from radiation of DRG was partially rescued with the direct addition of GDNF to the DRG-Matrigel complex. Using the DRG-cancer co-culture assays, non-radiated DRG yielded a mean area of invasion of 170,000 microns2, while exposure of DRG to 4 Gy completely inhibited any measurable area of invasion at day 8. The addition of purified GDNF to the DRG-Matrigel complex resulted in a partial rescue, with a mean area of invasion of 73,000 microns2 . The lack of a full rescue of PNI with GDNF replacement may be related to the non-physiologic application of the GDNF in these experiments, an inability to recreate a continuous source of endogenous GDNF secretion by the DRG, and potential non-GDNF nerve secreted neurotrophic factors that might be diminished by radiation.
Relationship Between Pni And Other Clinicopathological Parameters
Chi square testing demonstrated that PNI positive patients were significantly more likely to have a higher RP Gleason score, pT3 disease and the presence of positive surgical margin. Similarly, patients with PNI had significantly greater cancer volume on Mann-Whitney U testing. No significant relationship was seen between age or preoperative PSA and PNI .
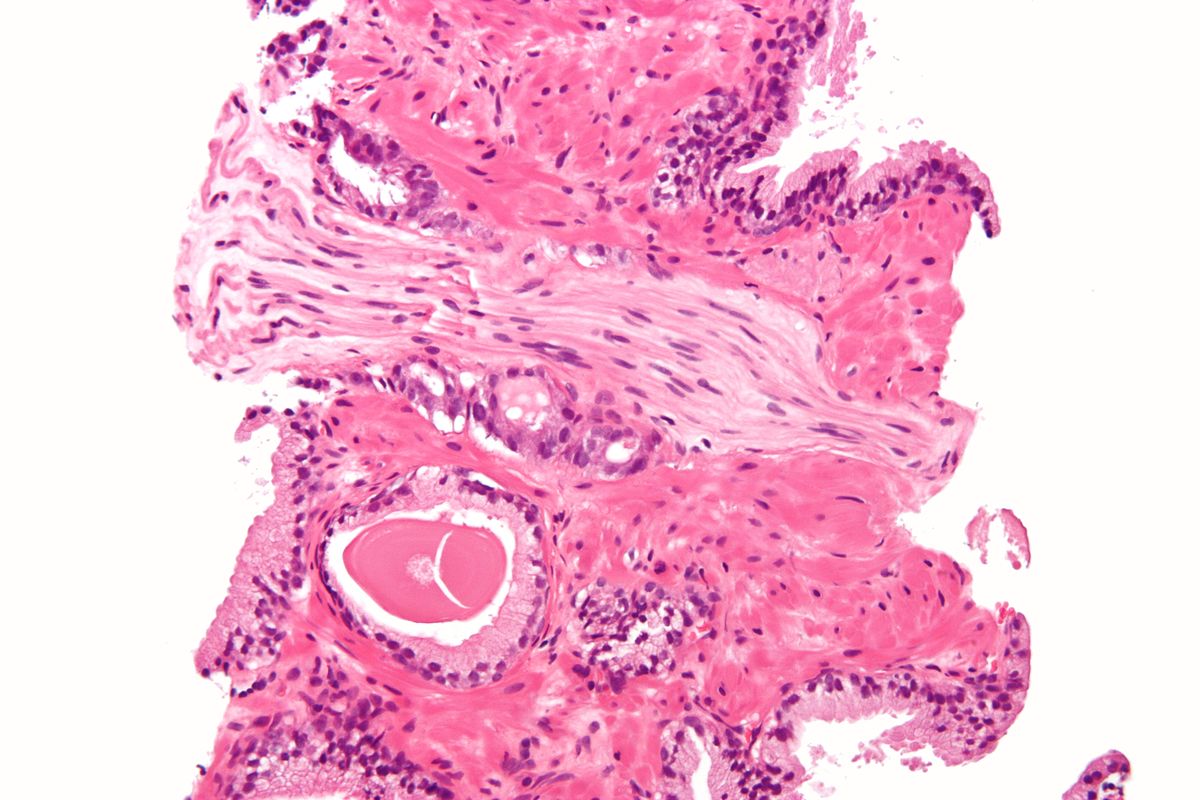
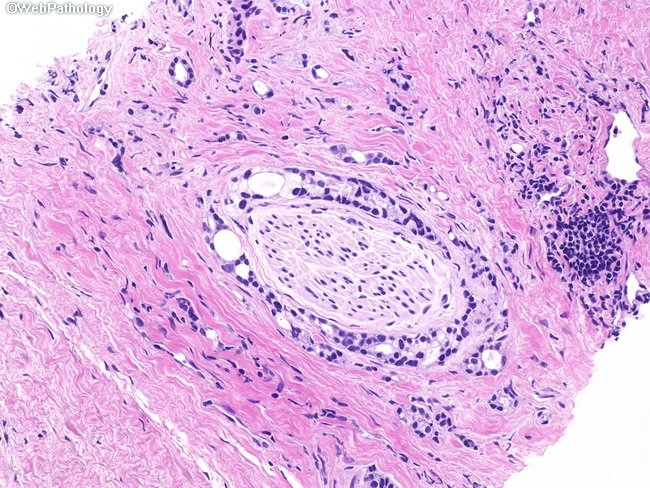
Expression Of Ret In Human Acc Cancer Cells
Radiation is frequently administered to patients with ACC, a salivary gland cancer, following surgical resection because of its high propensity for PNI and local recurrence. We assessed whether patient ACC tumor specimens express RET, the cognate receptor for GDNF, using immunohistochemical staining. Hematoxylin-eosin staining frequently demonstrated well-formed ducts and nests of cells growing in hyalinized stroma in a mixed tubular and cribriform pattern . We identified mild to moderate levels of RET expression in all of the 18 human ACC tumor specimens assessed . The nerves and surrounding stromal tissues did not express RET. These findings suggest that our model of GDNF mediated RET signaling as a mechanism for chemotaxis and PNI may be clinically relevant for patients with ACC.
Question: What Is The Association Of Pni With Extracapsular Tumor Extension** In Our Group Of Radical Prostatectomy Patients
What We Found: Perineural invasion in the biopsy specimen is associated with a significantly greater risk of ECE.
Men with PNI should not be treated with active monitoring, and careful consideration should be given to whether the surgeon should attempt to spare the nerve on the side of the prostate that shows perineural invasion.
In this case, the potential benefits of nerve-sparing surgery should be strongly weighed against the greater risk of ECE.
Pathologists should continue to report this finding in prostate needle biopsy specimens since it has significance for prognosis and can influence treatment recommendation.
Study: From 2003 to 2006, we were able to document the presence or absence of PNI in the biopsy report for 789 radical prostatectomy patients operated on by Dr. Catalona. 127 men had PNI in the biopsy specimen and ECE was reported in 44% of these men. Only 14% of the men without perineural invasion had ECE.
*Small nerve fibers in the prostate gland secrete a growth factor that attracts prostate cancer cells, so when pathologists look at sections of the prostate gland, they frequently see the tumor cells surrounding the nerve fibers. This is called perineural invasion.
Christopher R. Griffin, Chicago, IL; Stacy Loeb, MD, Washington DC; John Cashy, PhD; William J. Catalona, MD, Chicago, IL
Perineural Invasion In A Prostate Biopsy Specimen Is Not The Same As Pni In Prostatectomy Specimen
Background: Many pathologists who examine prostate cancer biopsies believe that perineural invasion* is present in all radical prostatectomy specimens if a careful search is made.
For this reason, some pathologists do not even report the presence or absence of PNI in needle biopsy specimens, thereby not distinguishing a needle biopsy specimen from a prostatectomy specimen.
However, many clinical doctors view the finding of PNI in a biopsy specimen as an adverse feature in prognosis.
The Johns Hopkins group is now excluding men with PNI on biopsy from their active monitoring possibility.
Mri Of Sciatic Nerves
Mice were subjected to magnetic resonance imaging , performed on a Bruker USR 4.7T 40-cm bore scanner equipped with a 400 mT/m 12-cm bore gradient, using a custom-designed active decoupled radiofrequency surface coil . Mice were anesthetized with 1% to 1.5% Isoflurane in oxygen and monitored with an animal physiological monitoring system . A scout fast spin echo scan in three orientations was acquired to localize the sciatic nerve, followed by an oblique-coronal T2-weighted fast spin-echo image acquired with: TR/TE 1.9 s and 40 ms, 117×186 µm in-plane resolution, 20 slices of 0.8 mm slice thickness and 16 averages. Contrast was injected via mouse tail vein 0.1 mmol/kg Gd-DTPA , Magnevist . Oblique-coronal T1-weighted gradient-echo images were acquired continuously prior to and after injection. The acquisition parameters were TR 126 ms, TE 2.2 ms, 156×186 µm in-plane resolution, 12 slices with 0.8 mm slice thickness, 8 averages with a time resolution of 3 minutes.
Imaging Evaluation Of Perineural Tumor Spread
Perineural invasion can be a challenging diagnosis. Whereas it can be recognized clinically with obvious cranial neuropathological conditions, the difficulty comes when diagnosing clinically silent perineural invasion before surgical resection, because it has the potential to alter treatment and patient prognosis. Perineural invasion is the result of tumor spread along the epineurium, allowing for dissemination of the neoplasm throughout the head and neck. These lesions will typically spread anterograde towards the skull base and central nervous system, although retrograde spread is possible, typically occurring at junction points . Occasionally, spread along the epineurium will break out beyond the nerve sheath, causing macroscopic deposits of disease. The extent of perineural invasion may be difficult to assess clinically, radiographically, and surgically because of skip lesions and small rests of tumor cells propagating along small nerves that are easily missed.
When imaging the primary lesion, evaluating the immediate surrounding tissue for any evidence of perineural invasion is crucial because it can provide important prognostic and treatment planning information with inadequate resection, leading to increased risk of recurrence of disease. Given the challenge of identifying direct evidence of perineural invasion, evaluating the muscles of the face, tongue, and palate for atrophy and fatty replacement may be the most reliable method for identifying evidence of disease.
Perineural Invasion And Large Nerve Perineural Spread
PNI is malignant infiltration of the potential space between nerve sheath and axon and occurs in 26% of cSCC and BCC.54 PNI detected incidentally at histopathology is an identified risk factor for recurrence.51 This risk may increase with increasing nerve diameter,55 the number of nerves affected, and how far the PNI extends away from the primary tumor. The presence of clinical symptoms related to the involved nerves and the presence of radiologically detectable disease5457 indicate more advanced PNI disease.
LNPNS is the spread of malignant cells along large nerves both distally, toward the dermis, and proximally, toward the nerve origin in the skull base.58 This most commonly affects branches of the trigeminal and facial nerves. If the patient is medically able to undergo surgery and the disease is potentially resectable, excision with clear margins should be attempted, and this should be followed by adjuvant RT.
For medically inoperable cases, RT may be used alone as definitive treatment and may provide durable control of disease in approximately 50% of cases.56,60
Perineural Invasion And Seminal Vesicle Involvement Predict Pelvic Lymph Node Metastasis In Men With Localized Carcinoma Of The Prostate
Stone NN, Stock RG, Parikh D, et al.
J Urol. 1998;160:17221726 .
In an effort to evaluate the ability of the presence of biopsy PNI to predict a subsequent finding of lymphatic or seminal vesicle involvement by prostate cancer, Stone and associates evaluated 212 men who presented with clinically localized prostate cancer and underwent staging pelvic lymph node dissection. Using univariate and multivariate analyses, the presence of biopsy PNI was correlated with the likelihood of metastatic prostate cancer found on pelvic lymphadenectomy. Stone and colleagues found that biopsy PNI was a better predictor of lymph node metastasis than serum prostate-specific antigen , biopsy Gleason score, or clinical stage. The authors concluded that men with biopsy PNI seeking definitive therapy for clinically localized prostate cancer should be counseled for staging pelvic lymph node dissection before definitive therapy. The potential role of biopsy PNI in predicting an increased likelihood of seminal vesicle invasion or lymphatic metastasis warrants further research. Additional support of the predictive power of PNI for lymphatic metastasis could strengthen the argument for staging lymph node dissection in the large number men with this biopsy finding who choose to undergo brachytherapy or external beam radiotherapy for clinically localized prostate cancer.
Perineural Invasion In Prostate Needle Biopsy Specimens: Correlation With Extraprostatic Extension At Resection
Vargas SO, Jiroutek M, Welch WR, et al.
Am J Clin Pathol. 1999;111:223228 .
Positing that PNI extensive enough to be sampled on needle biopsy may signal an increased risk of extraprostatic extension of cancer, Vargas and associates evaluated the preoperative needle biopsy specimens and corresponding prostates of 340 men who underwent radical prostatectomy between 1995 and 1997 in an attempt to correlate biopsy PNI with extraprostatic tumor extension. PNI was present in 16.7% of these biopsy specimens and correlated with higher Gleason scores and an increased incidence of extraprostatic tumor extension after radical prostatectomy. In this cohort of patients, all presenting after the widespread availability of PSA testing, biopsy PNI had a sensitivity of 32% and specificity of 88% for predicting extraprostatic tumor extension. Biopsy PNI had a positive predictive value of 42% for extraprostatic tumor extension. Using multivariate logistic regression, Vargas and associates found biopsy PNI to independently predict extraprostatic tumor extension. Despite this, when serum PSA was included in the multivariate analysis, PNI provided no additional ability to predict extraprostatic extension on final pathologic analysis.
The Significance Of Perineural Invasion Found On Needle Biopsy Of The Prostate: Implications For Definitive Therapy
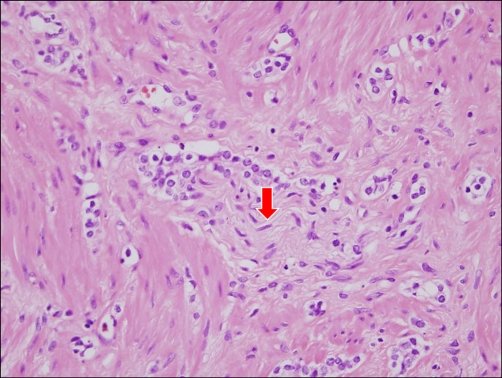
The pathologic assessment of perineural invasion of prostate needle biopsy specimens is relatively reproducible, requires no new technology or equipment, and is relatively inexpensive. The finding of PNI at biopsy has created excitement as a potential preoperative predictor of extraprostatic tumor extension. PNI is defined as the presence of prostate cancer tracking along or around a nerve within the perineural space . Although the finding of PNI on pathologic analysis of a radical prostatectomy specimen has no significance, the importance for treatment planning of PNI found on prostate needle biopsy has been a source of considerable debate. Since PNI is a major mechanism of prostate cancer extension from prostatic parenchyma to periprostatic soft tissue, PNI extensive enough to be sampled on needle biopsy may signal an increased likelihood of extraprostatic extension of cancer or, ultimately, of cancer recurrence.
Prostate needle biopsy specimen showing prostate cancer and perineural invasion with circumferential tumor growth in the perineural space .
Gdnf Production By Drg And Sciatic Nerves
Normal or radiated DRG were grown in 24-well plates for 13 days and the conditioned media removed and centrifuged. Supernatant was assayed for GDNF using an enzyme-linked immunosorbent assay kit .
A single-fraction dose of 8 Gy was administered to the right sciatic nerve as described, with the non-radiated left nerve serving as control. Three weeks following radiation, mice were sacrificed and bilateral sciatic nerves were excised. Identical segments of nerve were removed. The nerves underwent homogenization with an electronic pestle grinder . Tissue lysates were centrifuged and analyzed by GDNF ELISA. Total protein was quantified for each nerve .
Radiation To Cancer Cells Alone Diminishes Pni In Vivo
Radiation to cancer inhibits PNI in our in vitro models predominantly through diminished cell viability, rather than impaired chemotaxis. To assess this concept in vivo, MiaPaCa2 received a single dose of 2 Gy, and 48 hours later were injected into non-radiated sciatic nerves. Compared with non-radiated MiaPaCa2 cells, low doses of radiation to the cancer resulted in diminished invasion on imaging and histopathological analysis at 7 weeks . Hind limb function was significantly improved in animals with radiated MiaPaCa2 cells as compared with controls . Tumor volume at 7 weeks was significantly lower for the radiated MiaPaCa2 cells, compared to non-radiated MiaPaCa2 control cells , suggesting that in vivo cell viability, proliferation, and tumor progression were significantly impaired by a single dose of 2 Gy.
What Does It Mean If My Biopsy Mentions That There Is Perineural Invasion
Perineural invasion means that cancer cells were seen surrounding or tracking along a nerve fiber within the prostate. When this is found on a biopsy, it means that there is a higher chance that the cancer has spread outside the prostate. Still, perineural invasion doesnt mean that the cancer has spread, and other factors, such as the Gleason score and amount of cancer in the cores, are more important. In some cases, finding perineural invasion may affect treatment, so if your report mentions perineural invasion, you should discuss it with your doctor.
Predictors Of Biochemical Recurrence
All clinicopathological variables tested on univariable analysis, except age, were significantly associated with BCR . Of the PNI-negative patients, 9.7% had a BCR, compared to 23.3% of PNI-positive patients . On multivariable Cox regression analysis, PNI failed to retain significance . Variables shown to be independent predictors of BCR were preoperative PSA, cancer volume, RP Gleason score, pT-stage, and surgical margin status.
Probability of biochemical recurrence-free survival stratified by perineural invasion status on univariable analysis.
Understanding Your Pathology Report: Prostate Cancer
When your prostate was biopsied, the samples taken were studied under the microscope by a specialized doctor with many years of training called a pathologist. The pathologist sends your doctor a report that gives a diagnosis for each sample taken. Information in this report will be used to help manage your care. The questions and answers that follow are meant to help you understand medical language you might find in the pathology report from your prostate biopsy.
Perineural Invasion Associated With Increased Cancer
Beard. IJROBP 2006;66:403
The significance of PNI with respect to prognosis after surgery has been inconsistently demonstrated, with some investigators showing a clear risk of upstaging, upgrading, or adverse outcomes in their PNI+ patients, and others showing no effect whatsoever. There is less information on the association between outcomes after RT and PNI, but theavailable data suggest that PNI is associated with unfavorable outcomes after RT. Previously, an unfavorable outcome was defined as freedom from PSA failure. To the best of our knowledge, this is the first report demonstrating a survival decrement in the PNI+ patient population. However, the results must be viewed as preliminary, given the small number of events, relatively short follow-up, and retrospective nature of the analysis.
Purpose: To identify an association between perineural invasion and cancer-specific survival in patients with prostate cancer after standard-dose external beam radiation therapy .
Results: At a median follow-up of 4.5 years, 84 patients have died, 15 of 84 from prostate cancer. PNI was the only significant predictor of prostate cancer-specific mortality after RT . The estimated prostate cancerspecific mortality was 14% at 8 years for PNI+ patients vs. 5% for PNI patients .
Should Perineural Invasion Influence Active Surveillance And Radiation Treatment Options
Perineural invasion is a risk factor detected on a biopsy in 15 to 38 percent of men with a prostate cancer diagnosis. The presence of PNI means that the pathologist saw nerves infiltrated with cancer cells either in the biopsy specimens or later on, in the surgical specimen after a radical prostatectomy.
As they grow, tumors cause nerves to innervate them. The cancer infiltrates in and around small nerves that connect to nerve bundles outside the prostate, becoming a potential route of metastatic spread . The data on whether PNI is independently prognostic for T3 stage after surgery are equivocal, although PNI is often the mechanism for extracapsular extension. After considering Gleason score, PSA, stage, and tumor volume, PNI does not seem to add much to the risk of recurrence after surgery. PNI is not associated with higher surgical margin rates, and it is not considered sufficient to preclude nerve-sparing surgery. An open question is whether it raises risk enough to warrant more aggressive radiation options, like brachy-boost therapy, whole-pelvic radiation, and long-term adjuvant ADT.
Peng et al. retrospectively examined the records of 888 men who were treated with external beam radiation at Johns Hopkins from 1993 to 2007. Of these 888 men, 21 percent had biopsy-detected PNI. Compared to men with no PNI, those with PNI had:
- 33 percent in men not treated with ADT
- 8 percent in men treated with ADT
What Does It Mean When There Are Different Core Samples With Different Gleason Scores
Cores may be samples from different areas of the same tumor or different tumors in the prostate. Because the grade may vary within the same tumor or between different tumors, different samples taken from your prostate may have different Gleason scores. Typically, the highest Gleason score will be the one used by your doctor for predicting your prognosis and deciding on treatment options.
Histopathologic And Tumor Biomarker Evaluation
One dedicated genitourinary pathologist undertook a systematic histopathologic review of all available H&E slides for each case, blinded to patient outcome, for the presence or absence of PNI, Gleason grade, pathologic tumor stage , high-grade prostatic intraepithelial neoplasia , acute and chronic inflammation, and patterns of atrophy . TURP specimens were also assessed for tumor volume . The presence or absence of PNI was assessed in each available tumor slide. PNI was defined as the presence of complete circumferential encirclement of nerve structures by malignant glands. Cases with noncircumferential PNI or a single focus of PNI among multiple tumor slides were deemed PNI-negative.
Tumor proliferation, apoptosis, and angiogenesis were also examined in a subset of the patients in the HPFS. Ki67 immunostaining was performed on tumor tissue microarrays using a polyclonal antibody , diluted 1:2,000 after citrate-based antigen retrieval, and scored by quantitative image analysis. A TUNEL assay on tissue microarrays was used to assess apoptosis. For a subset of patients , whole section specimens were analyzed for morphologic markers of tumor angiogenesis by staining for the CD34 marker and using image analysis as described previously .
Radiation Of Miapaca2 Cells Impairs Migration And Pni Through Compromised Cellular Viability
We evaluated if radiation may impair cancer cell migration and PNI through mechanisms other than cell death. All experiments with radiated cells were performed at least 24 hours after radiation to allow for sub-lethal damage repair. In colony formation assays, MiaPaCa2 plating efficiency for colony formation was 10%. Colony formation was susceptible to single-fraction radiation doses, showing diminishing surviving fractions up through 8 Gy in a logarithmic fashion.
In migration assays, single fraction radiation of MiaPaCa2 inhibited cancer cell migration towards GDNF and DRG in a dose-dependent fashion . However, these observed differences correlated directly with surviving cell number in parallel plate experiments , suggesting that the impairment in migration was simply the result of RT-induced compromised cellular viability, rather than an impairment of chemotaxis. The assay was then repeated with starting cell numbers adjusted to achieve equivalent cell viability at 24 hours for all the radiation doses , and differences in migration towards GDNF and DRG were eliminated.
Understanding Your Prostate Pathology Report
At least initially, the pathology report is one of the most important factors in the management of your prostate health, especially if you have been diagnosed with cancer. For example, it can provide valuable information about the location and extent of the cancer, thus helping your physician decide whether to recommend active surveillance, hormone treatment, radiation therapy, or surgery.
With that in mind, you might think that preparing and reading a pathology report would be straightforward but unfortunately the opposite is true. Pathology reports are not prepared uniformly . In fact, they can vary considerably even within a single institution. They may not be labeled thoroughly or contain enough specifics for you and your doctor to make a good treatment decision.
In this article you will learn what your pathology report should include and how to make sense of the information it contains. Other articles on this site explain when to about the pathology report and why it is sometimes necessary to have a repeat biopsy, as well as what questions to ask to obtain the information you need to decide which treatment is best for you.
Swedish Watchful Waiting Cohort
PNI was present in 43 of 615 prostate cancer cases in the Swedish cohort. Patients with tumors harboring PNI tended to be slightly older . PNI was strongly associated with high Gleason grade; two-thirds of tumors with PNI were Gleason grade 8 tumors compared to only 16% of tumors without PNI . PNI was also positively associated with tumor volume and presence of hgPIN, a precursor lesion of prostate cancer . There was no association between the presence of PNI and chronic inflammation or any of the atrophy lesions.
Radiation Of The Sciatic Nerve Alone Decreases Gdnf Production In Vivo
To assess whether radiation alters the production of GDNF from sciatic nerves following radiation exposure, sciatic nerve lysates were collected 3 weeks after a single dose of 0 or 8 Gy and GDNF Elisa performed. A mean GDNF concentration of 130 pg/ml from non-radiated sciatic nerves was reduced to 65 pg/ml after a single dose of 8 Gy .
Perineural Invasion On Prostate Biopsy: Does It Mean That I Have Advanced Prostate Cancer
The simple answer is NO, however it should change your treatment game plan.
A member of one of my support groups who has been doing active surveillance for about 5 years recently reported that their current biopsy indicated that they now have perineural invasion . They did not understand what was the significance of this finding and they wanted to know if they now had advanced prostate cancer.
In reality, PNI is found in almost 30% of positive biopsies.
However, before I discuss the significance of this finding it is important to understand what this means. When a pathologist finds that there is PNI they are saying that they have found prostate cancer cells surrounding or tracking along a nerve fiber within the prostate. This does not mean that the cancer has left the gland.
Not withstanding this the importance of this finding , it takes on a new light when you realize that nerves within the prostate travel outside of the gland through microscopic holes in the prostate capsule. The capsule is the outer covering of the prostate gland, which for some period of time can manage to contain cancer cells within the gland. In essence it is a barrier protecting the rest of your body from prostate cancer cells.
However, the nerves do pierce the capsule and can offer an easy exit point for cancer cells from the gland to the rest of your body.
Simply put, the presence of PNI doubles the chance of a man having T3 disease .
Stone NN, Stock RG, Parikh D, et al.J Urol. 1998;160:17221726.
