Prostate Cancer Risk Higher Among Men With Ibd
Men with inflammatory bowel disease , especially ulcerative colitis, have an increased risk of prostate cancer , according to new study findings published in Prostate Cancer and Prostatic Diseases.
In a meta-analysis of 6 cohort studies including 86,137 IBD patientsfrom Europe and Asia, the presence of IBD was significantly associated with a33% increased risk for PCa over 4 to 40 years of follow-up. A subgroup analysisshowed that men with ulcerative colitis had a significant 58% higher riskfor PCa, whereas men with Crohns disease had a 12% higher risk. In addition,in 3 case-control studies that included 22,760 IBD cases and 300,851 IBD-freecontrols from the United States and the United Kingdom, men with IBD had an 81%higher risk for PCa.
Our findings based on the large and multicenter samples strongly indicated that men with IBD especial UC have significant elevated PCa risk, Yuqiu Ge, of the Wuxi School of Medicine, Jiangnan University, Wuxi, in Jiangsu, China, and colleagues concluded. If confirmed in larger studies, future efforts should focus on understanding the basis for the link between IBD and total PCa or clinically significant PCa risk, including the possibility that IBD leads to an altered microbiome that increases PCa risk.
The investigators said their findings suggest that increased PCascreening may be warranted for men with IBD.
How To Reduce Your Risk
Here are a few other things you can do to lower your chances of developing colorectal cancer and improve your odds of finding it early if you develop it:
- Ask your doctor about taking medications such as sulfasalazine , vedolizumab , or mesalamine . These drugs help manage UC, and they may help lower your risk for colorectal cancer.
- Take your medications as your doctor prescribed to keep your UC inflammation well managed.
- See your gastroenterologist for check-ups at least once a year.
- Let your doctor know if any of your family members had colorectal cancer or have recently been diagnosed.
- Eat more fruits, vegetables, and whole grains such as brown rice or wheat bread.
- Limit red meat, such as burgers, steaks, and pork. Also limit processed meats, such as hot dogs, bacon, and sausage. Theyve been linked to colorectal cancer risk.
- Avoid alcohol or limit yourself to no more than one drink a day.
- Try to walk, ride a bike, or do other exercises on most days of the week.
Along with getting regular screenings, look for these symptoms of colorectal cancer and report them to your doctor right away:
- a change in your bowel movements
- blood in your stool
Does Ulcerative Colitis Affect Your Cancer Risk
Having ulcerative colitis doesnt mean you will get colorectal cancer, but it does increase your risk.
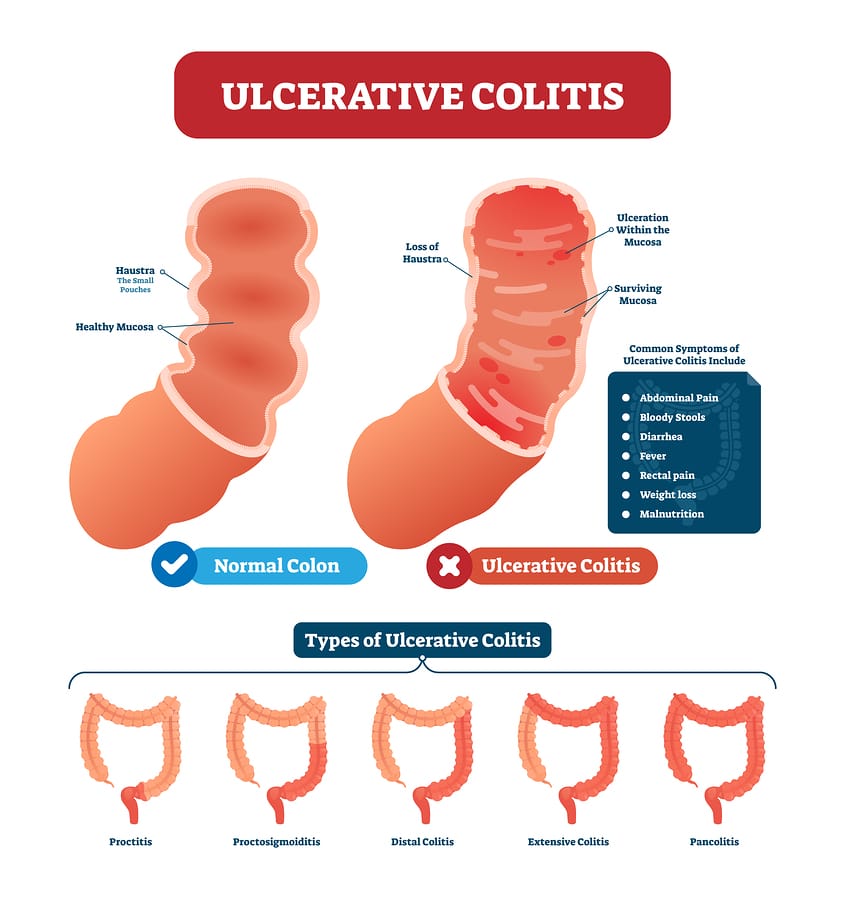
Ulcerative colitis is a chronic inflammatory bowel disease that affects the lining of the rectum and colon. It can be limited to the rectum or extend throughout the colon. Ulcerative colitis that affects the entire colon is called pancolitis.
The most common symptoms of ulcerative colitis are diarrhea and blood in your stool. Some patients may have abdominal pain. In severe cases, it can cause fever. Experts arent sure what causes the disease.
We talked to Yinghong Wang, M.D., about the link between ulcerative colitis, cancer and cancer treatment.
How does ulcerative colitis affect cancer risk?
If you have ulcerative colitis, your immune system recognizes the lining of your colon as a foreign body and attacks it. Over time, this damages the colon. As your body tries to repair the damage, the inflammation and constant cell replacement can result in a mutation that leads to cancer.
The more extensive your colitis and the longer you have it, the greater your risk of colorectal cancer. Males are at higher risk. And if you have both primary sclerosing cholangitis, which is inflammation of the bile duct, that puts you at even greater risk for colorectal cancer.
What should I do to reduce my cancer risk if I have ulcerative colitis?
Surgery is a cure. Because your colon is gone, the disease is gone, too.
What should cancer patients with ulcerative colitis know?
Don’t Miss: What Is Latest Treatment For Prostate Cancer
The Risk Of Colorectal Cancer In Crohns Disease And Ulcerative Colitis Patients
Patients with ulcerative colitis and Crohns disease involving the colon need to be especially vigilant about screenings for colorectal cancer. These patients are at higher risk for developing colorectal cancer than the general population.
Inflammation of the colon can cause continuous turnover of cells in the intestinal lining, which increases the chance of irregularities that may lead to cancer. Though the vast majority of patients with Crohns disease and ulcerative colitis will never develop colorectal cancer, it is important to discuss the risk with your doctor. Colorectal cancer is a highly treatable disease when its found early.
Duration Of Ulcerative Colitis
Your risk for colon cancer typically starts to increase once youve lived with UC for about 8 to 10 years, according to the Crohns & Colitis Foundation. The longer you have UC, the higher your cancer risk.
According to a 2019 literature review , colorectal cancer rates for people in North America increase dramatically after a person has lived with UC for 30 years.
Colorectal cancer rates in Asia increase dramatically after a UC duration of 10 to 20 years. Cancer rates for Asian people whove had UC for 10 to 20 years were four times higher than rates for Asian people whove had UC for 1 to 9 years.
Cancer rates for Europeans also increased as UC duration increased. However, the increase in cancer rates over time wasnt considered statistically significant. There wasnt enough data from Oceania to compare cancer rates over time.
This literature review had some noteworthy limitations. For instance, data wasnt included for people whod had colorectal polyps or a colectomy for UC.
Data for people with cancer outside of the colon or rectum, or those with a family history of colorectal cancer, was also excluded.
You May Like: Can Prostate Cancer Kill You
Symptoms Of Ulcerative Colitis
Some people with ulcerative colitis have only occasional symptoms. For others, the symptoms are constant. The symptoms a person experiences can vary depending on the severity of the inflammation and where it occurs in the large intestine.
Common symptoms include:
- diarrhea, often with blood and mucus
- cramping abdominal pain, especially in the lower abdomen
- a frequent sensation of needing to have a bowel movement
- little advance warning before a bowel movement
- the need to wake from sleep to have bowel movements
- low red blood cell count
Some people with ulcerative colitis develop pain or soreness in the joints, irritated eyes, and rashes.
The symptoms of ulcerative colitis can suddenly get worse. This is called a flare. Then symptoms may fade away. This is called remission. Some individuals with ulcerative colitis have symptoms only rarely, others have flares and remissions, others have symptoms all or most of the time.
Ulcerative Colitis And Colorectal Cancer
Ulcerative colitis increases the risk of colorectal cancer. Colorectal cancer often begins as small growths on the inside of the large intestine. The risk of colorectal cancer increases based on:
- the length of time a person has had ulcerative colitis
- how much of the colon is affected by ulcerative colitis
People with ulcerative colitis should have more frequent tests for polyps and colorectal cancer than people at average risk. The gold standard screening test is a colonoscopy. Polyps can be removed during a colonoscopy. This reduces the risk of colorectal cancer. Ask your doctor how often you should be checked for colorectal cancer.
Surgery to remove the entire colon eliminates the risk of colon cancer.
Recommended Reading: Prostate Cancer Questions And Answers
Inflammatory Bowel Disease And Prostate Cancer Risk Editorial
In the constant search for better approaches to treat and ultimately prevent prostate cancer, it is essential that we better understand the underlying etiology of prostate cancer. In times like this, I am often discouraged by the common mantra that the only known risk factors for prostate cancer are age, race, and family history. Surely, there must be other risk factors. Over time, certain risk factors have revealed themselves obesity , diet , and smoking to mention a few. One common factor, but certainly not the only factor, linking obesity, diet, and smoking is they all increase inflammation. If true that increased inflammation drives more prostate cancer, then it begs the question of whether other conditions that are clearly inflammatory-related are linked with prostate cancer. With this background in mind, Ge and colleagues tested the association between inflammatory bowel disease and prostate cancer risk.
Ibd And Prostate Cancer
Though controversial, doctors often use the prostate-specific antigen blood test to screen for prostate cancer. Normally, levels of PSA in the blood are low. If there is a significant increase, it can sometimes be a sign of prostate cancer.
However, men with IBD often have higher levels of PSA, possibly due to the chronic inflammation associated with the gastrointestinal condition.
Some researchers believe that certain inflammatory products, such as C-reactive protein, might boost levels of PSA without the presence of prostate cancer.
Because PSA levels can be high in people with IBD, they are often ignored. Understanding prostate cancer risk in this population is therefore important to help guide clinical decisions.
To investigate, the scientists followed 1,033 men with IBD and 9,306 men without IBD as a control group. On average, they followed each participant for 18 years. The average age at the beginning of the trial was 53.
They recently published their findings in the journal European Urology.
The scientists found that the prostate cancer risk for men with IBD was roughly five times greater than it was for those without the condition. The authors conclude:
ur study is the first to demonstrate an increased risk of clinically significant for men with IBD.
Read Also: What Happens When Prostate Cancer Spreads To The Lymph Nodes
Radiation For Prostate Cancer With Ulcerative Colitis
Has anyone with ulcerative colitis had pelvic radiation, specifically of the prostate bed after surgical prostatectomy? After 13 cancer-free years, doctors are concerned my prostate cancer is trying to return, with a PSA score of .33 after more than a decade of undetectable readings. Numerous scans of various types have not produced a single image of a cancerous mass. Radiation of the prostate bed would normally be a first line of attack, as the assumption is that’s where the cells are hiding. However, I also have ulcerative colitis, which is a non-issue for me health wise, but apparently radiation can produce life-changing inflammation of the colitis . Many radiation oncologists won’t even attempt prostate radiation with active colitis present, and those who will try are very clear about the risks. Any first-hand knowledge or recent studies would be helpful. Thanks.
Prostate Cancer And Radiation Colitis
Although technological advancements have made radiation therapy treatment more specific to the prostate, surrounding structures such as the bladder and rectum can still be affected.1 Close to 70% of all cancers are treated with radiation depending on the location of the involved organ, radiation colitis can be a common complication outside of prostate cancer.2 Yet up to 20% of patients with prostate cancer treated with RT will develop radiation colitis.3
Radiation colitis can present in 2 ways: acute and chronic .1-4 Patients with acute and chronic radiation colitis have similar symptoms, although chronic can cause more gastrointestinal bleeding. A patients bowel movements will contain more mucus and will be less formed they may experience diarrhea as well as urgency. Tenesmus is another common symptom.
Chronic inflammation of the rectum over many years can lead to stricturing of the left side of the colon, which may present with changes in stool caliber or constipation.
Also Check: How Hereditary Is Prostate Cancer
Does An Inflammatory Bowel Disease Flare Impact The Results Of The Prostate Specific Anitigen Test Used To Screen For Prostate Cancer
Co-Principal Researcher: Adam B. Weiner, MD |
Principal Investigator: Shilajit D. Kundu, MD
One million-plus Americans have IBD, accounting for more than two million ambulatory and emergency room visits annually. This health care utilization can lead to annual medical expenditures ranging from $5,000 to $8,000 per patient. Reducing unnecessary medical costs in this patient group is paramount. Take for example, PSA tests. While PSA screening can reduce prostate cancer deaths, false-positive elevations commonly occur, especially for patients with IBD. The Kundu research group recently found that men 65 and older with IBD, who underwent prostate cancer screening at Northwestern Memorial Hospital, had higher PSA values than non-IBD controls. In addition, men with IBD had a significantly higher risk of prostate cancer. However, whether the elevation in PSA is due to IBD-related inflammation versus a true reflection of an increased risk of prostate cancer remains unclear. Study findings may optimize how men with IBD are screened for prostate cancer by better assessing their risk while at the same time reducing needless medical expenses.
Researcher Bio
To receive Digestive Health Foundation updates on research, free education events, and the 2019 Gala, please fill in your information and click ‘Submit.’
Thank you, and welcome!
Save Article To Kindle

To save this article to your Kindle, first ensure coreplatform@cambridge.org is added to your Approved Personal Document E-mail List under your Personal Document Settings on the Manage Your Content and Devices page of your Amazon account. Then enter the name part of your Kindle email address below.Find out more about saving to your Kindle.
Note you can select to save to either the @free.kindle.com or @kindle.com variations. @free.kindle.com emails are free but can only be saved to your device when it is connected to wi-fi. @kindle.com emails can be delivered even when you are not connected to wi-fi, but note that service fees apply.
Recommended Reading: Does Melatonin Affect The Prostate
Helping Men With Ulcerative Colitis And Erectile Dysfunction
A first step in helping men with ED and UC is for either their doctor or the patient themselves, to begin the discussion. Ideally, all gastroenterologists should ask their male UC patients if they are experiencing ED. But, if that is not happening, a man should tell their doctor about this problem in order to get help.
Regular follow-ups is also recommended keeping tabs on their sexual health and what suggestions or medications are working or not. This helps men be more open discussing ED with their doctor helping them feel heard and acknowledged about their health concern.
Erectile Dysfunction And Ulcerative Colitis
There are a variety of reasons why men with UC unfortunately are more likely to suffer from ED. Many of the symptoms of UC likely lead to men to have less sexual desire and increased sexual functioning. When in an active phase, symptoms can include diarrhea, abdominal pain, rectal bleeding, urgent need to move bowels, and a sensation of incomplete evacuation of bowel movements.
Autoimmune diseases such as UC can also carry a psychological toll on mens mental health. A 2017 meta-analysis found that men with UC experiencing depression along with anxiety, stress, and poor social and emotional functioning, were all predictors of sexual problems that followed. Even if these men took antidepressants to deal with issues, antidepressant medication in and of itself, can lead to reduced sexual functioning as well.
Read Also: Does Radiation Treatment For Prostate Cancer Cause Erectile Dysfunction
Patient And Tumor Characteristics
In this single institutional retrospective review, we identified 4,245 patients who were treated with definitive SBRT for localized prostate cancer from 2012 to 2020. Of this cohort, 31 patients were found to have an underlying diagnosis of IBD prior to undergoing SBRT. The majority of patients in the IBD cohort were between the ages of 60 and 70 years, and there was no significant difference in the age distribution between the IBD and non-IBD patients when analyzed as a continuous variable. The majority of IBD patients had an excellent documented ECOG performance status of 1 . Androgen deprivation therapy was utilized as a component of treatment in the minority of patients , and was not significantly different relative to the non-IBD cohort.
Within the IBD cohort, the prostate cancer risk grouping was as follows: low , intermediate , and high . Pre-treatment PSA was< 10 ng/mL in the majority of patients . There were no patients found to have locally advanced disease and nearly half were diagnosed with pathologic grade group 2 cancer . There was no statistically significant difference identified between the IBD and non-IBD cohorts from a PSA , clinical stage , pathological grade group , or overall risk group standpoint . Patient and tumor characteristics are listed in Table .
Table 1 Patient tumor and characteristics
Ulcerative Colitis Linked To Increased Risk Of Prostate Cancer
According to a story from WebMD, a recent study revealed that men with Crohns disease, ulcerative colitis, or other forms of inflammatory bowel disease are at an increased risk of developing prostate cancer. Ulcerative colitis is considered rare, but Crohns disease is not. Around a million males in the US have inflammatory bowel disease .
Read Also: How To Clean The Prostate
How A Colonoscopy Works
In a colonoscopy, a doctor uses a long, flexible tube with a camera at the end to see inside your colon. The test helps them detect polyps in your colon lining. The doctor can remove these growths to prevent them from turning into cancer.
Your doctor might also remove tissue samples during your colonoscopy and have them tested for cancer. This procedure is called a biopsy.
Characterization Of Inflammatory Bowel Disease
We considered several treatment-related implications of bowel inflammation among prostate cancer patients. First, even in otherwise healthy patients radiation can induce bowel inflammation. This effect becomes particularly worrisome when considered in a background of prior and possibly ongoing inflammation. Second, inflammation may make surgery more difficult as it obliterates natural planes and degrades tissue. Further, patients on immunosuppressive medications may be at elevated risk of postsurgical problems involving infection or wound healing. Last, while chronic immunosuppression is an important and often necessary part of the management of moderate to severe IBD, this carries the risk of increasing rates of extra-intestinal malignancy and possibly cancer recurrence.10
Read Also: How Does The Prostate Work
