Understanding Your Pathology Report: Prostatic Intraepithelial Neoplasia And Intraductal Carcinoma
When your prostate was biopsied, the samples taken were studied under the microscope by a specialized doctor with many years of training called a pathologist. The pathologist sends your doctor a report that gives a diagnosis for each sample taken. Information in this report will be used to help manage your care. The questions and answers that follow are meant to help you understand medical language you might find in the pathology report from your prostate biopsy.
Invasive Cribriform Acinar Adenocarcinoma Of Prostate
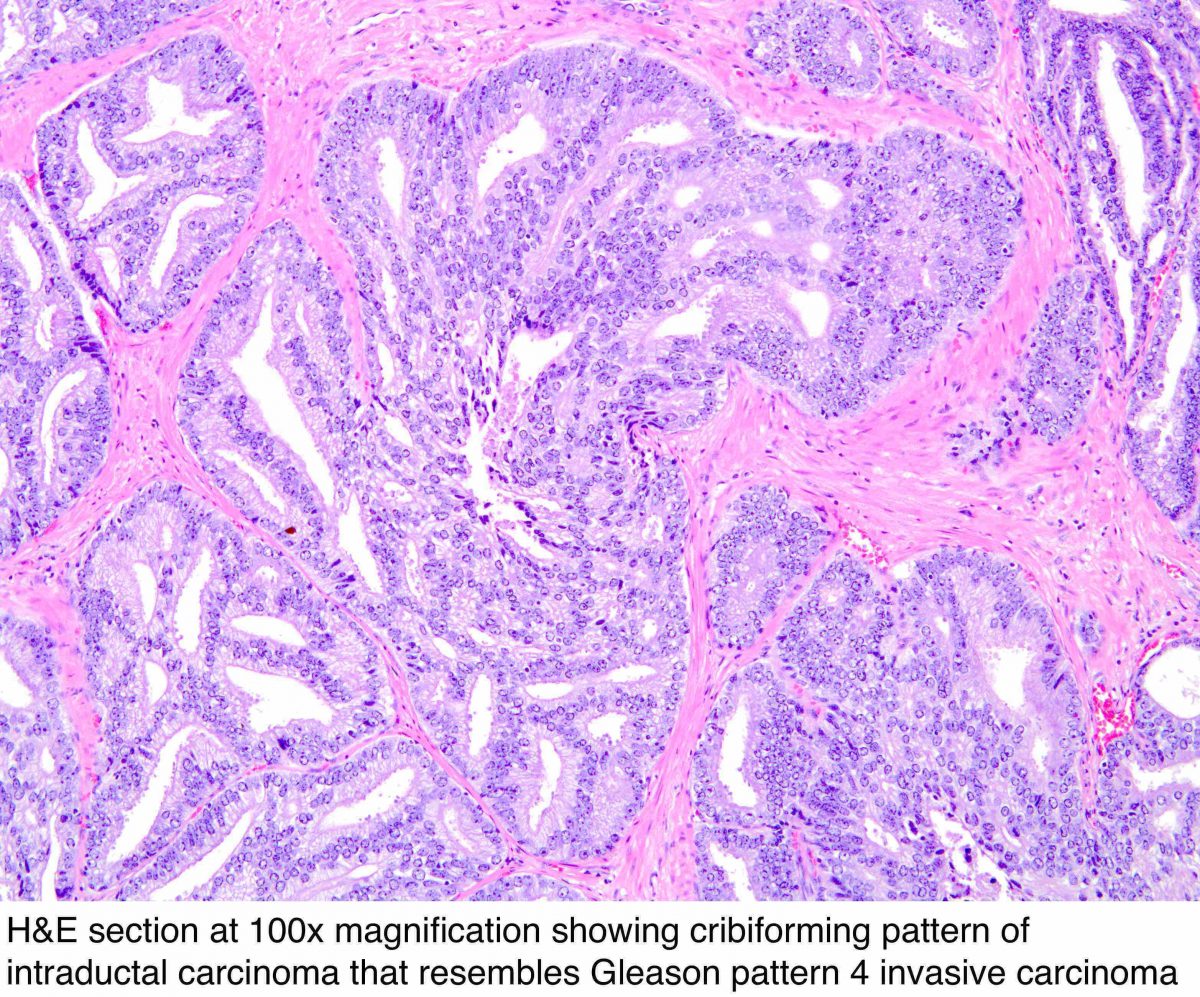
Infiltrating cribriform acinar adenocarcinoma closely mimics cribriform IDC-P. Invasive cribriform cancer, unlike IDC-P, lacks a basal cell lining. In some cases, the contour and branching pattern of normal duct architecture distinguishes IDC-P from infiltrating cribriform acinar adenocarcinoma. The distinction between invasive, high-grade PCa and IDC-P, however, is not critical because IDC-P is usually associated with a high-grade and high-volume PCa. Most cases of IDC-P would be diagnosed as cribriform acinar adenocarcinoma if immunohistochemistry for basal cells is performed.
What Will Happen After My Treatment
You will have regular check-ups during and after your treatment to check how well it is working. You may hear them called follow-up appointments. Youll have regular PSA blood tests ask the people treating you how often youll have these. If your PSA level goes down this usually suggests your treatment is working.
Tell your doctor or nurse about any side effects youre getting. There are usually ways to manage side effects.
Make sure you have the details of someone to contact if you have any questions or concerns between check-ups. This might be your specialist nurse or key worker. You can also speak to our Specialist Nurses.
Read more about follow-up after prostate cancer treatments.
Also Check: What Is Residual Prostate Cancer
Synchronous Male Breast And Prostate Cancer
It is most likely that our patient developed cancer in the prostate before the breast, given the advanced stage of prostate cancer as opposed to the early in situ stage of breast tumour at presentation. As we alluded to earlier, having prostate cancer per se does not increase the chance of developing breast cancer . As our patient denies other known risk factors for developing breast cancer, the only factor that was not investigated in him was genetic abnormalities connecting between the two primaries.
It is unlikely that a germline mutation would manifest itself at an age as late as 72 years old, especially in someone with no family history of malignancies. Interestingly, up to 90% of metastatic prostate cancer patients harbour abnormal genes, either somatic or germline . Even though DNA damage repair genes, including the BRCA gene, represent a quarter of abnormal genes in prostate cancer patients, the more common genetic abnormalities detected in them are in the AR, TP53, and RB1 genes. Furthermore, of the DDR genes, while BRCA2 mutation represents the most frequent event , other abnormal DDR genes have also been detected in metastatic prostate cancer patients, albeit at much lower frequencies, such as the ATM, MSH2, BRCA1, FANCA, MLH1, CHEK, and PTEN genes . These other genes, such as p53, CHEK, and PTEN, also increase the risk for breast cancer .
The Initial Causes Carcinoma In Situ Of Prostate
One of the first symptoms of prostate issues is pain or tenderness in the groin or lower back. This can be the result of a noncancerous condition called enlarged prostatic tissue, or it could be an infection of the bladder. In either case, its important to see a doctor as soon as possible. If youre suffering from prostate pain, you may want to consider reducing your caffeine intake.
Another symptom of a potentially enlarged prostate is difficulty starting a stream of urine, leaking, or dribbling. These symptoms are not serious, but theyre still alarming. Most men put up with an enlarged prostate for years before seeking medical attention, but they typically seek treatment as soon as they notice symptoms. Even if you dont have symptoms, its worth getting checked to determine if you have any prostate issues.
If you experience nightly bathroom runs, you may be experiencing an enlarged prostate. You may be having difficulty starting a stream of urine, or you may even be dribbling or leaking during the day. These problems arent life-threatening, but can become a nuisance. You should not ignore these signs and seek treatment as soon as you notice them. If you feel any of these symptoms, you should consult a doctor.
Read Also: Can You Have Sex Without A Prostate
Management Of Papillary Dcis In Men
DCIS has been reported to represent only between 9 and 11% of all male breast cancer as male breast cancers are more commonly invasive in nature . Because of the rarity of male breast DCIS, its management is mostly extrapolated from that of the management of the female counterpart, with some notable differences in the surgical options as well as endocrine treatment, which will be discussed below.
Papillary DCIS is the least common subtype of female breast DCIS, but it is the most common form of DCIS in male breast cancer . Nevertheless, as with other types of DCIS, untreated papillary DCIS has an increased risk of developing into invasive breast cancer. Therefore, surgical removal of the mass is the mainstay of treatment. For this, we feel that simple mastectomy without axillary surgery was justified as the best approach for our patient.
While the no axillary surgery approach in our patient concurs with accepted international guidelines on the management of breast DCIS, such as those from the National Cancer Care Network and ASCO, due to the low rate of axillary metastases associated with DCIS, perhaps we should have considered sentinel lymph node biopsy in the same setting as mastectomy as there is a small possibility that an element of tumour invasiveness may be missed during biopsy. We were fortunate that the final mastectomy specimen of our patient did not reveal an invasive component.
What Are The Symptoms Of Prostate Cancer
Prostate cancer doesn’t always cause symptoms, especially at first. If it does cause symptoms, they may include:
- Problems urinating , such as:
- A urine stream that’s weak, hard to start, or starts and stops
- Suddenly needing to urinate right away
- Urinating often, especially at night
- Pain or burning when urinating
- Blood in your urine or semen
But many of these symptoms may be from other common prostate problems that aren’t cancer, such as an enlarged prostate.
You should discuss your prostate health with your health care provider if you:
- Have symptoms that could be prostate cancer
- Have a high risk for developing prostate cancer
- Had a screening test that suggests you could have prostate cancer
Recommended Reading: What Is Prostate Cancer Staging
Histologic Features And Diagnosis Of Idc
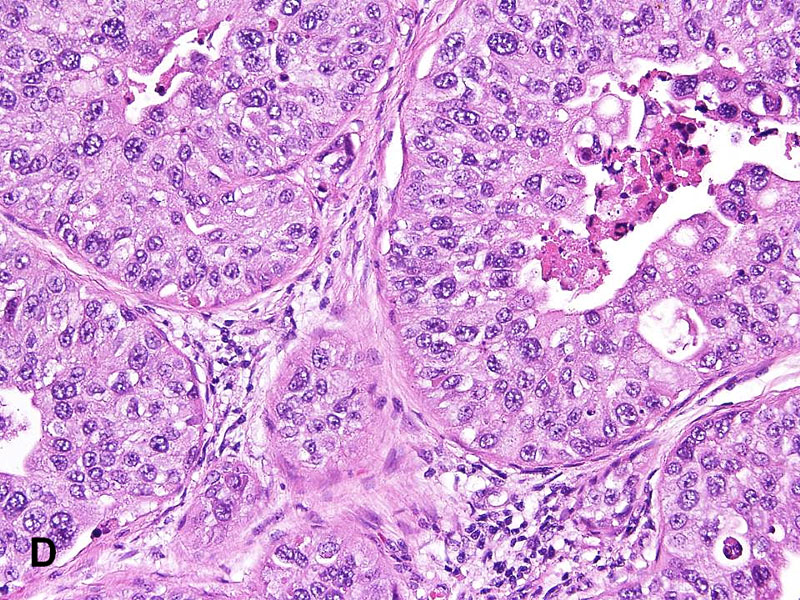
The hallmark of IDC-P is the expansile proliferation of PCa cells within the native prostatic glands with an at least partially preserved basal cell layer . McNeal and Yemoto first defined IDC-P as the complete spanning of the ductal or acinar lumen by several trabeculae of malignant epithelial cells, with foci of trabecular fusion, in radical prostatectomy specimens. More-proliferative, denser lesions with cribriform or solid architecture were also included in their definition. Later studies refined the histologic features of IDC-P .,, Classic examples of IDC-P usually comprise many glands, often greater than 6 per radical prostatectomy specimen, and the glands are larger than normal peripheral zone glands,, with irregular and branching contours .,, The neoplastic cells in IDC-P grow in several architectural patterns, including trabecular, loose cribriform , dense cribriform , and solid , which represent progressive dedifferentiation, with a reciprocal increase in proliferation and correlated with cancer stage, grade, and clinical course. Neoplastic cells in classic IDC-P are pleomorphic, some 6 times larger than adjacent nonneoplastic nuclei . Two cell populations may be seen, usually in the dense cribriform and solid IDC-P, in which a central population of cells has small and uniform nuclei, and the peripheral population cells have pleomorphic nuclei . Comedonecrosis is diagnostic of IDC-P but is only present in a subset of cases .
Figure 1.
What Causes Prostate Cancer
Researchers don’t know for sure what causes prostate cancer. They do know that it happens when there are changes in the genetic material .
Sometimes these genetic changes are inherited, meaning that you are born with them. There are also certain genetic changes that happen during your lifetime that can raise your risk of prostate cancer. But often the exact cause of these genetic changes is unknown.
Don’t Miss: Can A Prostate Infection Be Cured
What Does It Mean If My Biopsy Report Also Mentions Atrophy Adenosis Or Atypical Adenomatous Hyperplasia
All of these are terms for things the pathologist might see under the microscope that are benign , but sometimes can look like cancer under the microscope.
Atrophy is a term used to describe a shrinkage of prostate tissue . When it affects the entire prostate gland it is called diffuse atrophy. This is most often caused by hormones or radiation therapy to the prostate. When atrophy only affects certain areas of the prostate, it is called focal atrophy. Focal atrophy can sometimes look like prostate cancer under the microscope.
Atypical adenomatous hyperplasia is another benign condition that can sometimes be seen on a prostate biopsy.
What Does It Mean If My Biopsy Report Mentions The Word Core
The most common type of prostate biopsy is a core needle biopsy. For this procedure, the doctor inserts a thin, hollow needle into the prostate gland. When the needle is pulled out it removes a small cylinder of prostate tissue called a core. This is often repeated several times to sample different areas of the prostate.
Your pathology report will list each core separately by a number assigned to it by the pathologist, with each core having its own diagnosis. If cancer or some other problem is found, it is often not in every core, so you need to look at the diagnoses for all of the cores to know what is going on with you.
Read Also: How Likely Is It For Prostate Cancer To Spread
Information For Medical Professionals
Code Edits
The Medicare Code Editor detects and reports errors in the coding of claims data. The following ICD-9 Code Edits are applicable to this code:
Index to Diseases and Injuries
References found for the code 233.4 in the Index of Diseases and Injuries:
- Dysplasia SEE ALSO
- intraepithelial neoplasia III PIN III 233.4
- prostate gland 185 198.82 233.4 222.2 236.5 239.5
- utricle 189.3 198.1 233.9 223.81 236.99 239.5
- PIN III prostatic intraepithelial neoplasia III 233.4
What Is Carcinoma Of The Prostate
Carcinoma of the prostate is a type of prostate cancer that occurs when normal prostate cells begin to grow uncontrollably.
Carcinomas begin in the epithelial tissuethe thin tissue, like skin, that covers the linings of internal organs. Other cancers typically form in the bodys connective or supportive tissues , blood-forming tissue like bone marrow , or within the immune system .
Carcinomas are the most common type of cancer and they can be broken down into multiple subgroups: squamous cell carcinoma, adenocarcinoma, transitional cell carcinoma, and basal cell carcinoma.
How commonare carcinomas of the prostate?
The most common carcinoma of the prostate is an adenocarcinoma they make up about 95% of all prostate carcinomas. Adenocarcinomas are a type of cancer that are produced by glandular cells, such as those of the prostate gland. They are most commonly found in men over the age of 70.
Othercarcinomas of the prostate are less common and only make up about 5% of totalprostate carcinomas. Transitional cell carcinomas form in the cells that coverthe urethra. This cancer typically begins in the bladder and then spreads tothe prostate. Some carcinomas, like squamous cell or small cell carcinomas, arerare, malignant tumors of the prostate. In contrast to most prostate cancersthat are slow growing, and these types of carcinomas are usually aggressive.
Read Also: When To Get Prostate Test
Clinical Significance Of Idc
Studies have established that IDC-P represents an aggressive form of PCa and is an adverse pathologic parameter in both radical prostatectomy and needle biopsy specimens.
Since the initial studies by Kovi et al and McNeal et al, several other studies have investigated IDC-P in radical prostatectomy and consistently found that the presence of IDC-P correlated with other adverse pathologic features, including higher Gleason score, larger tumor volume, and greater probability of extraprostatic extension, seminal vesicle invasion, and pelvic lymph node metastasis. It also correlated with decreased progression-free survival and with postsurgical, biochemical recurrence.,,
Only a few studies to date have examined the significance of IDC-P in needle core biopsy specimens, and, in 2 of these studies, IDC-P was present without associated invasive carcinoma in the biopsies,, an exceedingly rare finding, involving less than 0.06% of all prostate biopsy specimens.
Based on their studies of needle biopsy with IDC-P and previous studies in the literature that demonstrated consistent association of IDC-P at radical prostatectomy with multiple adverse prognostic factors, Robinson and Epstein recommend definitive therapy in men with IDC-P on needle biopsy, even in the absence of pathologically documented, invasive PCa.
Is Male Breast Cancer A Risk Factor For Prostate Cancer
Abhyankar et al. looked at the SEER database of 5,753 male breast cancer cases diagnosed between 1988 and 2012. They found that 250 of these men developed prostate cancer during a median follow-up of 4.3 years. Given that prostate cancer is one of the most common cancers among men, the calculated risk of prostate cancer in patients with a previous history of male breast cancer is no higher than that of the general population.
However, the risk of developing prostate cancer in their lifetime increases 1.9-fold if they also carry a BRCA gene mutation. The risk increases further to 2.64-fold if the mutated gene is BRCA2 . Whether or not there is an association between prostate cancer and male breast cancer, it certainly is not straightforward and will be discussed further in the later part of this report, after our case presentation.
Don’t Miss: How To Get Prostate Checked Uk
What Is My Outlook
Many men will want to know how successful their treatment is likely to be. This is sometimes called your outlook or prognosis. No one can tell you exactly what will happen, as it will depend on many things, such as the stage of your prostate cancer and how quickly it might grow, your CPG your age, and any other health problems. Speak to your doctor about your own situation.
Most localised prostate cancer is slow-growing and may not need treatment or shorten a mans life. For many men who have treatment for localised prostate cancer, the treatment will get rid of the cancer. For some men, treatment may be less successful and the cancer may come back. If this happens, you might need further treatment.
For more information about the outlook for men with prostate cancer, visit Cancer Research UK. The figures they provide are a general guide and they cannot tell you exactly what will happen to you. Speak to your doctor or nurse about your own situation.
Carcinoma In Situ Vs Invasive Carcinoma
In contrast to carcinoma, or invasive cancer, carcinoma in situ has not yet invaded the basement membrane, and there is no stromal invasion. Other than thisthe fact that the cells have not yet broken through the supporting structure from which they beganthe cells appear the same as invasive cancer cells would appear under the microscope.
Read Also: Can You Still Have Prostate Cancer After A Prostatectomy
Carcinoma In Situ Vs Cancer
A million-dollar question lately, especially with controversy over the treatment of ductal carcinoma in situ or in situ breast cancer, is whether or not carcinoma in situ is really cancer. The answer is that it depends on who you talk to. Some physicians classify carcinoma in situ as non-invasive cancer and others may prefer calling it pre-cancer. The distinction would lie in knowing whether or not the CIS would progress to invasive cancer, and that, by definition, is not known. Nor are we apt to get answers soon, as it wouldn’t be ethical to simply watch large numbers of carcinoma in situ’s to see if they became invasive cancer and spread.
What Are The Treatments For Prostate Cancer
Your treatment options usually depend on your age, your general health, and how serious the cancer is. Your treatment may include one or more of options:
- Observation,which is mostly used if you are older, your prostate cancer isn’t likely to grow quickly, and you don’t have symptoms or you have other medical conditions. Your doctor will keep checking on your cancer over time so to see whether you will need to start treatment for the cancer. There are two types of observation:
- Watchful waiting means having little or no testing. If symptoms begin or change, you will get treatment to relieve them, but not to treat the cancer.
- Active surveillance means having regular tests to see if your prostate cancer has changed. If the tests show the cancer is starting to grow or if you develop symptoms, then you will have treatment to try to cure the cancer.
Also Check: Is Green Tea Good For Prostate
Inclusion And Exclusion Criteria
De-duplicated studies were screened for relevance, of which 114 were eligible for inclusion . These studies were divided into case reports and case series . The excluded studies met at least one of the following criteria: the article was a review or meta-analysis, editorial comment, letter or book chapter non-English language a basic science cancer biology article unavailable . Intra-ductal adenocarcinoma of the prostate and prostatic intraepithelial neoplasia -like ductal carcinoma of the prostate were both excluded as separate histopathological entities to DAC.
FIGURE 1
