Metastases: Whether The Cancer Has Spread
The spread of cancer is measured in two ways: by lymph node involvement, and by its appearance in other organs or parts of the body, or metastasis.
Lymph node staging, or N-staging, determines whether the cancer is present in nearby lymph nodes. Lymph nodes are tiny organs that are part of the immune system.NX: The regional lymph nodes cannot be evaluated.N0: The cancer has not spread to lymph nodes in the immediate area.N1: The cancer has spread to lymph nodes in the pelvic region.
The M in the TNM system indicates whether the prostate cancer has spread to other parts of the body, such as the lungs or the bones. This is called distant metastasis.
MX: Metastasis cannot be evaluated.M0: The cancer has not metastasized beyond the immediate prostate region.M1: The cancer has metastasized deeper into the body.
- M1a: The cancer has spread to lymph nodes away from the groin area.
- M1b: The cancer has spread to the bones.
- M1c: The cancer has spread to another part of the body, with or without spread to the bones.
The combination of your full staging results, including your grade and your T, N, and M stages, paints a more complete picture of how the cancer is progressing. This enables your doctors to determine which treatments have the best chance or controlling or eradicating your cancer.
Ct Scanning Mri And Bone Scanning
Men with PSA levels above 10 ng/mL, high-grade histology , or physical findings that suggest stage T3 disease should probably undergo a staging computed tomography scan and bone scan. CT scanning is the one modality with evidence-based guidelines. The CT scan can be used to evaluate extension into the bladder and lymph nodes to help stage the patient’s cancer or to consider lymph node sampling prior to treatment.
According to the National Comprehensive Cancer Network , technetium-99m-methyl diphosphonate bone scan is indicated in the initial evaluation of patients at high risk for skeletal metastases, as indicated by any of the following :
- T1 disease, PSA 20
- Symptoms suggestive of osseous metastasis
The NCCN recommends pelvic CT or magnetic resonance imaging in patients with any of the following:
- T1-T2 disease and nomogram-indicated probability of lymph node involvement > 10%
Conventional endorectal MRI is helpful for localizing cancer within the prostate and seminal vesicles and for local staging. Dynamic, contrast-enhanced MRI and MR spectroscopic imaging are complementary in local staging, but their use is currently limited to a research setting.
- Detection of large and poorly differentiated tumors
- T staging: Detection of extracapsular extension, with high negative predictive values in low-risk men
- N staging: MpMRI is equivalent to CT scan
- M staging: MpMRI outperforms bone scan and targeted x-rays for M staging, with 98-100% sensitivity and specificity
Can The Gleason Score On My Biopsy Really Tell What The Cancer Grade Is In The Entire Prostate
Because prostate biopsies are tissue samples from different areas of the prostate, the Gleason score on biopsy usually reflects your cancers true grade. However, in about 1 out of 5 cases the biopsy grade is lower than the true grade because the biopsy misses a higher grade area of the cancer. It can work the other way, too, with the true grade of the tumor being lower than what is seen on the biopsy.
Recommended Reading: How Big Can A Prostate Get
Stage 1 Prostate Cancer Treatment
Where stage 1 prostate cancer patients are of an advanced age, a watch and wait approach* is usually chosen over conventional medical treatment. This is because tumors can be slow growing at this early first stage and the survival rate is very high. For example, a person over 80 years old who is diagnosed with stage 1 prostate cancer could be more likely to die from other causes. Treatment could mean the benefits are outweighed by negative side effects. *also referred to as watchful waiting
However, in cases where a younger person has been diagnosed with first stage prostate cancer, there may be more immediacy in treating the disease rather than monitoring it. A younger person will have more years ahead of them in which the cancer can develop, and they may also make a better recovery following medical treatment.
When treatment is given, the treatment options are similar to those for stage 2 prostate cancer. The prostate gland may be removed through a procedure known as a radical prostatectomy. Radiation therapy and hormonal therapy may also be administered to shrink any tumors.
You May Like: How Do Prostate Cancer Patients Die
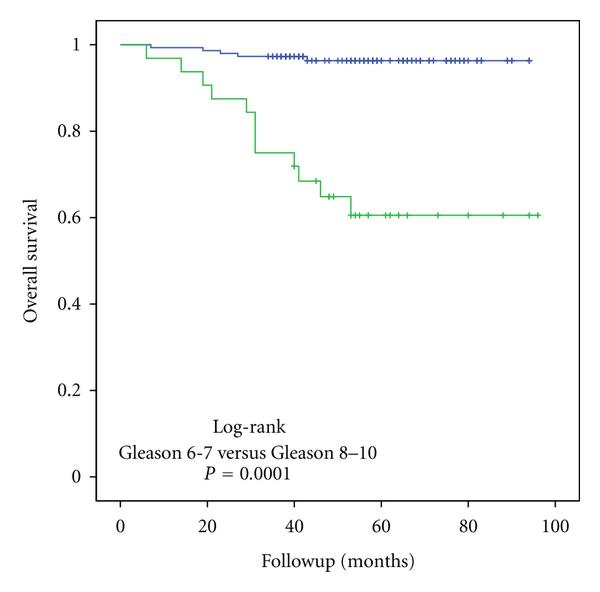
Prognostic Nomogram For Os
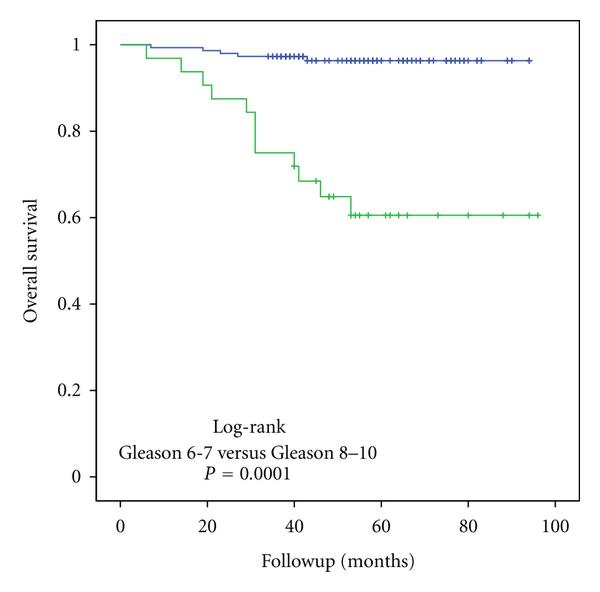
To establish a prognostic nomogram in predicting OS for prostate cancer patients with Gleason score 7, the study population were randomly divided into the training group and testing group in a 7:3 ratio. The nomogram integrating all the significant independent factors for OS based on the training cohort is shown in Figure 6A. The C-index for nomogram of OS prediction was 0.785 , and 0.788 in the training and validation cohort, respectively. The calibration plots indicated an optimal agreement between the actual observation and nomogram prediction for OS probability at 5 and 10 year in the training cohort and testing cohort .
Figure 6. Nomogram for OS of Gleason score 7 prostate cancer Nomogram for CSS of Gleason score 7 prostate cancer.
Don’t Miss: Hormone Therapy With Radiation For Prostate Cancer
What Does It Mean If My Biopsy Mentions That There Is Perineural Invasion
Perineural invasion means that cancer cells were seen surrounding or tracking along a nerve fiber within the prostate. When this is found on a biopsy, it means that there is a higher chance that the cancer has spread outside the prostate. Still, perineural invasion doesnt mean that the cancer has spread, and other factors, such as the Gleason score and amount of cancer in the cores, are more important. In some cases, finding perineural invasion may affect treatment, so if your report mentions perineural invasion, you should discuss it with your doctor.
Understanding Prostate Cancers Progression
To determine the appropriate treatment, doctors need to know how far the cancer has progressed, or its stage. A pathologist, the doctor trained in analyzing cells taken during a prostate biopsy, will provide two starting pointsthe cancers grade and Gleason score.
- Cancer grade: When the pathologist looks at prostate cancer cells, the most common type of cells will get a grade of 3 to 5. The area of cancer cells in the prostate will also be graded. The higher the grade, the more abnormal the cells.
- Gleason score: The two grades will be added together to get a Gleason score. This score tells doctors how likely the cancer is to grow and spread.
After a biopsy confirms prostate cancer, the patient may undergo additional tests to see whether it has spread through the blood or lymph nodes to other parts of the body. These tests are usually imaging studies and may include a bone scan, positron emission tomography scan or computed tomography scan.
Prostate cancer treatment: The care you need is one call away
Your multidisciplinary team will work with you to develop a personalized plan to treat your prostate cancer in a way that fits your individual needs and goals.
Recommended Reading: Can Zytiga Cure Prostate Cancer
Staging Of Prostate Cancer
Doctors will use the results of your prostate examination, biopsy and scans to identify the stage of your prostate cancer .
The stage of the cancer will determine which types of treatments will be necessary.
If prostate cancer is diagnosed at an early stage, the chances of survival are generally good.
Read Also: Best Treatment For Gleason 7 Prostate Cancer
Risk Of Progression Of Prostate Cancer
Prostate cancer can also be classified based on the risk of recurrence . For this assessment, that can impact your choice of therapeutic approach, we take into account your clinical stage, PSA level, and Gleason score.
Low risk
Your cancer may be at low risk of spreading if:
- Your PSA level is less than 10 ng/mL
- You Gleason score is 6 or less
- Your cancer is stage T1 or T2a
Medium risk
Your cancer may be at medium risk of spreading if:
- Your PSA level is between 10 and 20 ng/mL
- Your Gleason score is 7
- Your cancer is stage T2b
High risk
Your cancer may be at high risk of spreading if:
- Your PSA level is higher than 20 ng/mL
- Your Gleason score is 8, 9 or 10
- Your cancer is stage T2c, T3 or T4
Don’t Miss: How Does An Enlarged Prostate Affect Urination
Survivability For Prostate Cancer According To Stage
Relative survival looks at a persons chances of surviving after diagnosis compared to a healthy person from the general population who shares similar characteristics, such as age, sex, and race.
For prostate cancer, relative survival depends on the stage of the disease . It is important to note that this prognostic grouping, also established by the UICC, is more accurate than stage grouping in assessing a survival prognostic.
Read Also: Is Frequent Urination A Sign Of Prostate Cancer
What Is Prostate Cancer
Prostate cancer develops in the prostatea small gland that makes seminal fluid. It is one of the most common types of cancer in men. Prostate cancer usually grows over time and, in the beginning, usually stays within the prostate gland, where it may not cause serious harm. While some types of prostate cancer grow slowly and may need minimal or no treatment, other types are aggressive and can spread quickly.
Prostate cancer that is caught early has a better chance of successful treatment.
Read Also: What Medication Is Used To Treat Enlarged Prostate
Prostate Health Index Testing
The Prostate Health Index test is a diagnostic blood test that combines free and total PSA and the pro-PSA isoform . The PHI test is intended to reduce the number of unnecessary prostate biopsies in PSA-tested men. In prospective multicenter studies, the PHI test has outperformed free and total PSA for detection of prostate cancer and has improved prediction of clinically significant prostate cancer in men with a PSA of 2 or 4 ng/mL to 10 ng/mL.
Assessment Of Unusual Epe Cases
We encountered several unusual cases where it was not possible to clearly measure the length extending beyond the prostate proper. One case showed that the tumor appeared to extend to the periprostatic soft tissue beyond the prostate proper. However, thick-walled vasculature was in the vicinity of the extending tumor and did not involve the fat pads. In this case, the tumor appeared to extend beyond the prostate capsule but did not invade into any fat pad. Therefore, it was classified as pT2 .
Figure 4
An example of a pT2 case. The tumor showed definite protrusion beyond the prostate proper at the level of thick vasculature. However, fat pads were not apparently involved. In this case, we suggest a T2 classification. Although such cases are often encountered, they should not be dealt with as T3 cases. The presence of tumor cells in anterior muscle bundles without neurovascular bundles causes controversy in the evaluation of EPE. Most accepted guidelines define EPEs as extending beyond the contour of the proper tissue. EPE showed extensively broad-based sessile extensions of tumor beyond the capsule and fat pad.
You May Like: When Do Men Start Getting Prostate Exams
Where Can I Get Support
Being diagnosed with any kind of prostate cancer can be frightening and overwhelming. No matter what youre feeling or thinking, there is support available if you want it. You can speak to our Specialist Nurses, in confidence or chat with them online. Our Dealing with prostate cancer page looks at things you can do to help yourself and people who can help.
Visit our wellbeing hub for information to help support you in looking after your emotional, mental, and physical wellbeing. If you are close to someone with prostate cancer, find out more about how you can support someone with prostate cancer and where to get more information.
What Does It Mean If In Addition To Cancer My Biopsy Report Also Mentions Acute Inflammation Or Chronic Inflammation
Inflammation of the prostate is called prostatitis. Most cases of prostatitis reported on biopsy are not caused by infection and do not need to be treated. In some cases, inflammation may increase your PSA level, but it is not linked to prostate cancer. The finding of prostatitis on a biopsy of someone with prostate cancer does not affect their prognosis or the way the cancer is treated.
Also Check: Prostate Cancer Lung Metastasis Treatment
Characteristics Of Prostate Cancer
Ninety-five percent of prostate cancers are adenocarcinomas. In approximately 4% of men with prostate cancer, the neoplasm has transitional cell morphology and is thought to arise from the urothelial lining of the prostatic urethra.
In rare cases, the tumor has a neuroendocrine morphology in such instances the neoplasm is believed to have arisen from the neuroendocrine stem cells that are normally present in the prostate or from aberrant differentiation programs during cell transformation.
Seventy percent of prostate cancers arise in the peripheral zone, 15-20% arise in the central zone, and 10-15% arise in the transition zone.
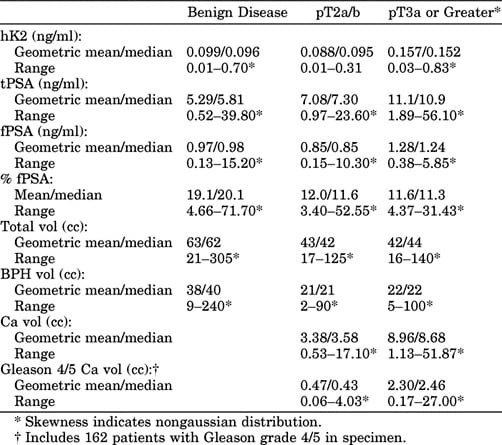
Percentage Of Free Psa
The measurement of bound and free PSA can help to differentiate mildly elevated PSA levels caused by cancer from elevated levels resulting from benign prostatic hyperplasia. The lower the ratio of free-to-total PSA, the higher the likelihood of cancer. For example, among men with greater than 25% free PSA, only 8% are found to have cancer at prostate biopsy.
In contrast, more than half of men with less than 10% free PSA are found to have cancer at biopsy. While cutoffs may be used, the percentage of free PSA is usually employed as an additional factor in making an informed recommendation for or against biopsy. Generally, these percentages are useful in patients who have a PSA level in the range of 4-10 ng/mL.
This information is most useful in men with very large glands or in whom 1 biopsy result has already been negative. In healthy men with a PSA level of 4-10 ng/mL, many recommend biopsy without the additional free-PSA test or consider a trial of antibiotic therapy for 4-6 weeks before repeating the PSA test.
You May Like: How Do They Biopsy A Prostate
Risk Factors For Prostate Cancer
Factors that can increase your risk of prostate cancer include the following.
- Older age: Your risk of prostate cancer increases as you age.
- Race: Black men have a greater risk of prostate cancer than do men of other races. In black men, prostate cancer is also more likely to be aggressive or advanced. It’s not clear why this is.
- Family history of prostate or breast cancer: If men in your family have had prostate cancer, your risk may be increased. Also, if you have a family history of genes that increase the risk of breast cancer or a very strong family history of breast cancer, your risk of prostate cancer may be higher.
- Obesity: Obese men diagnosed with prostate cancer may be more likely to have advanced disease that’s more difficult to treat.
Understanding Your Pathology Report: Prostate Cancer
When your prostate was biopsied, the samples taken were studied under the microscope by a specialized doctor with many years of training called a pathologist. The pathologist sends your doctor a report that gives a diagnosis for each sample taken. Information in this report will be used to help manage your care. The questions and answers that follow are meant to help you understand medical language you might find in the pathology report from your prostate biopsy.
Read Also: How Do Men Get Prostate Cancer
Risk Groups For Prostate Cancer
Prostate cancer is divided into risk groups.
Before planning your treatment, your cancer doctor will look closely at your risk group. This helps you and your doctors to decide on the best treatment for you. The treatment options for each risk group can be different.
Prostate cancer was previously grouped into low, intermediate or high risk groups. Doctors now use a more detailed system to work out your risk group. This is called the Cambridge Prognostic Group . It divides prostate cancer risk into 5 different groups. Your doctor may still describe your risk as low, moderate or high.
To work out your CPG risk group, your doctors look at:
- the stage of the cancer
- your Gleason score.
Tnm Staging For Prostate Cancer
The TNM system is a way of staging prostate cancer. It stands for Tumour, Node, Metastasis. Staging means describing the size of the cancer and how far it has grown.
Doctors in the UK now use a tool called the Cambridge Prognostic Group to divide prostate cancer into 5 groups. The CPG uses information about:
- the T stage from the TNM staging
- Grade Groups or Gleason score
- Prostate specific antigen level
You May Like: How To Reduce Your Chances Of Getting Prostate Cancer
Prostate Grading Group And Gleason Pattern In Epe
All 1,903 RP cases were assigned to five subgroups according to PGG classification: 357 cases of PGG 1, 670 cases of PGG 2, 313 cases of PGG 3, 224 cases of PGG 4 and 339 cases of PGG 5. When focusing on 501 pT3 cases, these cases were assigned to each group as follows: eight cases of PGG 1, 126 cases of PGG 2, 81 cases of PGG 3, 71 cases of PGG 4 and 179 cases of PGG 5.
In the majority of cases, GP in the areas of EPE paralleled that of the dominant tumor nodule, usually GP 4 and 5 . However, in a few cases of PGG 2 and 3, GP 3 tumor was identified in the area of EPE, whether alone or more commonly mixed with GP 4 . Seminal vesicle invasion was not found in PGG 1 and was observed in six cases of PGG 2 and eight cases of PGG 3.
Figure 1
Gleason grade and extraprostatic extension . Gleason patterns in the areas of EPE paralleled the dominant tumor pattern, usually Gleason patterns 4 and 5. A few cancer cells scattered around the nerve outside of the capsule were often encountered and can indicate Gleason pattern 5. In a few cases of PGG2 and 3, EPEs were scored as Gleason Grade 3, whether alone or more commonly mixed with Grade 4.
