G Car T Cells Become Exhausted During In Vitro Expansion
During in vitro culture and restimulation, 2G CAR T subset progressively expanded and accumulated up to 6 weeks, the last time point tested. Conversely, 3G CAR T cells strongly reduced their proliferation by week 4 from transduction, with a significant difference in the total CAR T cell yield from day 25 to day 40 . By day 25, furthermore, CD28–4-1BB CAR T cells showed a cell surface profile consistent with exhaustion, including a higher and significant difference in the expression of PD-1 , TIM-3 and LAG-3 , as compared to the 2G CAR T cell population . Moreover, 3G CAR T cells showed higher rates of apoptosis in comparison to the 2G CAR T cell population, likely associated to the induction of the FAS-FASL pathway . In addition, at these late stages of culture 3G CAR T cells produced lower levels of IL-2, TNF-, and IFN- following exposure to PSMA+ cells, as compared with 2G CAR T cells . Together, these phenotypic and functional data demonstrate that 3G CAR T cells become rapidly exhausted and have a limited expansion during in vitro culture, whereas similar effects do not occur in 2G CAR T cells stimulated in the same manner.
Problems Relating To Use Of Car
The use of CAR-T cells for the treatment of non-hematological tumors exposes the patient to risks that could limit their use in clinical practice. Perhaps the most important risk is the presence of several structures in solid tumors that limit the contact between CAR-T cells and the tumor itself . For example, bone is the most frequent site of PCa metastasis. Within this context, the tumor microenvironment enhances aberrant angiogenesis mediated by vascular endothelial growth factor receptor . Shi et al. demonstrated that a combination of immunotherapy and angiogenesis-normalizing treatments increases the efficacy of immunotherapeutic agents .
More recently, some authors evaluated the possibility of inserting a chemokine receptor gene into CAR-T cells. For example, engineering CXCL12 ligand, i.e. C-X-C motif receptor -4, into CAR-T cells could increase the percentage of CAR molecules reaching reach tumor cells .
How Much Does Car T
China is a world leader in number of clinical trials for CAR-T cell therapy & BMT. Till now there are more than 300 CAR-T cell clinical trials in progress. Chinas CAR-T treatment is the most budget one around the world. Because the CAR-T cell preparation is free now ! The patients only have to pay for the treatment & services. Total cost of treatment will be around $30,000 -$40,000.
Don’t Miss: What Is The Function Of The Prostate Gland
At The 2017 Aacr Meeting Progress Was Reported On The Development Of Car T Cell Immunotherapy For Treating Glioblastoma And Prostate Cancer
Immune cells that are genetically engineered with designer molecules to recognize and kill cancer cells may sound like an episode of science fiction, and for solid tumors, they used to be until now. At the 2017 American Association for Cancer Research Annual Meeting, City of Hope National Cancer Center reported on results from the first study ever to successfully use Chimeric Antigen Receptor T cells to battle glioblastoma , as well as progress on a soon-to-enter-clinical-trials version for prostate cancer.
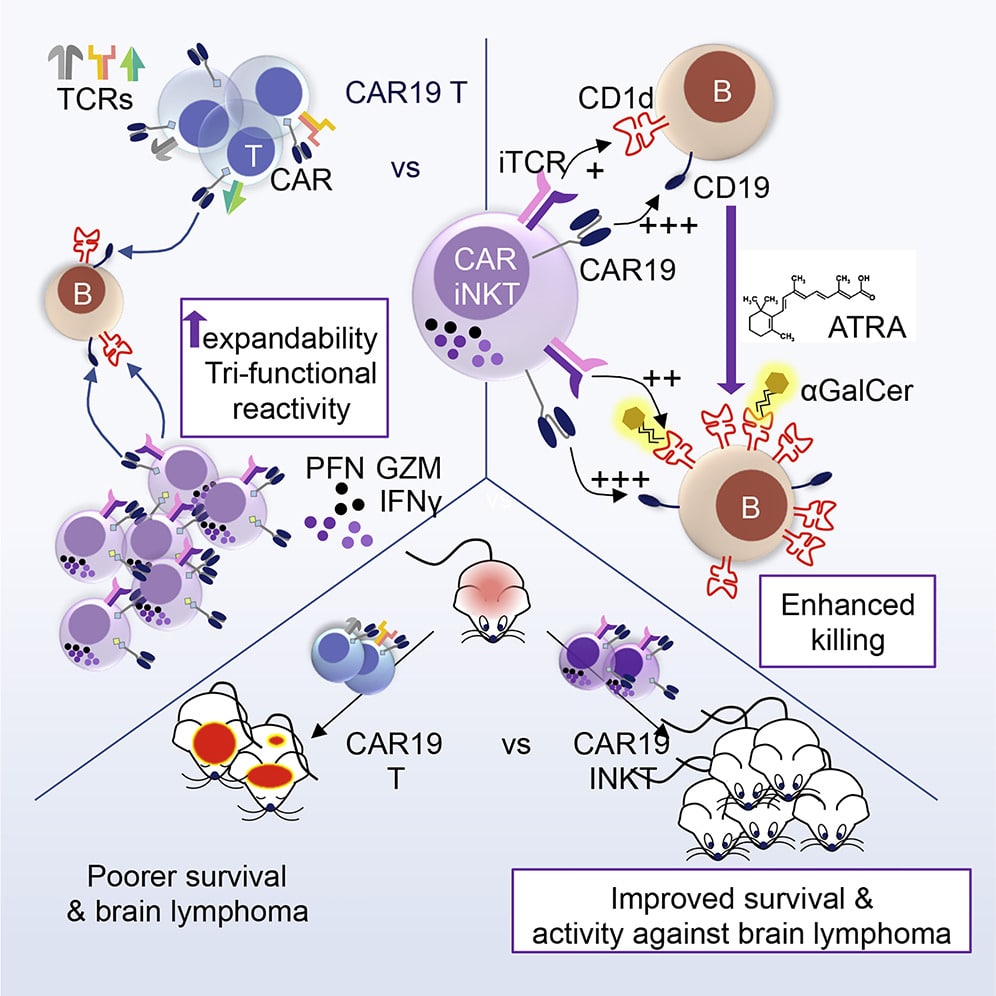
CAR T cells have previously made headlines for causing dramatic and long-term regressions in patients with certain types of leukemia and lymphoma. These CAR T cells were uploaded with a CAR that targets CD19, a gene specially expressed by B cells , which activates the CAR T cell to kill any cell encountered that expresses this target. Because of these successes, researchers have been racing to engineer CAR T cells that can target other tumor types. However, to limit side effects and maximize therapeutic potency, the CAR target selected needs to be specifically expressed by cancer cells and not cells that our bodies cant get by without, which has proven to be more challenging than it sounds.
Towards a New Era in Cell Engineering for Immunotherapy
The 2017 AACR Annual Meeting was held from April 1-5, 2017, in Washington, D.C.
First Effective Car T Cells Developed
The MSK team builds the first effective CAR T cells, targeted against a prostate cancer antigen. These second-generation CARs T cells are able to survive, proliferate, and kill prostate cancer cells in the lab, establishing the feasibility of CAR T cell therapy. An even more promising CAR target lay ahead.
You May Like: What Does Prostate Fluid Look Like
More Than Just Car T Cells: Tils And Tcrs
CAR T cells have garnered the lion’s share of attention when it comes to cellular therapies. But other types of cellular therapies have also shown promise in small clinical trials, including in patients with solid tumors.
One type, known as tumor-infiltrating lymphocytes , uses immune cells that have penetrated the environment in and around the tumor. Researchers at NCI were the first to use TILs to successfully treat patients with advanced cancerinitially in melanoma and later in several other cancers, including cervical cancer. More recently, NCI researchers have developed a technique for identifying TILs that recognize cancer cells with mutations specific to that cancer and identifying people whose cancers are more likely to respond to TIL therapy.
The other type of cellular therapy involves engineering patients’ T cells to express a specific T-cell receptor . Unlike CARs, which use portions of synthetic antibodies that can recognize specific antigens only on the surface of cells, TCRs use naturally occurring receptors that can also recognize antigens that are inside tumor cells.
To date, TCR T cells have been tested in patients with a variety of solid tumors, showing promise in melanoma and sarcoma.
Related Resources
G And 3g Car T Cells Show Comparable Tumor Cell Killing And Cytokine Production Following Exposure To Psma+ Cells
Both the 2G and 3G CAR populations lysed the PSMA-transfected PC3 cells at high levels . Moreover, they efficiently recognized LNCaP cells, a target that naturally harbors the PSMA antigen , while sparing the antigen-negative counterpart . Other than exerting a relevant cytotoxic activity, both generations of CAR-transduced T cells also produced high and comparable levels of IFN-, IL-2, and TNF- in response to PSMA-expressing tumor targets, but not against PSMA negative control cells .
Figure 3 Functional characterization of the 2G and 3G CAR-expressing populations. Lytic activity of the 2G and 3G -CAR expressing populations. Cytotoxicity was analyzed at day 15 post-transduction as target cells, PC3-PSMA, LNCaP, and PC3 were used. Cytokine release upon antigen stimulation. IFN-, IL-2 and TNF-. Cytokine release was evaluated 15 days after T cell infection by stimulating 2G and 3G CAR populations with PC3-PSMA or PC3 cancer cell lines. Negative and positive controls were represented by 2G and 3G CAR T cells treated or not with PMA/Ionomycin. Figures show the mean +/- SD of 3 independent experiments.
Don’t Miss: Do Women Get Prostate Cancer
Request An Appointment At Moffitt Cancer Center
Please call for support from a Moffitt representative. New Patients and Healthcare Professionals can submit an online form by selecting the appropriate button below. Existing patients can call . for a current list of insurances accepted at Moffitt.
NEW PATIENTS To request a new patient appointment, please fill out the online form or call 1-888-663-3488.
REFERRING PHYSICIANS Providers and medical staff can refer patients by submitting our online referral form.
Moffit now offers Virtual Visits for patients. If you are eligible for a virtual appointment, our scheduling team will discuss this option further with you.
Moffitt Cancer Center is committed to the health and safety of our patients and their families. For more information on how were protecting our new and existing patients, visit our COVID-19 Info Hub
Car T Cells Reach Clinical Milestone In Prostate Cancer
volume 28, pages 635636
Armored CAR T cells show early signs of clinical activity in patients with castration-resistant prostate cancer, paving the way for further development and optimization.
Cancer progression is often fueled by a preponderance of genetic aberrations such as mutations, amplifications and divergently expressed genes. These can lead to newly expressed peptides that are entirely absent from normal human tissues, or to peptides that are expressed at higher levels in tumors, but are also expressed at lower levels in other tissues the latter are known as tumor-associated antigens.
Don’t Miss: How To Massage Own Prostate
How You Can Support Dr Fraietta And Other Researchers Work
In addition to being an Alliance for Cancer Gene Therapy Fellow, Dr. Fraietta is an Assistant Professor of Microbiology at the University of Pennsylvania Perelman School of Medicine.
Dr. Fraiettas experience includes a postdoctoral fellowship under Carl June, MD, who created the first CAR T-cell therapy approved by the U.S. Food and Drug Administration. Dr. Fraietta was part of this scientific breakthrough for blood cancers and now aims to make CAR T cells effective against solid tumor cancers.
Please consider donating today to help Alliance for Cancer Gene Therapy create a cancer-free future. If youre not ready to donate yet, please look at some of the other cancer research programs the Alliance has funded over the past two decades.
This background hopefully helps you understand Alliance for Cancer Gene Therapys purpose, including the steps taken to give more cancer patients hope of longer survival. 100% of all private donations to Alliance for Cancer Gene Therapy go directly to research and programs.
T Cell Engineering Begins
As a postdoctoral student at the Whitehead Institute at MIT, immunologist Michel Sadelain begins using newly developed genetic engineering tools, specifically retroviral vectors, to introduce genes into T cells, with the goal of making souped-up cancer fighters. This idea would bear fruit in the coming years.
You May Like: Best Way To Check Prostate Cancer
Research Award Accelerates Research On Car T
According to the American Cancer Society, one in eight men will receive a prostate cancer diagnosis in his lifetime and about one in 40 will die as a result. A Keck Medicine of USC research team has now developed an innovative treatment for prostate cancer, known as synthetic immune receptor T-cell therapy. The new technology was adapted from chimeric antigen receptor therapy, which has been proven effective for several types of blood cancer.
Principal investigator Preet M. Chaudhary, MD, PhD, chief of the Jane Anne Nohl Division of Hematology and Center for Blood Diseases in the Department of Medicine, Bloom Family Chair in Lymphoma Research and director of Blood and Marrow Transplant and Cell Therapy at the Keck School, has been selected to receive a $5.8 million award from the California Institute for Regenerative Medicine to begin conducting preclinical studies of SIR-T therapy.
To continue reading this story, .
Challenges In Solid Tumours
Whilst CAR-T cell therapy has revolutionised the treatment of haematological malignancies, this success has largely not been repeated in solid tumours. The reasons for this are thought to be due to many factors .
Barriers in CAR-T cell therapy and strategies adopted in overcoming these barriers. Abbreviations: TGF-βâtumour growth factor beta TregsâT regulatory cells MDSCsâmyeloid-derived stem cells M2-MÏâM2 macrophages CAFâcancer-associated fibroblasts PD-1âprogrammed cell death type 1 PD-Lâprogrammed death ligand shRNAâshort hairpin RNA. Created with BioRender.com .
Unlike haematological malignancies, solid tumours express antigenic heterogeneity rather than monoclonality , and therefore some tumours in certain individuals may express a combination of antigens that may differ from another individualâs. Intratumoural heterogeneity is also common in prostate cancer hence, an individual tumour itself may display a wide variety of antigens. Furthermore, there is evidence that CAR-T treatment can induce antigen escape by means of adaptive resistance . Given the low tumour mutational burden and the antigenic heterogeneity, a useful approach is manufacturing CARs that target multiple antigens. Kloss et al. and Feldmann et al. created CARs that target PSCA and PSMA, demonstrating effective results .
Read Also: How Fast Does Prostate Cancer Progress
Understanding And Managing The Side Effects Of Car T
Like all cancer treatments, CAR T-cell therapies can cause severe side effects, including a mass die-off of antibody-producing B cells and infections. One of the most frequent and serious side effects is cytokine release syndrome .
As part of their immune-related duties, T cells release cytokines, chemical messengers that help stimulate and direct the immune response. In the case of CRS, the infused T cells flood the bloodstream with cytokines, causing serious side effects, including dangerously high fevers and precipitous drops in blood pressure. In some cases, severe CRS can be fatal.
Ironically, CRS is considered an “on-target” effect of CAR T-cell therapythat is, its presence demonstrates that T cells are at work in the body. Generally, patients with the most extensive amount of cancer in their bodies are more likely to experience severe CRS from CAR T cells, Dr. Kochenderfer explained.
In many patients, both children and adults, mild forms of CRS can be managed with standard supportive therapies, including steroids. And as researchers have gained more experience with CAR T-cell therapy, they’ve discovered ways to better manage the more serious cases of CRS.
A big part of that management is the drug tocilizumab . This drug, initially used to treat inflammatory conditions like juvenile arthritis, blocks the activity of IL-6, a cytokine that is often secreted in large amounts by T cells and macrophages.
Inclusion Criteria For Car T
1. Patients with CD19+ B-cell Lymphoma
2. To be aged 3 to 75 years
3. ECOG score 2
4. Women of childbearing potential must have a urine pregnancy test taken and proven negative prior to the treatment. All patients agree to use reliable methods of contraception during the trial period and until follow-up for the last time.
Also Check: What Is Prostate Removal Called
Are Chimeric Antigen Receptor
COVID-19 has affected everything we do in medicine and science. This certainly includes cancer research, and many clinical trials have placed temporary holds on patient accrual to reserve hospital/intensive care unit beds, preserve personal protective equipment, and limit person-to-person contact. However, we must be optimistic and start to plan for a future when the COVID-19 pandemic calms down. The first wave of clinical trials to reopen must importantly take into account the risk/benefit ratio for the patient.
The more dire the study population’s prognosis, the higher priority we ought to place on reopening relevant trials for patient accrual, especially if the therapeutic agent have promise for high efficacy. Not surprisingly, this first wave of trials will include many hematological malignancy trials, and that should include those with autologous cellular immunotherapies, such as CAR-T cells.
Yet as a genitourinary oncologist, I have a mild sense of envy on this topic of CAR-T cell therapy, as I hope for a day where our patients can be treated with these exciting therapies. Therefore, Ive focused this months article on considerations for developing CAR-T cell therapeutics for prostate cancer patients.
Prostate Cancer And Newer Therapies
In this case, the creation of genetically modified T cells capable of combating cancer immunological tolerance would mark a significant advancement in the study of cancer. Clinical trials have been conducted to confirm the viability of employing chimeric antigen receptor T cells to recognise and eradicate malignant cells in the present new era of cancer immunotherapy. A tumour antigen-binding domain linked to an intracellular signalling domain and costimulatory molecules make up the CAR-T molecule. For this reason, unlike T cell receptor -mediated antigen recognition, antigen identification is not constrained by the major histocompatibility complex .
We give a thorough overview of CAR-T cell therapy for PCa in this study and make recommendations for ways to further enhance the present outcomes.
Don’t Miss: How To Know If You Have A Prostate
About Car T Cell Therapy
CAR therapies utilize T-cells , a patients own immune cells that are removed from the body and re-programmed to recognize and kill cancer cells throughout the body. The process involves the removal of some T cells from a patient, and through laboratory processes these T cells are re-programmed to identify and attach a patients cancer cells. CAR T cells appear to represent a significant advance in cancer treatment are already FDA approved for the treatment of lymphomas, myeloma and leukemia. Research is ongoing to see if this novel treatment approach can be effectively developed to treat solid cancer types like prostate cancer.
- Learn About CAR T Cell Therapy
Researchers from MSKCC presented interim results from a dose finding clinical trial in 14 evaluable patients treated at 3 different CAR T cell dose levels. All patients in the trial received a standard lymphodepletion regimen consisting of fludarabine and cyclophosphamide, prior to a single infusion of P-PSMA-101 CAR T Cells. Patients in the trial were heavily pre-treated, having received an average of seven prior lines of therapy with a median time since diagnosis of 6.4 years.
Key findings from the trial included:
- 10/14 patients demonstrated measurable declines in PSA levels
- 5/14 patients showed a decline in PSA levels of 50% or more
- One patient demonstrated evidence of complete tumor elimination and remains in a durable response of greater than ten months at the time of this presentation
Reference
The Molecular Structure Of Car
The CARs are fusion proteins constructed by modern molecular biotechnology. CARs are generally composed of three parts: extracellular antigen identification zone, transmembrane zone, and intracellular signal transduction zone.5 The extracellular antigen identification zone is the basis of specific recognition of tumor antigens by CARs.6 Single-chain fragment variable of CAR-T cells can recognize tumor-associated antigen specifically. The transmembrane zone usually consists of the transmembrane region of CD3, CD8, CD28, or FcRI and can fix scFv on the surface of T cells and transduce the signal into the cells. The intracellular signal transduction zone is composed of CD8, CD28, or CD137 intracellular area and CD3, which contain the immune-receptor tyrosine-based activation motif . ITAM plays a crucial role in the transduction of signal to active T cells.
You May Like: How To Tell If You Have Prostate Problems
