What Can Be Done
If your prostate cancer has recurred, your healthcare provider will likely order some imaging tests to better determine where in your body the cancer has returned. Bone scans, CT scans, and MRIs are the most common tests ordered to find where in the body prostate cancer has recurred.
Many treatment options are available for prostate cancer that has returned. The one that you and your healthcare provider choose depends on individual factors such as what treatment you have already received, where in the body your prostate cancer has returned, how your cancer has spread, your general health, and your age.
If your prostate cancer is thought to have recurred in only a small area and has not spread to other areas of the body, then radiation therapy to that area may be an option.
If your prostate cancer has most likely spread to multiple areas of the body, then hormonal therapy would likely be an option. Chemotherapy can also be used when the cancer has spread to multiple sites.
What Happens If My Psa Rises After Surgery
If your PSA starts to rise after youve undergone prostatectomy, salvage radiation therapy might be a good option to explore, and has been shown to improve outcomes over time. With this approach, external beam radiation is delivered to the area immediately surrounding where the prostate was , with the aim of eradicating any remaining prostate cells that have been left behind. Depending on your PSA level, the addition of hormone therapy can improve outcomes with salvage radiation for details, please see Therapies for Locally Recurrent Prostate Cancer in PCFs Prostate Cancer Patient Guide. Clinical trials are investigating more aggressive systemic therapies.
What Is Hormone Therapy For Prostate Cancer
Hormone therapy is a key treatment strategy for prostate cancer that has recurred following treatment for localized disease. Testosterone is a male hormone that fuels the growth of prostate cancer cells. The goal of hormone therapy is to stop the production and/or interfere with the effects of testosterone. However, not all prostate cancer cells are sensitive to decreases in testosterone levels, and, over time, the cancer can adapt to survive in a low-testosterone environment. Therefore, hormone therapy is a treatment for prostate cancer but does not cure the disease. The decision to start hormone therapy is individualized, based on your PSA, the PSA doubling time, whether the cancer has spread visibly or caused symptoms, and the potential side effects and risks involved with this type of therapy.
Recommended Reading: Good Diet For Prostate Cancer Patients
What Are The Side Effects Of Hormone Therapy For Prostate Cancer
Testosterone is the primary male hormone and plays an important role in establishing and maintaining the male sex characteristics, such as body hair, muscle mass, sexual desire, and erectile function. Most men who are on hormone therapy experience at least some effects related to the loss of testosterone, but the degree to which you will be affected by any one drug regimen is impossible to predict. Side effects from testosterone-lowering therapies include hot flashes, breast enlargement or tenderness, loss of bone mineral density , weight gain , higher cholesterol, and a higher risk of diabetes and heart attack. Some men experience fatigue, memory loss, and/or depression. Dont be afraid to discuss these issues with your doctors. Maintaining a healthy lifestyle through good nutrition and exercise can help reduce the impact of these side effects.
Treating Prostate Cancer That Doesnt Go Away Or Comes Back After Treatment
If your prostate-specific antigen blood level or another test shows that your prostate cancer has not been cured or has come back after the initial treatment, further treatment can often still be helpful. Follow-up treatment will depend on where the cancer is thought to be and what treatment you’ve already had. Imaging tests such as CT, MRI, or bone scans may be done to get a better idea about where the cancer is.
Also Check: Why Does Prostate Gland Swell
What Are Antiandrogens And Should They Be Part Of My Treatment Plan
Antiandrogens can be helpful in preventing the flare reaction associated with LHRH agonists resulting from an initial transient rise in testosterone. They can help block the action of testosterone in prostate cancer cells. Their use for at least the first 4 weeks of LHRH agonist therapy can relieve the symptoms often seen from the flare reaction, ranging from bone pain to urinary frequency or difficulty. You should ask your doctor whether continuing these pills for longer-term cancer control might be beneficial for you.
Treatment Options After Recurrence
After surgery to remove your prostate
PSA levels are usually extremely low about a month after surgery. You may hear your doctor saying that your PSA level is undetectable . If your PSA level starts to rise, this might mean the cancer has come back.
Your doctor might recommend:
- radiotherapy to where the prostate was
- hormone treatment
After external beam radiotherapy
PSA levels usually get lower slowly over months or years. Saying at what level your PSA should be for cure is complicated and you should ask your cancer specialist. Usually a level of 2 ng/ml above the lowest point after treatment is taken as a sign of recurrence, or 3 increases in a row .
Your treatment options may be:
- surgery to remove your prostate
- hormone treatment
- high frequency ultrasound
After brachytherapy
PSA can rise temporarily after brachytherapy. This is called PSA bounce. The level then lowers slowly. Usually a level of 2 ng/ml above the lowest point after treatment is taken as a sign of recurrence.
After hormone treatment
If you are given hormone treatment alone, the PSA can rise after you finish hormone treatment. It may then become stable or static. If it rises this may suggest the cancer is becoming resistant to the hormone treatment.
If hormone treatment is no longer controlling your cancer, your doctor may suggest:
Also Check: What Is Your Prostate Gland For
Treatment Of Rising Psa
If PSA levels are rising slowly or by a small amount, a person may not need treatment. A doctor usually considers an individuals overall health, medical history, and age when giving advice on treatment.
Doctors often use active surveillance if PSA levels are rising. Active surveillance is a series of regular tests and health checks, with treatment only if necessary. Prostate cancer often progresses very slowly, so it may be many years before a person needs treatment.
If a person has had a prostatectomy, a doctor may also recommend radiation therapy, which kills cancer cells using high-energy particles.
Radiation therapy is not suitable for everyone who has had a prostatectomy. If a person had radiation therapy before surgery, they cannot usually have this treatment again. Having radiation therapy a second time can cause side effects.
Doctors may also use hormone therapy to shrink a persons tumors. This can make other treatments such as radiation therapy more effective.
It is not always possible to prevent PSA levels from rising. The best way to safeguard health after having a prostatectomy is by undergoing regular medical checks.
- stopping smoking or using tobacco products
- exercising regularly
- eating a healthful diet, with plenty of fruits and vegetables
- limiting alcohol intake to a moderate amount
Read Also: Sbrt Vs Surgery For Prostate Cancer
Disclosure Of Potential Conflicts Of Interest
No potential conflicts of interest were disclosed.
Grant support: We also acknowledge the financial support from our prior NIDDK George M. O’Brien grant, the Department of Defense Prostate Cancer Research Program grant , the NCI NW SPORE Prostate Cancer Grant , the Department of Veteran’s Affairs , and the Richard M. Lucas Foundation.
You May Like: Can Prostatitis Go Away On Its Own
Salvage Therapies After Failed Radical Surgery
To recap, the challenges with treating recurrence with radiation after failed prostatectomy are:
1. The target is no longer in place and this void becomes occupied by critical structures such as the bladder and rectum.2. Because of this postsurgical situation, only lower doses can be achieved.3. After surgery, the surgical bed is denuded of vessels , but radiation works best in a vascularized, oxygenated region. In theory, even higher doses are necessary than when the prostate is intact. Solution: Only the sophisticated technology of DART can achieve the required higher dose levels of radiation. Hormones are commonly used to work in synergy with radiation.
What Type Of Follow
If prostate cancer recurs, follow-up treatment depends on what treatment you have already had, the extent of your cancer, the site of recurrence, other illnesses, your age, and other aspects of your medical situation.
One possible treatment might include hormone therapy. Researchers are working on new drugs to block the effects of male hormones, which can cause prostate cancer to grow, and drugs to prevent prostate cancer growth.
Radiation therapy, ultrasound, extreme cold, electrical current, or medicines may be used to relieve symptoms of bone pain. Chemotherapy or other treatments being medically researched are also options.
Now in clinical trials are several types of vaccines for boosting the body’s immune system against prostate cancer cells. Sipuleucel-T is the only vaccine available on the market for prostate cancer.
Show Sources
Recommended Reading: Is Sex Good For An Enlarged Prostate
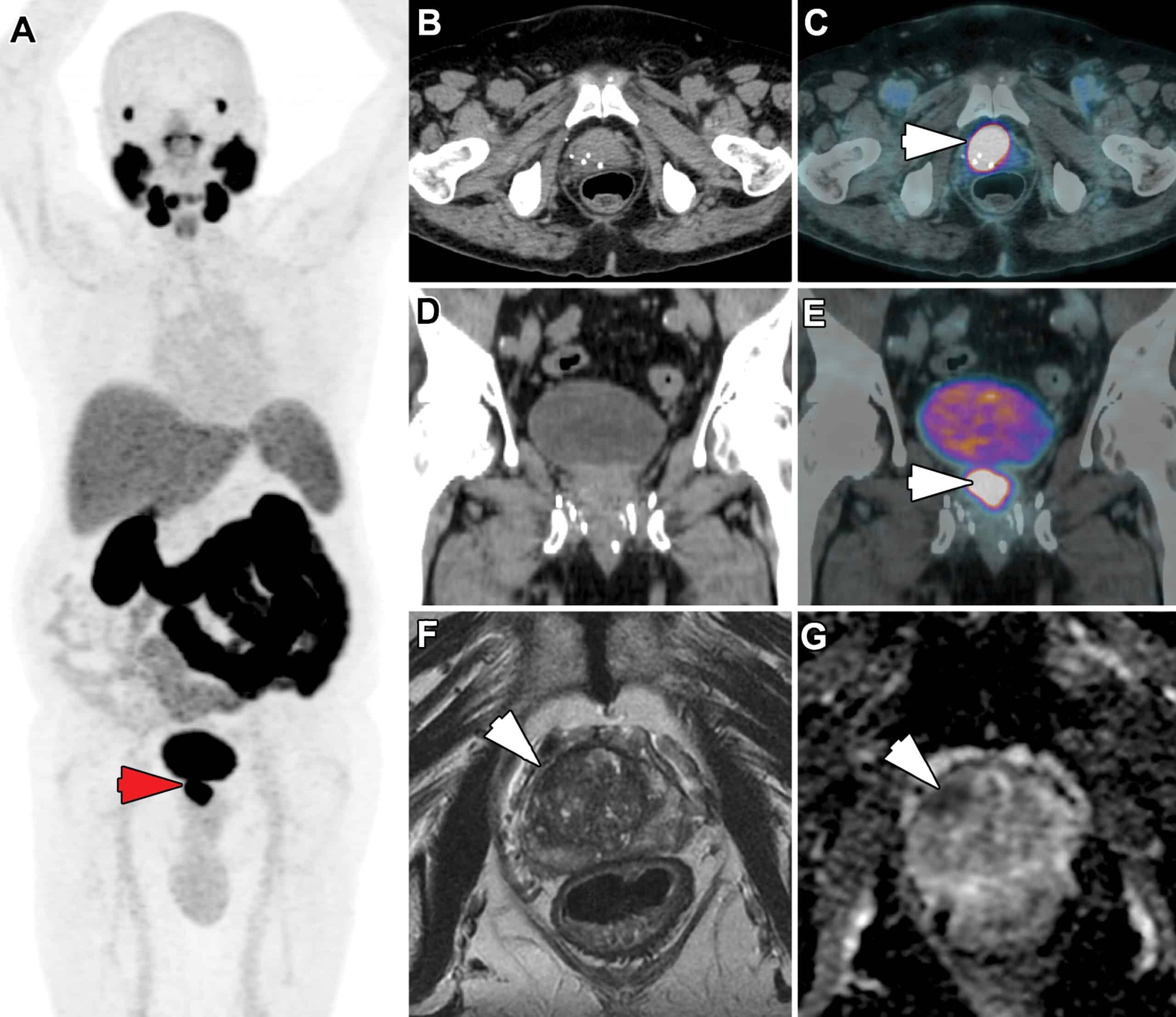
Targeting Local Recurrence After Surgery With Mri Imaging For Prostate Cancer In The Setting Of Salvage Radiation Therapy
- 1Academic Department of Radiology, Hôpital Pitié-Salpétrière, Assistance Publique des Hôpitaux de Paris, Paris, France
- 2Sorbonne University, Paris, France
- 3Nuclear Medicine Department, Tenon Hospital, Assistance Publique des Hôpitaux de Paris , Paris, France
- 4Department of Imaging, Clinique Pasteur, Toulouse, France
- 5Department of Oncology, Saint-Louis Hospital, Université de Paris, Assistance Publique des Hôpitaux de Paris, Paris, France
- 6Department of Radiotherapy, Clinique Pasteur, Toulouse, France
Magnetic resonance imaging is being increasingly used for imaging suspected recurrence in prostate cancer therapy. Functional MRI with diffusion and perfusion imaging has the potential to demonstrate local recurrence even at low PSA value. Detection of recurrence can modify the management of postprostatectomy biochemical recurrence. MRI scan acquired before salvage radiotherapy is useful for the localization of recurrent tumors and also in the delineation of the target volume. The objective of this review is to assess the role and potential impact of MRI in targeting local recurrence after surgery for prostate cancer in the setting of salvage radiation therapy.
Stage Iv Prostate Cancer Prognosis
Prostate cancers detected at the distant stage have an average five-year survival rate of 28 percent, which is much lower than local and regional cancers of the prostate. This average survival rate represents stage IV prostate cancers that have metastasized beyond nearby areas to lymph nodes, organs or bones in other parts of the body.
Don’t Miss: Does Prostate Milking Prevent Cancer
The Lancet Publishes Sylvester
Stay up to date with the latest medical news and research at UHealth.
Adding short-term hormone therapy and pelvic lymph node radiotherapy to standard of care prostatectomy surgical bed treatment benefits prostate cancer patients whose prostate-specific antigen levels are rising post prostatectomy, according to an international study led by Alan Pollack, M.D., Ph.D., chair and professor of radiation oncology at Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine, and published in The Lancet.
An increasing PSA after prostatectomy for prostate cancer is a hallmark of recurrence, which occurs on average in over 50% of patients with adverse surgical pathologic findings. The PSA indicates that the cancer has returned, but not where it is coming from the prostate surgical bed, the pelvic lymph nodes, or elsewhere in the body, according to Dr. Pollack.
Salvage radiotherapy is the only curative option for such patients, and the standard of care has been to treat the prostate surgical bed only. PSA recurrence after salvage radiotherapy has on average been over 50% over the subsequent five to 10 years. The SPPORT trial was designed to test whether treatment intensification with the addition of short-term hormone therapy or short-term hormone therapy plus pelvic lymph node radiotherapy significantly reduces recurrence and the risk of cancer spread.
Incremental Benefits
New Standard of Care
How Common Is Recurrence
The recurrence of prostate cancer depends on when it was caught and treated the first time. If your doctor was able to remove the cancer while it was still confined in the prostate gland, your chances of recurrence are fairly low. If your cancer spread before treatment, such as in the case of about 10% of men, recurrence is more likely to occur. Recurrence, therefore, occurs if not all of the cancer cells were treated the first time or if the cancer was more advanced than originally believed.
You May Like: Can Psa Rise After Prostate Removal
Statistical Methods To Build Biochemical Recurrence Prediction Models
Available preoperative parameters for multivariate analysis were age, clinical TNM stage, Gleason score from biopsy specimen , PSA and acid phosphatase level. Available postoperative variables were organ confinement, focal extraprostatic extension, extensive extraprostatic extension, lymph node involvement, seminal vesicle invasion, surgical margin status and Gleason score from surgical specimen.
Actuarial analysis was performed comparing freedom from biochemical recurrence after radical retropubic prostatectomy . Patients were censored if they were lost to followup or there was no recurrence. Event time distributions for the time to recurrence end point were estimated with the Kaplan-Meier method and compared using the log rank statistic or the proportional hazards regression model. The simultaneous effect of two or more factors was studied using the multivariate proportional hazards model. Covariates and interactions marginally significant in univariate analyses were entered into the multivariate regression model and insignificant effects were removed in a stepwise fashion. The first model was developed using preoperative variables only and the second model using all available variables.
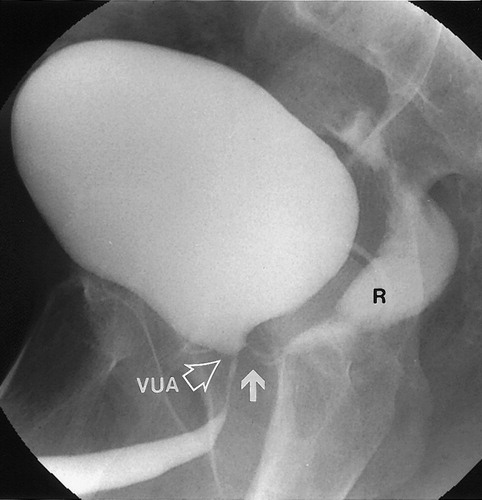
Normal Pelvic Anatomy After Radical Prostatectomy
RP includes total removal of the prostate and seminal vesicles, along with pelvic lymph node dissection. Postradical prostatectomy MRI findings include descent of the bladder which is anastomosed to extra prostatic distal urethra. The vesico-urethral-anastomosis should be visualized as a ring of postoperative fibrosis with low signal intensity on all sequences . Seminal vesicle which are supposed to be removed, may be retained in part with postoperative findings highly variable: 20% of the patients had SV remnants, with similar location of the preoperative SV position, with an additional 38% with fibrotic SV tips .
Figure 1 Postsurgical imaging findings after radical prostatectomy on sagittal and axial T2-weighted imaging: bladder neck descended into the prostatectomy fossa with a more conical shape the VUA anastomosis visualized as a ring of postoperative fibrosis on low signal intensity inferior to the bladder neck. Seminal vesicles which are supposed to be removed in a classical RP demonstrate a low signal intensity , but may be retained in part and can be seen in their presurgical locations with their characteristic tubular structure on T2W .
Don’t Miss: How Long After A Prostate Biopsy
What Treatment Options Are Best For Recurrent Prostate Cancer
The most suitable treatment for prostate cancer, if it becomes an issue once again after a prostatectomy, will vary on a patient-by-patient basis. These differences are usually contingent on a combination of factors, including the increased risk markers , the area of the body where recurrence manifests, the age of the patient, personal medical history, and more.
In many cases, hormone treatment may be recommended and carried out. This option for addressing recurrent prostate cancer works by blocking the cellular and physiological effects of certain male hormones. This kind of mitigation may further be supplemented with specialized drugs that play a significant role in preventing metastatic processes and curbing the cancers rate of growth.
Other options that can effectively eradicate or adequately address prostate cancer recurrence include high-intensity focused ultrasound , radiation therapies, and certain drug-based or chemotherapeutic approaches.
How Prostate Cancer Recurrence Is Detected
Following surgery for prostate cancer removal, the majority of patients will have regular appointments to check in and assess recovery progress with their healthcare provider or preferred oncologist. At each of these visits, your doctor will draw blood to run tests on various levels of biomarkers, hormones, and immunological markers, including PSA. You may also undergo minor physical assessments as part of your post-prostatectomy preventive maintenance care plan.
If prostate specific antigen levels are found to be rising, staying the same as pre-operative quantities, or slowing their rate of decrease in an unexpected way, your provider may suggest imaging tests or an X-ray of the prostate and pelvic area. A few other alternative options for detecting prostate cancer recurrence are available, although some are in the early stages of development or are not yet widely available, so should not be used as a default or go-to option for determining whether metastatic resurgence is a clear and present health risk.
Are you a practicing healthcare provider or oncologist who would like to learn more about alternative options for localized detection of recurrent prostate cancer?
Check out the full infographic here.
Dont Miss: How Can I Check My Own Prostate
You May Like: Does Erectile Dysfunction Mean Prostate Cancer
How Long Will Hormone Therapy Keep My Cancer In Check
Hormone therapy typically is effective for only a few years, but this period can range from several months to many decades. For many men who were using an antiandrogen in combination with an LHRH agonist or antagonist, stopping the antiandrogen, or antiandrogen withdrawal, is the most common first step in secondary hormone therapy. Between 10%30% of men will respond to anti-androgen withdrawal, which lasts on average 3 to 5 months. However, inevitably, additional therapies will need to be added even if this withdrawal response occurs. Continuing the LHRH agonist or antagonist and adding a new therapy in combination can improve survival and maintain or improve quality of life.
