What Gets Stored In A Cookie
This site stores nothing other than an automatically generated session ID in the cookie no other information is captured.
In general, only the information that you provide, or the choices you make while visiting a web site, can be stored in a cookie. For example, the site cannot determine your email name unless you choose to type it. Allowing a website to create a cookie does not give that or any other site access to the rest of your computer, and only the site that created the cookie can read it.
Lymph Node Dissection In Prostate Cancer: ‘jury Is Still Out’
M. Alexander Otto, MMS, PA
The role of pelvic lymph node dissection in patients with localized prostate cancer remains controversial. Although guidelines are increasingly recommending extended PLND alongside radical prostatectomies, the evidence to date has not clearly demonstrated a therapeutic benefit for this more invasive approach compared with limited dissection.
Now, two recent randomized controlled trials offer some clarity on the extended vs limited PLND debate.
Overall, the trials found no difference in biochemical recurrence after several years of follow-up in men randomly assigned to limited pelvic lymph node dissection vs more extensive dissection. Even so, the investigators did not rule out the role of extended dissection in nodal staging.
According to one study, published in August in European Urology Oncology, the “concept that comprehensive surgical removal of nodal micrometastasis halts the disease progression process cannot be considered to have been refuted.”
Researchers from the second trial, published in May in European Urology, found that “differences in early oncological outcomes were not demonstrated” between the extended and limited groups, but that more extensive dissection “provides better pathological staging.”
The Relationship Between The Number Of Lymph Nodes Resected And Prognosis
Heidenreich et al. reported that e-PLND could significantly reduce the cancer-specific mortality of prostate cancer . Many researchers have tried to reduce the number of resected nodes to reduce postoperative complications while ensuring tumor control. JI JD et al. reported data on 360 patients with localized prostate cancer who underwent open RP. A comparison of the progression-free survival after s-PLND to that after e-PLND revealed that the 5-year progression-free survival rates after s-PLND and e-PLND were 90.1 and 91.3% in the low-risk group, respectively. There was no significant difference between the survival rates. In contrast, there was a significant difference in the intermediate risk group and in the high-risk group . Abdollah et al. reported data on 315 cases of lymph node metastasis. They found that the ratio between the number of resected lymph nodes and the 10-year survival rates without CSM was 8:74.7%, 17:85.9%, 26:92.4%, 36:96% and 45:98%. CSM was significantly reduced when the number of resected lymph nodes was 14 or more.
Don’t Miss: Does An Enlarged Prostate Prevent Ejaculation
Number Of Positive Lymph Nodes And Prognosis
The extent of lymph node involvement appears to have prognostic significance, although the data supporting this observation have several limitations. The first limitation is the extent of lymphadenectomy performed: The more lymph nodes removed, the greater likelihood of finding positive lymph nodes. In most practices, once a single positive lymph node is identified, surgeons will abandon further lymphadenectomy . Hence, the true incidence of multiple lymph node involvement is unknown, potentially resulting in an artificially poorer reported outcome for patients who have a single lymph node metastasis.
Another challenge in interpreting studies that describe differences in outcomes based on the number of lymph nodes involved is that the actual numbers of lymph nodes are not always reported., Because of these reporting differences, it is not surprising that there are widely different conclusions reached by the various authors. Some conclude that, as a rule, lymph node involvement indicates metastatic spread of cancer and that local-regional treatment, at most, is palliative, , , while others conclude that, in patients with minimal lymph node disease, local-regional treatment may affect survival favorably., , –
| Study |
|---|
- Single lymph node. Single lymph node.
- ¶ Distant progression free.
- ** Cause-specific survival.
The Case For Rn1 Patients
Lymph node recurrent PCa after the primary treatment is considered an unfavorable situation, and systemic hormone therapy is the gold standard in this patient population.96 However, there are very few data on irradiation of recurrent LN disease. Elective LN irradiation combined with SRT boosts to the recurrent LN could reduce the risk of regional LN progression. This hypothesis has recently been strengthened by the results from a surgical study.58 In this study, only LNM detected by choline PET/CT were removed by the surgeon and no adjuvant therapy was delivered. All of the patients had a PSA response and 3 out of the 6 patients included had a lasting complete PSA remission after a median follow-up of 24 months. Preliminary results from a small study on stereotactic radiotherapy for isolated LN relapses diagnosed with 11C-choline PET-CT have also been published recently.97 Total doses ranged from 20 to 45 Gy given in 25 fractions. Rates of toxicity were low. After 19 months of follow-up, 8 of the 14 patients had no evidence of disease. Patients with progression had no in-field relapse. These pioneering results need to be confirmed, but are extremely promising. However, until more data on radiotherapy or surgery for recurrent LN disease are available, aggressive regional approaches should be considered investigational.
Read Also: How To Ejaculate From Prostate Massage
The Role Of Radical Prostatectomy In Management Of Pn+ Pca
Although direct comparison of different trials is a flawed approach, their collective results do provide interesting insights. At the same time as the EORTC was enrolling patients on protocol 30846, the Eastern Cooperative Oncology Group launched a randomized trial of immediate vs deferred ADT in patients who were found to have pathologically involved lymph nodes at the time of RP, but in contrast to the EORTC trial, these patients underwent RP and were randomly assigned to receive immediate, continuous ADT , or to be followed up and receive ADT when clinical recurrence was detected . With a median follow-up of 11.9 years, median overall survival was 13.9 vs 11.3 years in the immediate-ADT and delayed-ADT groups, respectively. In the immediate-ADT group, 41% of patients died of PCa compared with 89% in the delayed-ADT group.
TABLE
Outcomes for Patients Treated With Various Combinations of Androgen Deprivation Therapy and Local Therapies for Lymph NodePositive Prostate Cancer
The Jury Is Still Out
In a addressing both studies, editorialists praised the investigators for their efforts to address an important clinical question, given that prior to these trials “prospective randomized trials on this topic were nonexistent.”
However, the editorialists, led by Gaëtan Devos, MD, a urology resident at University Hospitals Leuven in Leuven, Belgium, noted that “until mature results on hard endpoints are reported, the jury is still out for limited vs extended PLND.”
One of the problems is that most patients in both trials had low- or intermediate-risk prostate cancer, “a population probably benefiting the least from extended PLND.”
The low detection rate of positive lymph nodes in both studies 10% in the Brazil trial and 12.6% in the Memorial Sloan Kettering study reflects this “nonideal patient selection,” according to the editorialists, who noted the improved survival among high-risk men in the Brazil trial.
The editorialists called for a follow-up study that would compare extended PLND vs no PLND in high-risk disease, similar to a 2019 randomized controlled trial in advanced ovarian cancer. This ovarian cancer study found no survival benefit with pelvic and para-aortic lymphadenectomy following macroscopically complete resection with normal lymph nodes before and during surgery.
For more from Medscape Oncology, join us on and
Read Also: When Should You Have A Prostate Biopsy
Imaging Guided Surgery To Improve The Detection Of Lymph Node Metastases In Prostate Cancer Patients
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government.Know the risks and potential benefits of clinical studies and talk to your health care provider before participating. Read our disclaimer for details. |
| First Posted : April 6, 2021Last Update Posted : August 25, 2021 |
Potential participants will be identified, screened and recruited by the Urologists working at the Department of Urology, IRCCS San Raffaele, Milan, Italy. A total of 100 patients affected by PCa with a risk of LNI > 5% according to the Briganti nomogram and planned to receive RARP with an ePLND according to the European Association of Urology guidelines will be identified and enrolled in the study.
The patient must personally sign and date the latest approved version of the Informed Consent Form before any trial specific procedures are performed.
- The exact nature of the trial
- The surgical procedures
All procedures will be performed through a trans-peritoneal approach using the Da Vinci Xi robotic Surgical System. The patient will be placed in a Trendelenburg position. After incision of the peritoneum, release of the bladder laterally to the endopelvic fascia, the ureter will be localized.
The Case For Pn1 Patients
No randomized controlled study has ever tested the role of adjuvant RT in node-positive patients after RP and ePLND. In a large retrospective study, the role of adjuvant pelvic RT in the case of LN involvement after PR and ePLND was investigated. One hundred and twenty-one patients treated with adjuvant standard hormone therapy were compared with 129 patients treated with WPRT combined with HT. With a median follow-up of 95.9 months, the rates of biochemical recurrence-free and cancer-specific survival at 10 years were 53% and 80%, respectively. In multivariate analysis, no adjuvant RT and the number of positive LN were strong predictors of failure.95
Read Also: How To Detect Prostate Cancer Early
Comparison Of Different Local Nodal Treatments Or Observation
Two prospective, randomized, multicenter phase II trials were recently published in recurrent prostate cancer, comparing surveillance or metastasis-directed therapy . In the STOMP trial, patients with up to three PET-positive metastatic lesions, including 55% lymph node metastasis in both groups, were included. MDT included SABR in most patients , but also surgery . At a median follow-up of 3 years, the median ADT-free survival was 13 months in the surveillance group and 21 months in the MDT group . In the intention-to-treat analysis, a significant difference was only found for nodal metastases .
The ORIOLE trial also included patients with up to three metastatic lesions in conventional imaging, randomized 2:1 to SABR or observation. In 61%, metastatic lesions included only lymph nodes. Biochemical or clinical progression at 6 months occurred in 19% of patients receiving SABR and 61% undergoing observation . Total regression of PSMA radiotracer-avid disease decreased the risk of new lesions at 6 months . SABR was suggested to induce a systemic immune response. The presence of high-risk mutations in circulating tumor DNA might be associated with a worse prognosis .
Clinical Lymph Node Metastatic Prostate Cancer
Patients with suspicious lymph nodes at imaging represent approximately 12% of all new PCa diagnosis.2 This rate is likely to increase within the next few years given the greater utilization of advanced preoperative imaging ,3 and a trend towards higher rates of newly diagnosed non-local confined disease observed during the past decade.4 The presence of clinical nodal metastases is associated with detrimental oncologic outcomes. As such, patients with node positive PCa are considered to have stage IV disease based on the National Comprehensive Cancer Network guidelines.6 In these guidelines, no distinction is made between distant metastatic disease and lymph node metastatic disease . Therefore, systemic therapies should be considered in PCa patients with suspicious lymph nodes at diagnosis.7
Also Check: What Is A Good Psa Reading For Prostate
Read Also: Can You Really Milk A Prostate
Anatomy And Observation Of The Pelvic Lymph Nodes In The Cadaveric Specimens
All 30 adult male cadavers underwent pelvic lymph node dissection by the same anatomists , and all nodes were counted and recorded by a single pathologist . The boundaries of the lymph node dissection were as follows: the cephalic boundary was the bifurcation of the abdominal aorta the caudal boundary was the circumflex iliac vein and Cooper ligament the external boundary was the genitofemoral nerve and the posterior boundary was the internal iliac artery .
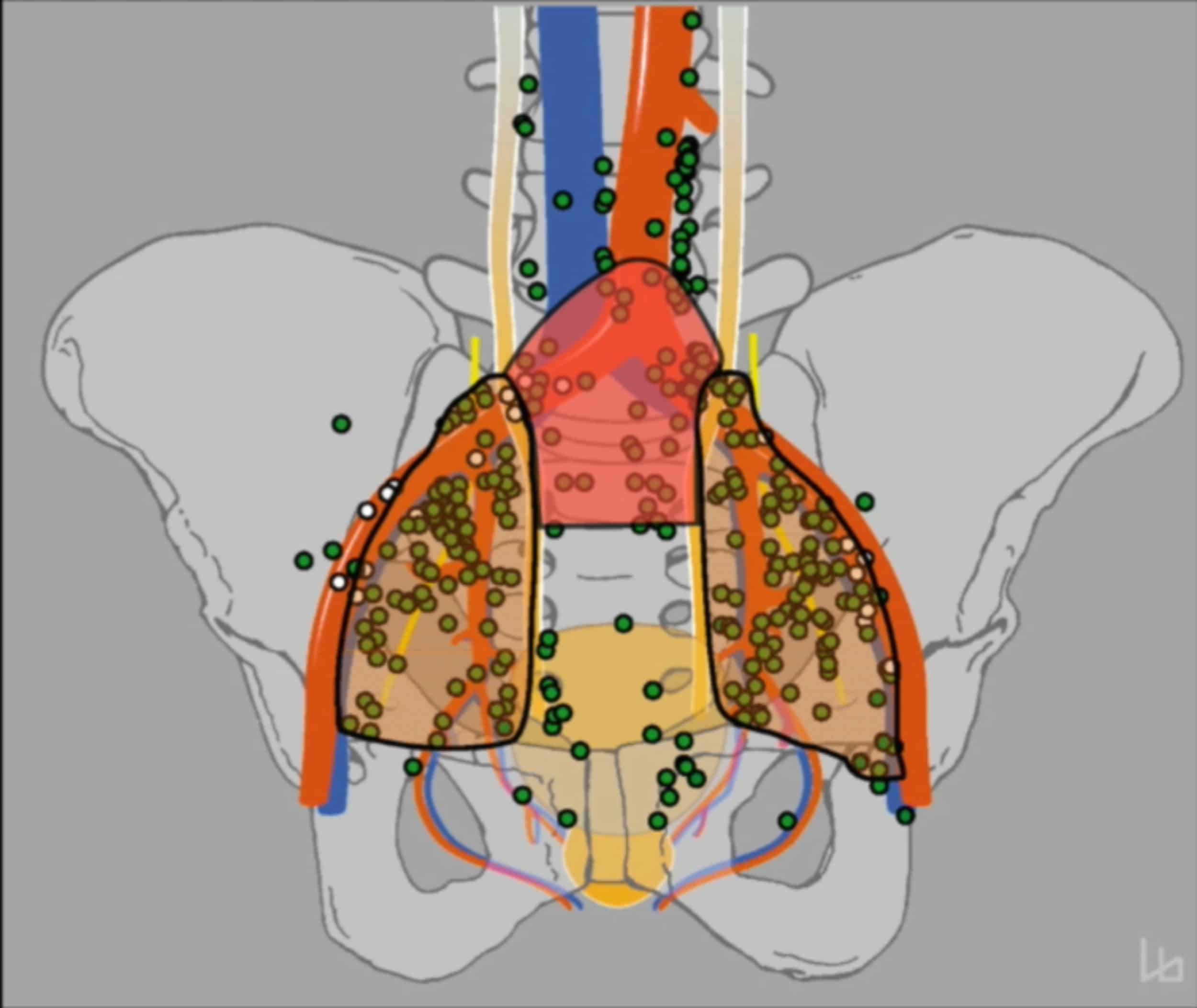
Fig. 1
Distribution of pelvic lymph nodes 1: presacral nodes 2: right common iliac nodes 3: left common iliac nodes 4: right external iliac nodes 5: left external iliac nodes 6: right obturator nodes 7: left obturator nodes 8: right internal iliac nodes 9: left internal iliac nodes
The tissue samples from each dissection zone were packaged separately and stored in 10% formalin solution until evaluation. Lymph nodes in adipose connective tissue are counted as follows: cut the tissue at intervals of 0.5cm , then use magnifying glass to distinguish and feel with fingers. Adipose lobules and small lymph node are not easy to distinguish in appearance sometimes, press with finger slightly, adipose lobule is easy to be crushed, have oily and lubricious feeling, while lymph node has capsule, not easy to be crushed. All lymph nodes were examined under a microscope.
Correlative Studies Linking Lymph Node Metastasis With The Lymphangiogenic Axis In Human Prostate Cancer
A number of clinical studies have examined the relationship between lymphangiogenesis and prostate cancer lymph node metastasis . These studies produced conflicting results. Although some detected lymphangiogenesis in prostate cancer tissues, which were correlated with lymph node metastasis, others failed to observe such a correlation. Interestingly, most of these studies have observed increased expression of VEGF-C in tumor tissues of prostate cancer patients with lymph node metastasis. The major point of dispute has been whether the increased expression of lymphangiogenic growth factors and their receptors, such as VEGFR-3, in prostate cancer tissues induced lymphangiogenesis for lymph node metastasis, or whether they might facilitate increased invasion of tumor cells into lymphatic vessels. Thus, we will discuss the major findings of each study and attempt to reconcile these conflicting results.
Dont Miss: How Many Radiation Treatments Are Needed For Prostate Cancer
Also Check: How Is Radiation Treatment For Prostate Cancer Done
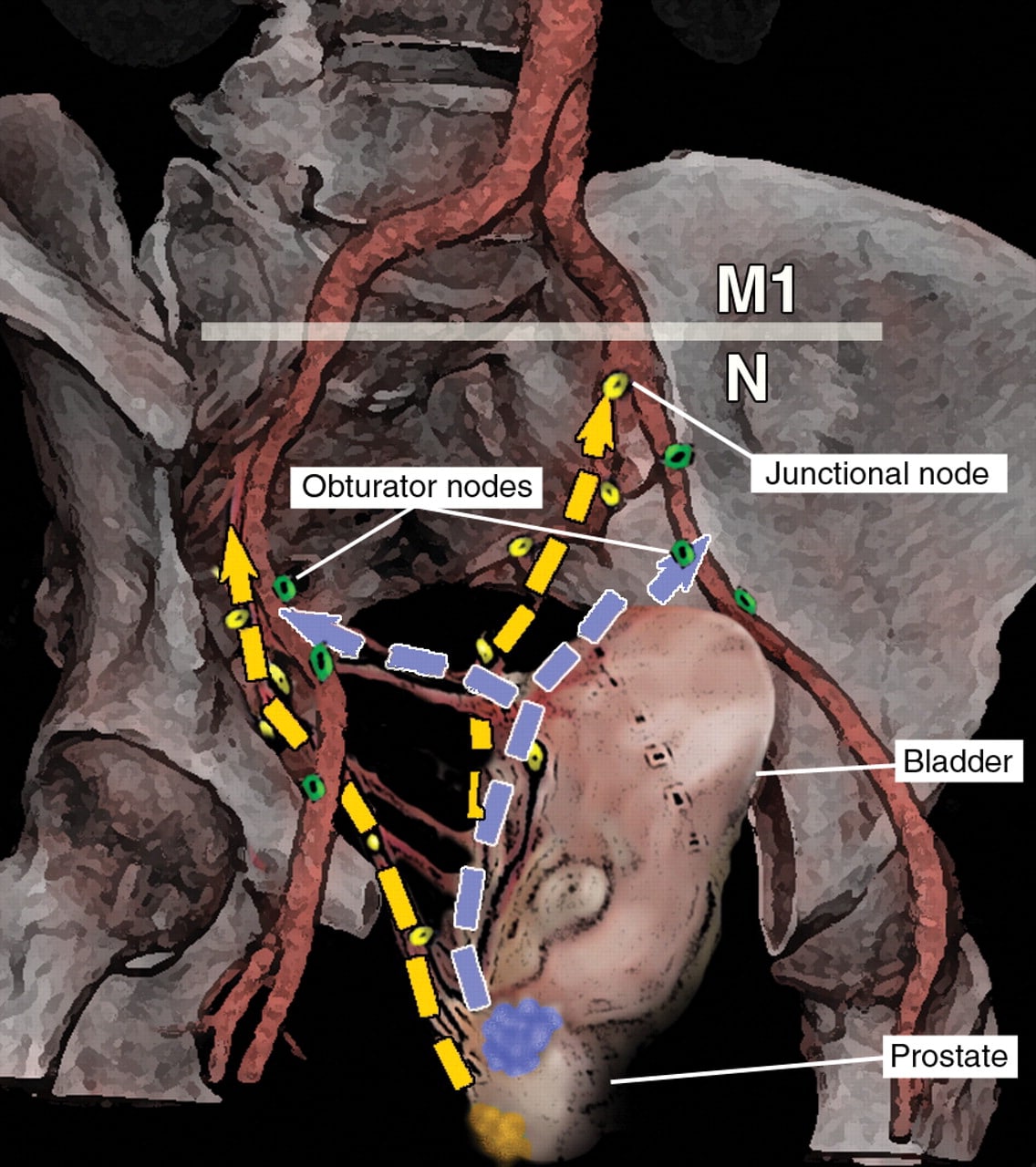
Lymph Node Mapping And Kernel Density Estimation
The geometric centers of pelvic nodes from all patients were mapped into a common template CT using an observer-independent non-rigid registration-based mapping technique . After mapping, distances between all lymph nodes from all patients were calculated and compared to the lymph node distances obtained via intra-patient measurements . The mean distance between involved pelvic lymph nodes was highly significantly smaller in individual patients than at a cohort-level , i.e., metastatic nodes were significantly closer. This was equally true, if distances between lymph nodes in individual patients were measured after being mapped into the common anatomy of the template dataset showing that the increase in mean lymph node distance at a cohort-level was not artificially introduced by the mapping procedure.
Figure 5 Three-dimensional renderings visualize the estimated three-dimensional probability density function of pelvic nodal metastases for the whole cohort in a common reference CT . CT atlas reconstructions . Left column: superior/axial view, middle column: left-side view/sagittal reconstruction, right column: anterior view/coronal reconstruction. Weighting was applied so that each patient case contributed equally to the estimate irrespective of the number of positive nodes.
Psma Pet/ct Imaging And Calculation Of The Roach Formula
PSMA imaging was performed with 3 different scanners: a Biograph mCT Flow was used for 192 patients , a Biograph 6 PET/CT for 85 , and a Biograph 20mT for 3 . All scans were performed according to previously published protocols . For 254 patients , 68Ga-PSMA-11 PET/CT was used, whereas 26 patients were imaged with 18F-PSMA-1007 PET/CT. Synthesis of 68Ga-PSMA-11 and 18F-PSMA-1007 followed the methods described by Eder et al. and Cardinale et al. , respectively.
PSMA PET/CT scans were interpreted by 2 board-certified nuclear medicine physicians and 1 board-certified radiation oncologist with regard to lymph node metastases. For image evaluation, tracer accumulation was considered positive if PSMA uptake in a node had a relevant difference from the background. Evaluation was done using Syngo TrueD and a dedicated workstation. All PSMA PET/CT scans were evaluated in consensus. A consensus reading was performed for 12 patients because of PSMA uptake within the ureter.
The risk for LNI was calculated according to the Roach formula for every patient included in this study. We compared the probability derived from the Roach formula with the results of PSMA PET/CT imaging.
You May Like: Does Super Beta Prostate Really Work
Understanding Prostate Cancers Progression
To determine the appropriate treatment, doctors need to know how far the cancer has progressed, or its stage. A pathologist, the doctor trained in analyzing cells taken during a prostate biopsy, will provide two starting pointsthe cancers grade and Gleason score.
- Cancer grade: When the pathologist looks at prostate cancer cells, the most common type of cells will get a grade of 3 to 5. The area of cancer cells in the prostate will also be graded. The higher the grade, the more abnormal the cells.
- Gleason score: The two grades will be added together to get a Gleason score. This score tells doctors how likely the cancer is to grow and spread.
After a biopsy confirms prostate cancer, the patient may undergo additional tests to see whether it has spread through the blood or lymph nodes to other parts of the body. These tests are usually imaging studies and may include a bone scan, positron emission tomography scan or computed tomography scan.
Also Check: Do Men Need A Prostate
Clinical Staging Options For Lymph Node Involvement
Several user-friendly but sometimes sophisticated tools based on initial clinical and pathological characteristics have been developed to predict the risk of nodal involvement in patients.1014 These tools are useful for predicting the probability of finding positive nodes in populations of patients, but they cannot determine if and where nodes are involved in an individual. As a result, the use of these tools has generated a lot of controversy not only because of significant differences in the observed vs. expected rates of pathological stage in the modern era of lymph-node dissection, but also because of concerns about their clinical relevance.
Recommended Reading: How Many Weeks Of Radiation For Prostate Cancer
