Advantages And Disadvantages Of Surgery
What may be important for one person might be less important for someone else. The advantages and disadvantages of surgery may depend on your age, general health and the stage of your cancer.
Advantages
- If the cancer is completely contained inside the prostate, surgery will remove all of the cancer.
- The prostate is looked at under a microscope to give a clearer picture of how aggressive your cancer is,;whether it has spread;outside your prostate and if you need;further treatment.
- Your health professionals can get a good idea of whether your cancer was completely removed during surgery. Your;PSA;level should drop so low that its not possible to detect it at six to eight weeks after surgery.
- If there are signs that your cancer has come back or wasnt all removed, you may be able to have further treatment.
- Some men find it reassuring to know that their prostate has been physically removed, although you will still need to have;follow-up tests;to make sure no cancer cells have spread outside the prostate.
Disadvantages
What Kinds Of Surgeries Treat Urinary Incontinence After Your Prostate Is Removed
There are two types of surgery for urinary incontinence: the urethral sling and the artificial urinary sphincter. Usually, the incontinence needs to last for about one year after the prostatectomy to be sure there is not going to be further improvement before your healthcare provider suggests this type of therapy.
Penile Rehabilitation After Prostate Removal May Include:
- Prescription medications. Medications, called phosphodiesterase-5 inhibitors, work for many men unless their nerve bundles were damaged or removed. These medications include Viagra and Cialis.
- An injection. Your body makes prostaglandin E1, a substance that helps your body have an erection. A made-made version is now available. Your doctor can teach you to inject this at the base of your penis about 5-to-10 minutes before intercourse. The injection is virtually painless; this medication is also available as a suppository placed into the tip of your penis.
- Vacuum devices. These devices draw the air from around your penis. The vacuum created brings blood into your penis, creating an erection.
- Penile implants. A device is surgically implanted into your penis. Penile implants provide a lasting solution for ED, lasting 10 or 15 years. There are risks, but if none of the other penile rehabilitation methods work, many men agree that a penile implant is a cosmetically-acceptable solution for their prostate cancer-related erectile dysfunction.
Don’t Miss: What Happens If Prostate Cancer Goes Untreated
Going Home With A Catheter
You will be discharged from the hospital with a catheter in place to drain urine from your bladder into a bag. The doctor will remove this in the office in five to 14 days. Be sure to clean the catheter where it exits your penis twice a day with soap and water and to empty the bag frequently. The bag should always be positioned lower than your bladder.
On occasion, the catheter may irritate the bladder, causing bladder spasms that can be quite uncomfortable. If these occur, your doctor can prescribe medication that can help. Leakage of urine around where the catheter exits the penis also may occur and can be managed by wearing incontinence pads as described in the next section.
It is normal for your urine to look cloudy for a few weeks after surgery. Occasionally, bleeding may occur around the catheter or be noticed within the urine. This also is common. If you see large clots â more than an inch in length â or if the catheter becomes plugged, contact your doctor. No anesthesia is required for catheter removal, and most patients experience only a little discomfort.
What Happens After Urethral Sling Surgery
Patients usually recover from this surgery quickly. It’s best to limit demanding activities for approximately six weeks after surgery to avoid having the sling loosen before healing is complete.
After surgery, there may be swelling that makes it difficult to urinate. You’ll have a catheter coming out of the urethra for two to three days. After this, the catheter is removed and just about everyone is able to void on their own. In rare cases, the catheter may have to be reinserted for a few days or up to a week if you cannot urinate.
After the swelling goes down, youll gradually be able to urinate on your own and empty your bladder. However, your normal urination pattern may not return for a few weeks.
The majority of men who’ve had this procedure have been cured of their urinary incontinence and no longer use pads. The others usually improve to the point where they don’t use as many pads as they were before.
Last reviewed by a Cleveland Clinic medical professional on 10/31/2020.
References
Recommended Reading: How To Pleasure A Woman After Prostate Surgery
Caring For Your Incision
The incision runs from above the base of the pubic area to below the navel. It is important to keep it clean and dry. Showering once a day should be sufficient. If you notice extreme or increasing tenderness, progressive swelling, more than a small amount of drainage or any pus or redness, notify your doctor right away.
What Is An Artificial Urinary Sphincter And How Does It Help With Urinary Incontinence
An artificial urinary sphincter can help men who have moderate to severe urinary incontinence due to poorly functioning muscle or sphincter valve after prostate cancer surgery.
The AUS has three parts:
- An inflatable cuff that is placed around the upper urethra. The cuff closes off the urethra to prevent leakage of urine.
- A pump that is inserted into the scrotum. It’s completely on the inside and not visible, and the pump controls the opening and closing of the cuff.
- A small pressure-regulating balloon that is placed in the abdomen, under the muscles. The balloon maintains fluid under pressure within the urethral cuff to pressurize the system and hold urine back.
If you have this surgery, youll press on the pump when you feel the need to pee. This opens the cuff to allow urine to pass. When youre done peeing, the cuff automatically closes again on its own.
The AUS procedure provides a very good and satisfactory result in 90% of cases. Risks are uncommon and include:
- Failure of the device .
- Erosion of the cuff into the urethra.
- Infection.
All of these would require additional surgery.
Also Check: Does Enlarged Prostate Cause Constipation
The Benefits Of Robotic Surgery
MRI technology helps us precisely visualize where the cancer is located and whether it is spreading. Based on this information, as well as a patients age, overall health, and personal preferences, prostate cancer treatment can include:
- Surgery
- Radiation
- Medication
Surgery is typically the best way to remove the cancer, and MedStar Health continues to lead the Mid-Atlantic region in robotic surgery expertise. Using the da Vinci® surgical robot system, I have performed over 3,000 robotic nerve-sparing radical prostatectomies to treat prostate cancer by removing the entire prostate.
Robotic surgery uses small incisions in the abdomen, through which the surgeon inserts tiny instruments. The robots movements mimic the human wrist but with greater dexterity, and its small camera provides a 3-D, magnified view of the prostate and surrounding tissue. Using a console to guide these instruments with extreme precision, we remove the prostate with minimal disruption to the surrounding healthy nerves and tissue that support normal urination and erection.
- A faster return to your normal urinary and sexual function
- Lower risk of surgical site infection
- Less blood loss
- Less pain overall
Psa Doubling Time Is More Accurate Than Gleason Score
Detecting recurrence with PSA at the earliest possible stage creates an opportunity to determine the seriousness of the relapse. With repeated, sequential testing of PSAsay with monthly blood drawsthe rate of PSA increase can be accurately determined. How quickly the PSA doubles reveals the grade of relapse. This information is very important because low-grade relapses are treated very differently than high-grade relapses.
Most people are familiar with the Gleason grading system, the most popular methodology for cancer grading in newly diagnosed men, that is, prior to relapse. With the Gleason system, the cancer cells are graded by a special doctor called a pathologist. The pathologist views the biopsy specimen under a microscope and assigns a grade to cancer. The Gleason system is the most powerful prognostic indicator for grading newly-diagnosed prostate cancer and has a very important role in determining optimal treatment for newly diagnosed men. However, in relapsed prostate cancer, the PSA doubling time easily supersedes the accuracy of the Gleason score. Knowledge of the cancers growth rate is the most accurate way to grade the cancers aggressiveness, and, luckily, the PSA determines this with unparalleled exactitude.
Once the PSA doubling time reveals the severity of the relapse, a treatment strategy is implemented. Treatment varies drastically depending on the grade of relapse, so the optimal;type of treatment for each grade of relapse is discussed below.
Don’t Miss: External Prostate Massage For Prostatitis
How Radical Prostatectomy Affects A Relationship
A 2011 study of 63 men that had undergone a radical prostatectomy found that about 75 percent of them sought treatment for erectile dysfunction. Additionally, more than 50 percent reported having less sexual desire, and roughly an additional 40 percent were unable to have a satisfying orgasm.;
The mental health effects of these symptoms were worse in highly sexually motivated participants. 52 percent reported that this had affected their self-esteem, and 36 percent said having performance anxiety.;
Additionally, the last three items on the list above can be show-stoppers for a relationship. Few women can tolerate a high degree of urine leakage during sexual activity, and few men can handle the pain during intercourse.;
Newly Diagnosed With Prostate Cancer Why Choose Robotic Prostatectomy
When first diagnosed with prostate cancer, its common for men to wonder what the future will hold. Certainly, a prostate cancer cure is a top priority, but then what?
Dr. David Samadi understands that men want to know:
-
Will I have sex after prostate cancer?
-
How will sex after prostate cancer be different?
For many men, prostate cancer treatment choice determines these answers.
If you select robotic prostate surgery your chances of enjoying sex after prostate surgery are very high. Robotic prostatectomy is a minimally invasive prostate removal. It is considered one of the best treatment options for prostate cancer due to its success rate and fast recovery rate.
The da Vinci robotic prostate cancer surgery system enables the surgeon to make precise movements. This ensures cancer-removal efficiency and sparing of the nerves and muscles that are responsible for the sexual function.
However, it is absolutely critical to choose a robotic surgeon with a high case volume and extensive prostate surgery experience. The robot does not perform the surgery and technology is no guarantee of success.
Dr. Samadi explains how the preservation of sexual function is possible:
If my only responsibility was to remove the cancerous prostate, my job would be much easier, he acknowledges, But patients deserve much more than that. It was paramount that I find a way to remove the prostate gland without damaging functions critical to a comfortable and enjoyable life after recovery.
Also Check: What Happens To The Prostate Later In Life
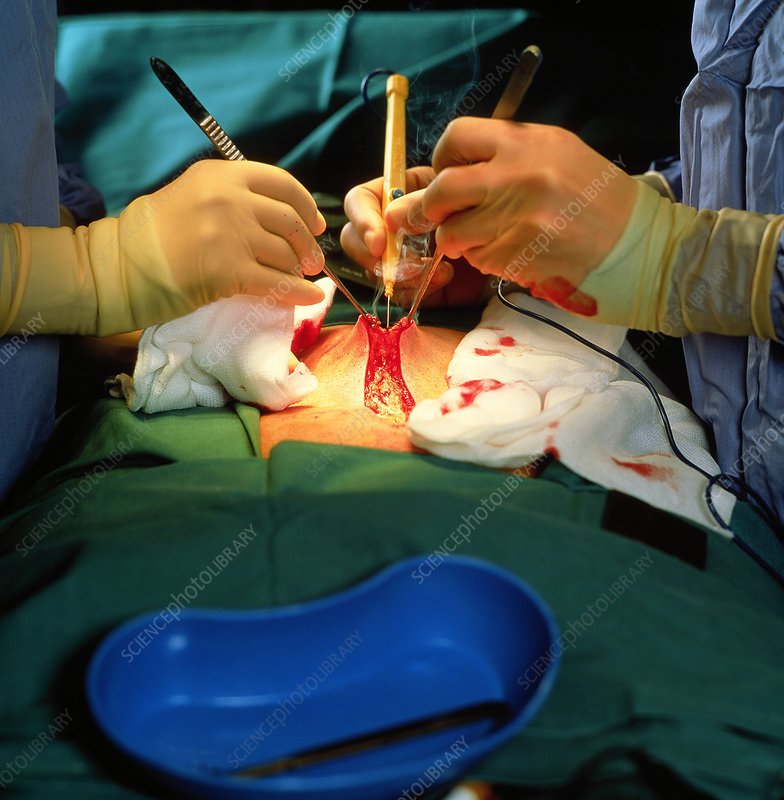
Radical Prostatectomy Retropubic Or Suprapubic Approach
You’ll be positioned on the operating table, lying on your back.
An incision will be made from below the navel to the pubic region.
The doctor will usually perform a lymph node dissection first. The nerve bundles will be released carefully from the prostate gland and the urethra will be identified. The seminal vesicles may also be removed if necessary.
The prostate gland will be removed.
A drain will be inserted, usually in the right lower area of the incision.
Day Before Your Surgery

Follow a light diet
Follow a light diet, such as a small sandwich, eggs, toast, crackers, or soup. Limit the amount of dairy products you eat and drink, and avoid fried foods and foods with a lot of seasoning.
Note the time of your surgery
A staff member from the Admitting Office will call you after 2:00 pm the day before your surgery. If your surgery is scheduled for a Monday, theyll call you on the Friday before. If you dont get a call by 7:00 pm, call .
The staff member will tell you what time to arrive at the hospital for your surgery. Theyll also remind you where to go.
Do your bowel preparation
The night before your surgery, use a saline enema as instructed on the box.
Shower with a 4% CHG solution antiseptic skin cleanser
The night before your surgery, shower using a 4% CHG solution antiseptic skin cleanser.
Sleep
You May Like: Does An Enlarged Prostate Affect A Man Sexually
Psa Recurrence Or Psa Persistence After Prostate Removal How To Interpret The Data
Although PSA should be 0 after surgery, some patients are faced with one of two scenarios: PSA recurrence or PSA persistence.PSA persistence is the detection of a PSA higher than 0 within the first three months after prostatectomy. The distinction is that the PSA has not recurred, but rather persisted after surgery. The key difference this small distinction makes is the prediction of the course the disease will take. A persistent PSA after radical prostatectomy or other forms of treatment can, unfortunately, mean cancer has progressed and metastasized. In many cases, the best course of secondary treatment is hormone therapy.
Unlike PSA persistence, PSA recurrence is characterized by a PSA of 0 postoperative and a rising in the blood test after an unspecified period of time. Traditionally, the value of 0.2 has been used as the benchmark to indicate PSA recurrence.
Why Is The Prostate Removed
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
Ask U.S. doctors your own question and get educational, text answers â it’s anonymous and free!
HealthTap doctors are based in the U.S., board certified, and available by text or video.
Don’t Miss: Is Viagra Good For Enlarged Prostate
Gene And Protein Expression
About 20,000 protein coding genes are expressed in human cells and almost 75% of these genes are expressed in the normal prostate. About 150 of these genes are more specifically expressed in the prostate with about 20 genes being highly prostate specific. The corresponding specific proteins are expressed in the glandular and secretory cells of the prostatic gland and have functions that are important for the characteristics of semen. Some of the prostate specific proteins, such as the prostate specific antigen , and the Prostatic acid phosphatase.
In the developing embryo, at the hind end lies an inpouching called the cloaca. This, over the fourth to the seventh week, divides into a urogenital sinus and the beginnings of the anal canal, with a wall forming between these two inpouchings called the urorectal septum. The urogenital sinus divides into three parts, with the middle part forming the urethra; the upper part is largest and becomes the urinary bladder, and the lower part then changes depending on the biological sex of the embryo.
What To Expect After Surgery
A prostatectomy is major surgery from which your body needs time to recover. Your doctor will discuss the details of your recovery with you.
Typically patients stay in the hospital overnight after surgery and then need to recuperate at home for a month before returning to work. Most men can start to drive a few weeks after surgery. You should avoid heavy lifting for several weeks after surgery. It usually takes about six weeks for most men to feel back to normal.
This page provides general information about what you can expect in the first hours and days right after surgery. You may also want to read more about:
Read Also: Can Prostatitis Go Away On Its Own
Facts About Prostate Removal Surgery
Prostate cancer surgery can be extremely concerning for many patients. You may be wondering how your surgery will be performed because of your prostate glands location. Youll probably have questions about pain and the side effects including questions about your sexual life afterward and your ability to control urine. ;
The good news is that todays technology offers minimally-invasive prostate removal surgery. The method is known as Robotically Assisted Laparoscopic Radical Prostatectomy . RALP is the most often used surgical method for prostate cancer. The da Vinci robotic system allows surgeons to use one or more small incisions for your surgery. Surgeons use a high-magnification 3D camera system to help them operate with accuracy.
Who Should Undergo Radical Prostatectomy
Men younger than age 75 with limited prostate cancer who are expected to live at least 10 more years tend to get the most benefit from radical prostatectomy.
Before performing radical prostatectomy, doctors first try to establish that the prostate cancer has not spread beyond the prostate. The statistical risk of spread can be determined from tables comparing the results of a biopsy and PSA levels. Further testing for spread, if needed, can include CT scans, bone scans, MRI scans, and ultrasound.
If it appears that the prostate cancer has not spread, a surgeon may first offer other options besides surgery. These can include radiation therapy, hormone therapy, or simply observing the prostate cancer over time, since many prostate cancers grow slowly. Depending on how high the risk of cancer spread, pelvic lymph node dissection may be considered, as well.
Don’t Miss: Does Cialis Shrink The Prostate
