Patient And Treatment Characteristics
One hundred and forty-two consecutive patients were analyzed with pretreatment and treatment factors described in Table 1. NCCN risk groups are depicted in Table 1 with either three or five strata . Androgen deprivation therapy in the form of luteinizing hormone-releasing hormone agonist was used in 28.2% of patients . The use of ADT was dependent on individual urologist and radiation oncologist preference. Selected very low and low risk patients received ADT to shrink the prostate before SBRT.
Table 1. Patient and tumor characteristics.
Patients who received 35 or 36.25 Gy were termed the low-dose group and those who received 37.5 Gy the high-dose group. Most patients received their treatment over 58 days. The remainder completed treatment between 9 and 19 days with one non-compliant patient receiving his final fraction several weeks later, all due to poor adherence to their schedule. Treatment was delivered with an average of 187 non-coplanar beams. X-ray images were taken every three to five beams to track the prostates movement.
Favorable Vs Unfavorable Intermediate
The DAmico risk groups, initially published in 1998, were designed to stratify patients according to the likelihood of biochemical recurrencefree survival after radical prostatectomy or radiotherapy. The current NCCN guidelines are a slight modification of this classification system. However, in 2005 an International Society of Urological Pathology conference was held in order to reach a consensus regarding the grading of prostate cancer. A consensus statement was published in 2005, and as a result of the adoption of this new grading system, the reporting of secondary pattern Gleason grade 4 disease became more prevalent. Several investigators have reported on their observation of grade migration from GS 3+3 to GS 3+4 . This grade migration could cause a number of men who previously would have been categorized as low-risk to be assigned to the NCCN intermediate-risk category because of their GS, thereby improving the prognosis of both groups . Thus, it has been hypothesized that some men with GS 3+4 intermediate-risk prostate cancer may have a low risk of PCSM and higher rates of overall survival , similar to what is seen in patients with low-risk prostate cancer.
Only one intermediate-risk factor .
GS of 3+4=7 or less.
Less than 50% of biopsy cores positive for cancer.
Those who were classified as unfavorable could have any of the following:
More than one intermediate-risk factor.
GS of 4+3=7.
Greater than 50% positive biopsy cores.
I Have Heard That Other Factors May Be Included When Evaluating Treatment
Yes, other factors such as the number of biopsies and the presence of Gleason Score 7 versus a Gleason Score may influence the treatment decision. The number of + biopsies is also strongly predictive of outcomes but not typically part of the risk grouping systems. An example would be a person with a multiple + biopsies Gleason 7. His cancer would be considered a High Intermediate Risk and require a combination of External Beam and radiation while another patient with only a few + biopsies could be a Low Intermediate Risk patient and be a good candidate for an implant alone. These factors should be discussed with you doctor.
©2013 Prostate Cancer Center of Seattle | All Rights Reserved | P 1.877.330.7722 OR 206.453.2992 |
Recommended Reading: Is Green Tea Good For Prostate
Variation In National Use Of Long
Background: The current NCCN Clinical Practice Guidelines in Oncology for Prostate Cancer recommend long-term androgen deprivation therapy for all men with high-risk prostate cancer treated with external-beam radiation therapy . We determined whether the use of long-term ADT varied by the recently defined subcategories of high-risk disease versus unfavorable intermediate-risk disease. Methods: We identified 5,524 patients with unfavorable-risk prostate cancer diagnosed from 2004 to 2007 and managed with EBRT using the SEER-Medicare linked database. Patients were stratified by risk group: unfavorable intermediate-risk, favorable high-risk , very-high-risk , or other high risk . We used multivariable competing risks regression to estimate the rates of long-term ADT by group. Results: Men with favorable high-risk prostate cancer were significantly less likely to receive long-term ADT than those with other high-risk disease , and similarly likely as those with unfavorable intermediate-risk disease . Other high-risk disease was less likely to receive long-term ADT than very high-risk cancer . Despite current guidelines, patients with EBRT-managed high-risk prostate cancer received significantly different rates of long-course ADT based on subclassification. Our results suggest that oncologists view these patients as a heterogeneous group with favorable high-risk cancer warranting less aggressive therapy than other high-risk or very high-risk disease.
Treatment Protocol At Each Institution
Some patients receiving SEED-BT at institution A in 2006 were treated using preplanning methods. Most other patients at the 3 institutions were treated using an intraoperative planning method with modified peripheral loading techniques using a Mick applicator,. The therapeutic planning and post-implant dosimetric evaluation were performed using the Interplant planning system or Variseed . 125I was used for all patients. Either Oncoseed 6711 or STM 1251 was used for SEED-BT. The doses were defined using the TG-43 criteria. At 1 month after treatment with SEED-BT alone, a computed tomography-based dosimetric analysis was performed to calculate the D90, V100, and V150 results. Prostate D90 is the minimum dose to 90% of the prostate gland at 1 month. Prostate V100 and V150 are the percentages of the prostate gland volume respectively receiving 100% and 150% of the prescribed dose at 1 month. These treatment protocols were used at each institution:
Institution A
Institution B
Institution C
All patients classed as intermediate-risk were candidates for treatment with SEED-BT alone. Patients receiving SEED-BT alone were treated at a prescribed dose of 145 Gy. Non patients were treated with a combination of SEED-BT and EBRT. The CTV for SEED-BT included the entire prostate. No PTV was created in SEED-BT.
Don’t Miss: What Is Prostate Gland Hypertrophy
Treatment Of Unfavorable Intermediate Risk Prostate Cancer
Biographies:Related Content:Read the Full Video Transcript
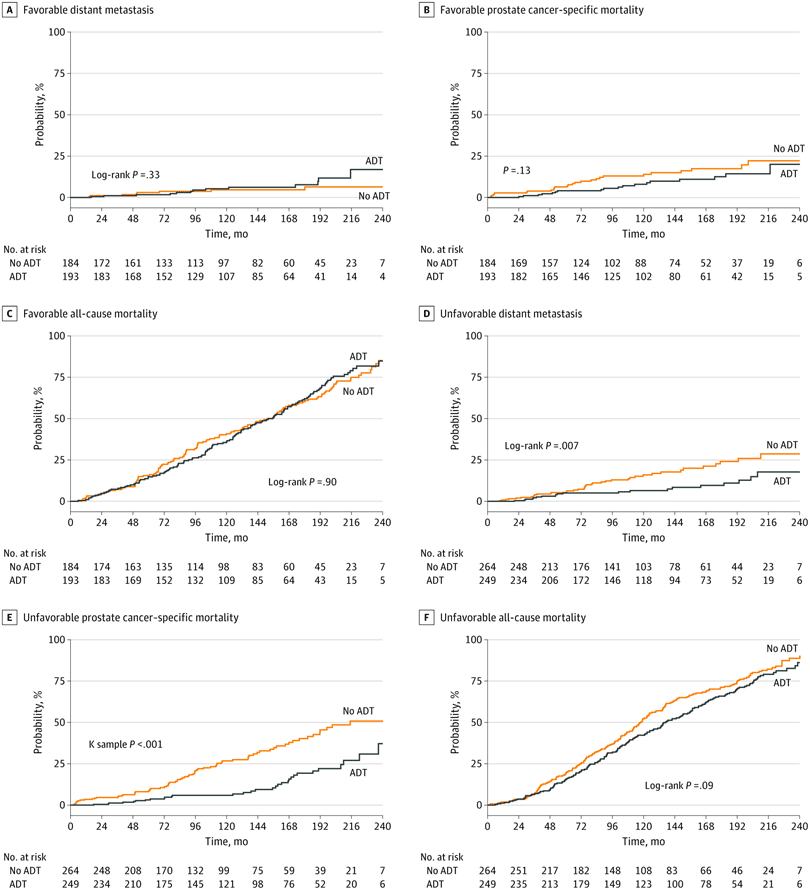
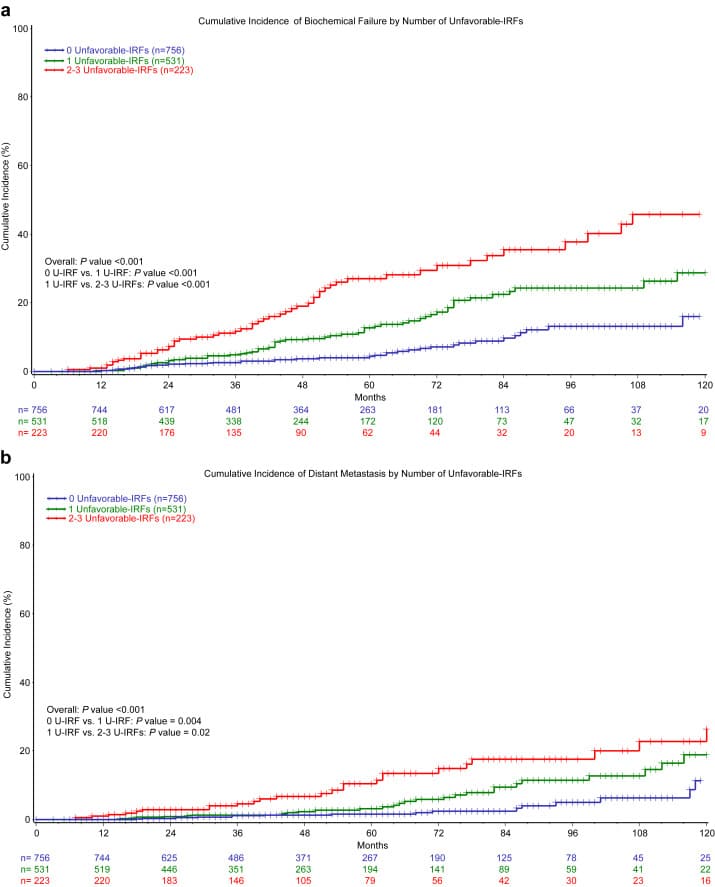
Ashley Ross: Hi, I’m Ashley Ross speaking for UroToday. I’m a urologist at Northwestern at the AUA 2022. This year. We had some interesting discussions around the use of decipher in unfavorable, intermediate risk, prostate cancer. Genomics has played a larger role in our practices as urologists. Particularly at initial diagnosis. For a while, we were using its prognostic ability to help guide us on decisions regarding active surveillance or active treatment for men with localized prostate cancer, mostly in the low and favorable intermediate risk space. They published some retrospective, an analysis of prospective randomized data in the RTOG 0126 trial. And this was with intermediate risk patients getting radiation for their prostate cancer. Many of which were unfavorable, intermediate risk patients. And they showed that you could use a genomic classifier to stratify those patients into low risk or into high risk categories. And by that stratification determine whether or not they would have benefit from adding androgen deprivation therapy to their treatment. In those studies men without androgen deprivation therapy, who were genomic high risk had metastasis rates of about 20%.
Katie Murray: Thank you.
> > > 1 Bedtime Hack To Pee Like A Bull
An enlarged prostate can also be the cause of other problems. If the enlarged prostate is causing symptoms, the best treatment would be a natural remedy. In the meantime, there are treatments for a wide range of conditions that cause a man to experience pain. A common surgical procedure involves an electric loop, laser, or electro-stimulation. The procedure is a safe and effective option for treating enlarged or symptomatic BPH.
Read Also: What Type Of Doctor Treats Prostate Issues
Focal Therapy For Prostate Cancer
With recent advances in MRI and targeted biopsy, we are better able to locate the exact area of prostate cancer. Men who do not have an enlarged prostate, who have prostate cancer that is detected only in a single region of the prostate and have intermediate grade cancer can be a candidate for focal therapy. This type of therapy treats only the cancerous tissue and spares the normal prostate, thereby preserving urinary and sexual function
Here at UCLA we commonly use cryotherapy or HIFU to focally treat prostate cancer. Given that this is a relatively new form of treatment, we have established rigorous post-treatment protocols using MRI and biopsies to ensure that the cancer has been adequately treated.
> > > This Simple Morning Test Will Fix Your Prostate
Another type of prostate issue is chronic prostatitis, or chronic pelvic pain syndrome. This condition causes pain in the lower back and groin area, and may cause urinary retention. Symptoms include leaking and discomfort. In severe cases, a catheter may be required to relieve the symptoms. If the problem is unresponsive to other treatments, your doctor may suggest a surgical procedure. If these do not work, your symptoms could progress and become chronic.
An acute bacterial infection can cause a burning sensation. Inflammation of the prostate can affect the bladder and result in discomfort and other symptoms. This is the most common urinary tract problem in men under 50, and the third most common in men over 65. The symptoms of acute bacterial prostatitis are similar to those of CPPS. Patients may experience a fever or chills as a result of the infection.
Also Check: Why Do People Get Prostate Cancer
Bisphosphonates And Prostate Cancer
In men with castration-recurrent prostate cancer and bone metastases, zoledronic acid every 3 to 4 weeks is recommended to prevent disease-related skeletal complications, including pathologic fractures, spinal cord compression, surgery, or RT to bone . Other bisphosphonates are not known to be effective for preventing disease-related skeletal complications.
In a pivotal multicenter study, 643 men with castration-recurrent prostate cancer and asymptomatic or minimally symptomatic bone metastases were assigned randomly to intravenous zoledronic acid or placebo.170 All men continued ADT throughout the study and received additional antineoplastic therapy at the discretion of the investigator. The primary study end point was the proportion of men who experienced one or more skeletal-related event by 15 months. Adverse renal events prompted 2 study amendments. In the first amendment, the infusion time for zoledronic acid was increased from 5 to 15 minutes. In the second amendment, the zoledronic dose in the 8-mg treatment group was reduced to 4 mg, serum creatinine monitoring was implemented before each dose, and the primary efficacy assessment became the comparison of the 4-mg group versus placebo.
Study Cohort And Treatment
The study cohort consisted of 136 consecutive men with unfavorable intermediate-risk PC who underwent open retropubic RP by a single urologic surgeon at an academic medical center for PC between 2005 and 2008. Men with unfavorable intermediate-risk PC included any intermediate-risk patient with a primary Gleason pattern of 4, percentage of positive biopsy cores > 50%, or multiple intermediate-risk factors . All diagnostic biopsy samples
Don’t Miss: Can You Have Erection After Prostate Cancer
Treatment For Intermediate Risk Prostate Cancer
Intermediate risk prostate cancers are the most frequently treated prostate cancers. They are cancers that are confined to the prostate, often are Gleason 7 and have a PSA of less than 20. These cancers are treated in men with life expectancy greater than 10 years to prevent spread of the cancer in the long-term. There are a number of different effective treatment options for intermediate risk prostate cancer and the decision is often a personal one. Here at UCLA we recommend consultation with both Urologist and Radiation Oncologist to help men decide which treatment option is best for them.
Comparison Of Distribution Of Patient Characteristics Stratified By Whether Patient Was Upgraded To Prostatectomy Gleason 8 Or Higher
Clinicopathologic characteristics of the 136 included patients are presented in Table 1. The median age was 60.5 years, and the median pretreatment PSA was 5.8 ng/mL. Most men had clinical T1c disease. All of men had Gleason score 7, with 49.3% of these demonstrating Gleason 4 + 3 on biopsy. The median GPC was 70%. We observed that men who had pathologic upgrading at the time of RP were significantly older and had higher median GPC
Also Check: Late Stage Prostate Cancer Symptoms
Considering Prostate Cancer Treatment Options
For most men diagnosed with prostate cancer, the cancer is found while its still at an early stage its small and has not spread beyond the prostate gland. These men often have several treatment options to consider.
Not every man with prostate cancer needs to be treated right away. If you have early-stage prostate cancer, there are many factors such as your age and general health, and the likelihood that the cancer will cause problems for you to consider before deciding what to do. You should also think about the possible side effects of treatment and how likely they are to bother you. Some men, for example, may want to avoid possible side effects such as incontinence or erection problems for as long as possible. Other men are less concerned about these side effects and more concerned about removing or destroying the cancer.
If youre older or have other serious health problems and your cancer is slow growing , you might find it helpful to think of prostate cancer as a chronic disease that will probably not lead to your death but may cause symptoms you want to avoid. You may think more about watchful waiting or active surveillance, and less about treatments that are likely to cause major side effects, such as radiation and surgery. Of course, age itself is not necessarily the best reason for your choice. Many men are in good mental and physical shape at age 70, while some younger men may not be as healthy.
Why Is Risk Level Important
Risk level is all about matching the right treatment to the right patient, so its very important!
The idea of classifying PCa according to risk was originally based on the relative risk of PSA failure after prostatectomy or radiation. Until the late 1990s, the only conceivable treatment options were either whole gland surgery or radiation, and watchful waiting . The standard risk classification was the DAmico system:
- Low risk defined as stage T1c, T2a and PSA level 10 ng/mL and Gleason score 6
- Intermediate risk defined as stage T2b or Gleason score of 7 or PSA level > 10 and 20 ng/mL
- High risk defined as stage T2c or PSA level > 20 ng/mL or Gleason score 8.
You May Like: Can Prostate Cancer Symptoms Come And Go
What You Need To Know About The Prostate Favorable Vs Unfavorable Intermediate Risk Prostate Cancer
A enlarged prostate can also cause blockages in the urethra. A blocked urethra can also damage the kidneys. A patient suffering from an enlargement of the prostate may have pain in his lower abdomen and genitals. If pain is present, a digital rectal examination will reveal hard areas. A doctor may prescribe surgery or perform an endoscopic procedure. If the enlarged prostate is not completely removed, it will shrink.
While the size of an enlarged prostate will influence the extent of urinary symptoms, men may experience a range of urinary symptoms. Some men have minimal or no symptoms at all. Some men will have a very enlarged prostate, whereas others will have a mild enlargement. Generally, the symptoms can stabilize over time. Some men may have an enlarged prostate but not notice it. If they have an enlarged colon, their physician can perform a TURP procedure.
Psa Response And Biochemical Control
The overall 5-year actuarial FFBF for the whole group was 92.7% . Six patients out of the entire cohort of 142 patients, all in the low dose group, experienced BF two were high risk, three intermediate risk, and one low risk. The low-dose and high-dose groups median PSA nadirs were 0.3 and 0.1 ng/mL, respectively. Five year actuarial FFBF was 100% for the high dose group and 93.75% for the low dose group, p= 0.05, hazard ratio of 11.0 for low compared to high dose .
Table 2. Freedom from biochemical failure stratified by risk and descriptive statistics.
Figure 2. Years of freedom from biochemical failure by dose for all patients.
Figure 3. Years of freedom from biochemical failure by Gleason score for all patients.
Multivariate analysis evaluated the most significant factors in univariate analysis including risk stratification groups, GS, and dose. GS and dose were the most predictive factors in multivariate analysis but did not reach statistical significance at the p< 0.05 level. Of note, with only six failures, we only have the power to detect a single significant predictor of failure in the multivariate analysis.
You May Like: Pros And Cons Of Having Prostate Removed
Matching Treatment For Favorable Risk Prostate Cancer
Today, the majority of PCa cases are diagnosed early thanks to PSA screening coupled with noninvasive multiparametric MRI tumor detection. It therefore makes sense that for those with Gleason 3+3 and some with Gleason 3+4, the conditions are favorable for a successful minimalist approach to managing the disease, including treatment and AS. These are considered favorable low-risk and favorable intermediate-risk prostate cancers. When carefully diagnosed and qualified, these patients may safely hold off on such aggressive radical treatments provided they protect themselves by adhering to monitoring protocols.
Radiation Therapy Oncology Group 94
This multi-institutional study was conducted to evaluate the effect of the addition of AST to RT on overall survival, freedom from biochemical failure, freedom from clinical progression, and disease-free survival in patients with localized prostate cancer in response to the positive effect on these parameters seen in RTOG 86-10. To this end, 1979 patients with T1bT2b prostate cancer and PSA less than 20 ng/ml were randomized to receive EBRT alone or in conjunction with 2 months of neoadjuvant and 2 months of concurrent goserelin and flutamide.
You May Like: What Does The Prostate Do In A Man
European Society Of Medical Oncology
The 2015 ESMO guidelines recommend watchful waiting with delayed hormone therapy as an option for localized disease or as an alternative for men with localized or locally advanced disease who are unwilling or unsuited for radical therapy.
Other recommended treatment options include :
-
Active surveillance for men with low-risk disease
-
Radical prostatectomy or radiotherapy for men with low- or intermediate-risk disease
-
Primary androgen deprivation therapy alone is not recommended for treatment of non-metastatic disease
-
For patients with high-risk or locally advanced prostate cancer, external beam RT plus hormone treatment or RP plus pelvic lymphadenectomy
Also Check: Preparation For Prostate Mri Scan
