Intermittent And Harmonic Ultrasonography
The rationale for intermittent and harmonic ultrasonography is that conventional ultrasonography destroys the microbubbles of the contrast agents used in ultrasonographic imaging. Intermittent ultrasonography increases the enhancement provided by the contrast agents. In harmonic imaging, the reverberations produced by the contrast agent are visualized at a different frequency than the insonating frequency, which can provide a better image.
Transrectal Ultrasound Guided Biopsy: Overview And Coding
A transrectal ultrasound may also be called prostate sonogram or endorectal ultrasound. It is used to look at the prostate and tissues around it. An;ultrasound transducer sends sound waves through the wall of the rectum and into the prostate and surrounding tissue.
A transrectal ultrasound of the prostate gland is typically used to help diagnose symptoms such as: a nodule felt by a physician during a routine physical exam or prostate cancer screening exam. An elevated blood test result, difficulty urinating.
Prostate ultrasound and biopsy both evaluate the abnormal results of a digital rectal exam or an elevated prostate-specific antigen blood test. Prostate ultrasound involves a probe about the size of a finger that is inserted a short distance into the rectum.
A suspicious area to biopsy or may take samples from several places in prostate. Generally, 10 to 12 tissue samples are taken. The entire procedure usually takes about 10 minutes.
Transrectal ultrasonography is a way of creating an image of the prostate gland using sound waves. In conventional ultrasound procedures, a probe placed against the skin sends painless, ultra-high-frequency sound waves into the body.
Preparing For Your Trus Biopsy
You have the biopsy in the outpatient department.
Your nurse will ask you to sign a consent form once they have given you information about the procedure.
You can’t have a TRUS biopsy if you have a urine infection. Some hospitals might get you to do a test before you have the procedure. Or just check with you that there’s no pain when you wee.;
You take;antibiotics;to;stop infection developing after the biopsy. You have a dose of antibiotics before the biopsy, and then;for;a couple of days afterwards.
Don’t Miss: What Is A Prostate Vibrator
Scared Stiff Of Having A Prostate Biopsy
Although the DRE and PSA tests are useful, they are not enough to make a clear diagnosis of prostate cancer. When results are abnormal or questionable, the doctor may prescribe a transrectal ultrasound and a biopsy. These examinations usually provide enough information for a precise diagnosis.
Having to undergo prostate biopsies can be scary: fear of the intervention, the pain it can cause, the unknown … or knowing you have prostate cancer. But remember, if you have cancer, the sooner it is diagnosed, the greater your chances of a complete cure with treatment!
Why a biopsy
Abnormalities detected during a digital rectal exam and a high PSA level often lead to a prostate biopsy. This procedure consists of taking small tissue samples of your prostate in order for the pathologist to examine them under a microscope to determine if they are cancerous or not.
That prostate biopsies are indicated does not mean that you necessarily have prostate cancer. Indeed, the analysis of microscopic specimens makes it possible to differentiate a benign hypertrophy from a cancer of the prostate.
To this day, the actual diagnosis of prostate cancer can only be made with a prostate biopsy.
Medical History And Physical Exam
If your doctor suspects you might have prostate cancer, he or she will ask you about any symptoms you are having, such as any urinary or sexual problems, and how long you have had them. You might also be asked about possible risk factors, including your family history.
Your doctor will also examine you. This might include a digital rectal exam , during which the doctor inserts a gloved, lubricated finger into your rectum to feel for any bumps or hard areas on the prostate that might be cancer. If you do have cancer, the DRE can sometimes help tell if its only on one side of the prostate, if its on both sides, or if its likely to have spread beyond the prostate to nearby tissues. Your doctor may also examine other areas of your body.
After the exam, your doctor might then order some tests.
Also Check: Will Bacterial Prostatitis Go Away
Read Also: What Is The Va Disability Rating For Prostate Cancer
What Is A Prostate/rectal Ultrasound
A prostate or rectal ultrasound is an imaging test that uses sound waves tolook at your prostate or your rectum.
The healthcare provider uses a small probe called a transducer to make theimages of your prostate or rectum. The transducer is about the size of afinger. It is gently placed into your rectum, where it sends out soundwaves that bounce off your organs and other structures. The sound waves aretoo high-pitched for you to hear. The transducer then picks up the bouncedsound waves. These are made into pictures of your organs.
Your provider can add another device called a Doppler probe to thetransducer. This probe lets your provider hear the sound waves thetransducer sends out. He or she can hear how fast blood is flowing througha blood vessel and in which direction it is flowing. No sound or a faintsound may mean that you have a blockage in the flow.
How Should I Prepare
Wear comfortable, loose-fitting clothing. You may need to remove all clothing and jewelry in the area to be examined.
You may be asked to wear a gown during the procedure.
You may be instructed to avoid taking blood thinners, such as aspirin, for seven to 10 days prior to the procedure if a biopsy is planned. An enema may be taken two to four hours before the ultrasound to clean out the bowel.
Also Check: Can A Prostate Biopsy Cause Problems
What Is A Prostate Biopsy
There are two main types of prostate biopsies transrectal ultrasound guided biopsies and transperineal biopsies. As the former tends to be more common, well focus on this method.
biopsies use ultrasound guidance with a biopsy tool to snip core samples from the prostate gland. An ultrasound probe and biopsy tool are introduced into the rectum where a biopsy needle penetrates the rectal wall and enters the prostate. The procedure is repeated up to 12 times.
Transrectal prostate biopsies are outpatient or in-office procedures that require only numbing medicine. Passing a needle through the rectum and into the prostate places you at risk of infection. To minimize the risk of infection, urologists commonly prescribe antibiotics beforehand.;
Other complications from prostate biopsies include:
- Blood in urine, semen, and stool
- Pain
Is Bluelaser 3t Mpmri Right For You
Knowledge is power only if man knows what facts not to bother with. -R.S. Lynd
Our BlueLaser 3T mpMRI empowers our patients by providing accurate knowledge about whats going on in their bodies, both normal and disease. You should consider BlueLaser 3T mpMRI for the earliest possible detection if:
- You have an elevated or rising PSA
- You have an abnormal DRE
- You were treated for a prostate infection or inflammation but your PSA is still high
- You are on Active Surveillance
- You are in a high-risk category to develop prostate cancer
- You have not had a PSA test but you have unusual urinary symptoms
Read Also: What Are The Signs That Prostate Cancer Has Spread
You May Like: What Is Neoplasm Of Prostate
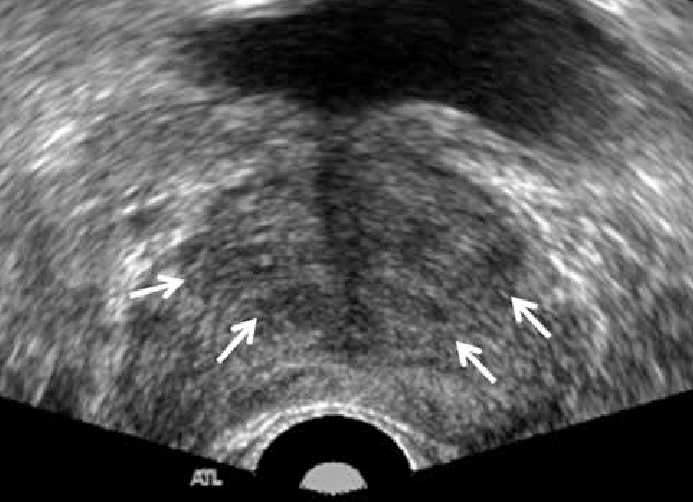
Biopsy Number And Technique
18G core biopsy needles are currently accepted as standard for the histological diagnosis of prostate cancer. The number of biopsies has increased since the original sextant biopsy developed by Hodge et al . 10 or 12 cores are now the standard in the UK and Europe, carried out in a systematic way according to number . The increasing number of biopsies reflects the isoechoic nature of the occult, small, multifocal cancers commonly encountered in modern practice. Thus, sampling is systematic and not random with the biopsies sampling the PZ, as this is the most likely site of cancer. However, there is still wide variation in the number of cores taken, direction of needle and area targeted. This is reflected in large variations in cancer detection between centres and also in the fact that increasing the number of cores will increase both cancer detection and complication rates . In the ProtecT study cancer detection rates varied from 23% to 53% across eight centres. It should also be noted that the current systematic biopsy protocols do not sample the inner gland because of its lower cancer rate and lower metastatic potential. Eichler et al analysed 87 studies and concluded that schemes of 12 cores that included posterior/laterally directed cores struck a balance between detection rate and adverse events.
Preparing For The Scan
You usually have this scan in the hospital x-ray department.
You need to make sure your bowel is empty when you go for your appointment. You might need to have an enema to empty your bowel. An enema is a liquid that you put into your back passage .
Or you might have a liquid medicine to swallow the day before. You need to stay close to a toilet for a few hours after taking the medicine.
Check your appointment letter to find out how to prepare for your scan.
Don’t Miss: What Happens After Prostate Surgery
How Is The Procedure Performed
In men, the prostate gland is located directly in front of the rectum, so the ultrasound exam is performed transrectally in order to position the imaging probe as close to the prostate gland as possible.
For a transrectal ultrasound, you will be asked to lie on your side with your knees bent. A disposable protective cover is placed over the transducer, it is lubricated, inserted through the anus and placed into the rectum.
The images are obtained from different angles to get the best view of the prostate gland.
If a suspicious lesion;is identified with ultrasound or with a rectal examination, an ultrasound-guided biopsy;can be performed. This procedure involves advancing a needle into the prostate gland while the radiologist;watches the needle placement with ultrasound. A small amount of tissue is taken for microscopic examination.
A prostate-specific antigen test, which measures the amount of PSA in the blood, may be administered to determine if a patient is at high risk for cancer. In this case, a biopsy is performed and an ultrasound probe is used to guide the biopsy to specific regions of the prostate gland.
When the exam is complete, you may be asked to dress and wait while the ultrasound images are reviewed.
This ultrasound examination is usually completed in less than 20 minutes.
What Does The Equipment Look Like
Ultrasound scanners consist of a computer console, video display screen and an attached transducer. The transducer is a small hand-held device that resembles a microphone. Some exams may use different transducers during a single exam. The transducer sends out inaudible, high-frequency sound waves into the body and then listens for the returning echoes. The principles are similar to sonar used by boats and submarines.
The technologist applies a small amount of gel to the area under examination and places the transducer there. The gel allows sound waves to travel back and forth between the transducer and the area under examination. The ultrasound image is immediately visible on a video display screen that looks like a computer monitor. The computer creates the image based on the loudness , pitch and time it takes for the ultrasound signal to return to the transducer. It also takes into account what type of body structure and/or tissue the sound is traveling through.
For ultrasound procedures such as transrectal exams that require insertion of an imaging probe, also called a transducer, the device is covered and lubricated with a gel.
Read Also: Can An Mri Detect Prostate Cancer
What Happens After A Prostate Ultrasound
Once the test is done, you can take off the gown and put your clothes back on. Your rectum may feel tender for a few days, but you wont need to follow any specific aftercare instructions. Your doctor may prescribe an antibiotic to prevent infection.
In some cases, your doctor or technician may ask you to wait in the facility until your results are available. Youll usually need to wait a few days for a radiologist to look at the images and diagnose any conditions, however. Depending on where the test was done, you may wait up to two weeks for results.
Your doctor will schedule a follow-up appointment to discuss your test results. If you have any abnormalities or conditions that are visible on the images, your doctor will point out these areas. Excess tissue, prostate enlargement, or cancerous tumors will appear on the ultrasound images as bright white areas that represent the dense tissue.
Uses Of Transrectal Ultrasound
Since ultrasound scan are used to produce real-time images of the internal organs/structure, Transrectal ultrasound can be used to diagnose a variety of condition and can be used to check for;
It can also serve as a guide to procedures such as needle biopsy a situation in which needles are used to extract a sample of the cell from an organ for a Laboratory test.
Also Check: How To Prevent Prostate Cancer Naturally
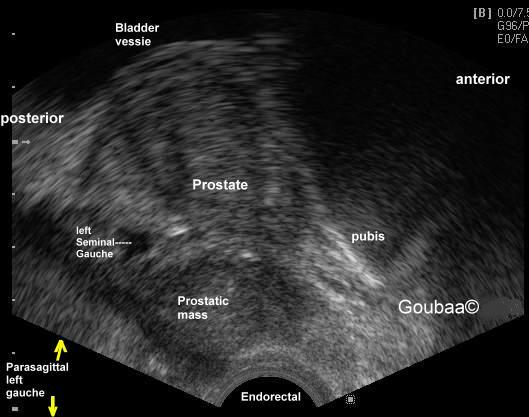
Transrectal Ultrasound Guided Prostate Biopsy
A transrectal ultrasound creates an image of organs in the patients pelvis. It is typically used to evaluate the prostate gland in men with elevated prostate specific antigen , or as further exploration when the Urologist detects prostatic nodules by digital rectal exam. The ultrasound images may reveal prostate cancer, benign enlarged prostate or prostatitis. Ultrasound can also help guide a biopsy of the prostate.
A transrectal ultrasound is typically performed in an outpatient setting. The Urologist will collect between six to twelve tissue samples with a small needle. While patients often report physical discomfort , the procedure usually only lasts about a half hour.
Following the procedure, complications include blood in the urine for several days, some bleeding in the stool for a few days, and blood in the ejaculate for a few weeks.
What Happens After The Procedure
The doctor will send the biopsy to a lab for analysis. Theyâll discuss the results with you when theyâre ready, which is usually within a week. Meanwhile:
- You can go back to your normal meals and activities.
- Do NOT take aspirin, products with aspirin, anti-inflammatory drugs such as Advil, Motrin, or Naprosyn, or indomethacin for at least 3 days after the procedure.
- Drink six to eight glasses of water every day for 3 days after the test to help flush your urinary system.
- You may notice a small amount of blood in your urine, semen, or stool up to 7 days afterward. This is normal.
- If your rear end is sore, soak in a warm bath for 20 minutes.
- Take your antibiotics until all the pills are gone. If you miss a dose, take it when you remember and then go back to your regular schedule.
Also Check: What Happens To The Prostate Later In Life
What You May Experience During And After A Transrectal Ultrasound
During a Transrectal ultrasound, you may experience minimal discomfort as the transducer is inserted into your anus or if biopsy is performed you may also experience discomfort when the needle is being inserted into the prostate gland.
Any pain or discomfort during this exam is usually temporary. After the Transrectal ultrasound, you will be asked to dress and sit for a while as the result is being reviewed.
You may be given the results or asked to return to the hospital in a few days and should be able to resume normal activities after an ultrasound scan but if pains persists after the scan then do not hesitate to call your doctor.
What Is A Transrectal Ultrasound For
A TRUS may help doctors not only make a diagnosis, but identify the exact location and size of a tumor as well.
A TRUS may be useful:
- If your PSA blood test results are abnormal, or your doctor feels an abnormal area during a digital rectal exam.
- If your doctor needs to perform a biopsy. A TRUS may help pinpoint where a tissue sample should be taken from, to give your doctor the best diagnostic results possible.
- To help your doctor determine the size of your prostate gland, especially if its naturally large.
- To help your doctor determine whether cancer has spread to any lymph nodes or other tissues.
- To help your doctor better navigate during certain prostate cancer treatments. A TRUS may help guide procedures such as a brachytherapy; or cryotherapy, which freezes prostate cancer cells.
You May Like: What Is Perineural Invasion In Prostate Cancer
Use Of Mri For Surveillance Of Prostate Cancer
The concept of observation as a therapeutic option for men with clinically localized prostate cancer has been well established and is associated with excellent long-term progression-free survival in men with favorable malignancy on prostate biopsy. Chodak et al. demonstrated in a large multi-institutional pooled analysis of 828 men that conservative therapy, also known as watchful waiting, resulted in disease-specific survival of 87% at 10 years for men with either grade 1 or grade 2 cancer. The finding that the metastasis-free survival for men with Grade 2 adenocarcinoma was only 58% at 10 years suggested that there was a role for a more active monitoring strategy in some men.125 More contemporary trials, including PIVOT and Protec T, support surveillance rather immediate treatment in contemporary patients, most likely to get diagnosed with serum PSA where the risk of overdiagnosis has been established.126,127
Despite this conclusion, significant opportunities exist for further refinement of active surveillance protocols to better risk-stratify men at initial entry into these protocols and to better target the regions of the prostate that could harbor a malignancy that would require a delayed therapeutic intervention. The combination of advanced imaging with MRI, altered biopsy approaches, , and the use of molecular markers appear to improve the outcomes of active surveillance.
Key Point
