The Above Policy Is Based On The Following References:
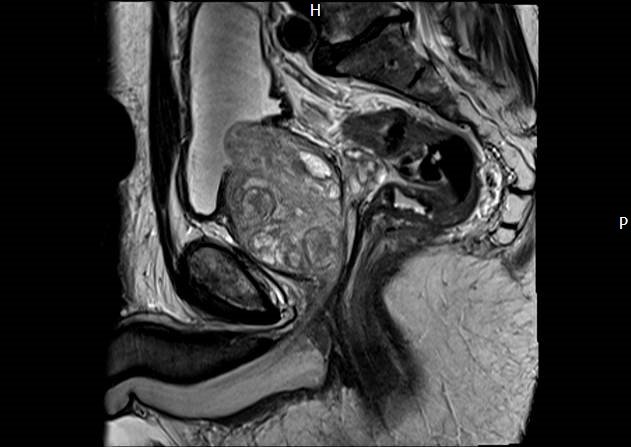
What Is An Mri Scan Of The Prostate
A magnetic resonance imaging scanner uses strong magnetic fields to create an image of the prostate and surrounding tissues.
The prostate gland is a small soft structure about the size and shape of a walnut, which lies deep in the pelvis between the bladder and the penis, and in front of the rectum .
Its function is to help liquefy semen .
What Are The Limitations Of Mri Of The Prostate
High-quality images depend on your ability to remain perfectly still and follow breath-holding instructions while the images are being recorded. If you are anxious, confused or in severe pain, you may find it difficult to lie still during imaging.
A person who is very large may not fit into certain types of MRI machines. There are weight limits on the scanners.
Implants and other metallic objects can make it difficult to obtain clear images. Patient movement can have the same effect.
A very irregular heartbeat may affect the quality of images. This is because some techniques time the imaging based on the electrical activity of the heart.
MRI cannot always distinguish between cancer and inflammation or the presence of blood products within the prostate. Blood may sometimes appear due to a prostate biopsy. To avoid confusing any bleeding with cancer, your doctor may wait six to eight weeks after prostate biopsy to perform prostate MRI. This will allow any remnants of bleeding to resolve.
MRI typically costs more and may take more time to perform than other imaging methods. Talk to your insurance provider if you have concerns about the cost of MRI.
Read Also: How To Massage A Man’s Prostate
What Are The Limitations Of Ultrasound
A biopsy can only show if there is cancer in the samples taken, so it is possible that cancer in unsampled areas of the prostate might be missed.
For MRI-guided biopsies, high-quality images are assured only if you are able to remain perfectly still while the images are being recorded. If you are anxious, confused or in severe pain, you may find it difficult to lie still during imaging, and the resulting images may not be of sufficient quality to be useful as a diagnostic tool.
Likewise, the presence of an implant or other metallic object sometimes makes it difficult to obtain clear MR images. A person who is very large may not fit into the opening of certain types of MRI machines.
MR imaging cannot always distinguish between cancer tissue and inflammation or the presence of blood products within the prostate, which sometimes occurs related to a prostate biopsy. To avoid confusing the two on imaging, prostate MR imaging may be performed six to eight weeks after prostate biopsy, if possible, to allow any residual bleeding to resolve itself.
MRI typically costs more and may take more time to perform than other imaging methods. Talk to your insurance provider if you have concerns about the cost of MRI.
What Will I Experience During And After The Procedure
Most MRI exams are painless. However, some patients find it uncomfortable to remain still. Others may feel closed-in while in the MRI scanner. The scanner can be noisy. Sedation may be arranged for anxious patients, but fewer than one in 20 require it.
You may feel pressure while the doctor inserts the endorectal coil into your rectum. This is similar to that experienced during a digital rectal exam.
It is normal for the area of your body being imaged to feel slightly warm, but if it bothers you, notify the radiologist or technologist. It is important that you remain perfectly still while the images are being recorded, which is typically only a few seconds to a few minutes at a time. For some types of exams, you may be asked to hold your breath. You will know when images are being recorded because you will hear tapping or thumping sounds when the coils that generate the radiofrequency pulses are activated. You will be able to relax between imaging sequences, but will be asked to maintain your position as much as possible.
You will usually be alone in the exam room during the MRI procedure. However, the technologist will be able to see, hear and speak with you at all times using a two-way intercom. Many MRI centers allow a friend or parent to stay in the room as long as they are also screened for safety in the magnetic environment.
You May Like: Does Enlarged Prostate Cause Constipation
What Will I Experience During And After The Biopsy
If you receive IV contrast for the MRI-guided procedure, you may feel coolness and a flushing sensation for a minute or two when the contrast material is injected. The intravenous needle may cause you some discomfort when it is inserted and you may experience some bruising once it is removed.
Rarely, patients may experience side effects from the MR contrast material, including nausea and local pain, hives, itchy eyes or other reactions. If you experience allergic symptoms, a radiologist or other physician will be available for immediate assistance.
When the ultrasound probe or endorectal coil is inserted into the rectum, you will feel pressure and may have some temporary discomfort.
You will hear a clicking noise when the biopsy needle samples the prostate, and you may feel a stinging or burning sensation in the area.
Some patients find it uncomfortable to remain still during MR imaging. Others experience a sense of being closed-in . Therefore, sedation can be arranged for those patients who anticipate anxiety.
If you feel heating on your skin at any time during MR imaging, the MR technician should be notified so that they can perform a closer examination of the area.
Some patients experience a small amount of bleeding from the rectum or perineum immediately after the biopsy procedure. If this occurs, it will cease with gentle pressure.
You may feel pain and discomfort in the area of the prostate for a day or two after the biopsy, particularly when you are seated.
Who Interprets The Results And How Do I Get Them
A radiologist, a doctor trained to supervise and interpret radiology exams, will analyze the images. The radiologist will send a signed report to your primary care or referring physician, who will share the results with you.
Follow-up exams may be needed. If so, your doctor will explain why. Sometimes a follow-up exam is done because a potential abnormality needs further evaluation with additional views or a special imaging technique. A follow-up exam may also be done to see if there has been any change in an abnormality over time. Follow-up exams are sometimes the best way to see if treatment is working or if an abnormality is stable or has changed.
Recommended Reading: Does Cialis Shrink An Enlarged Prostate
What Are The Risks Of A Prostate Mri
A very small number of people have an allergic reaction to the gadolinium contrast medium. Most reactions are mild, such as a rash or hives .
If you have very poor kidney function, you will not be given contrast medium, as there is a small risk of nephrogenic systemic fibrosis see Contrast Medium: using gadolinium or iodine in patients with kidney problems.
If an endorectal coil is used for the scan, there is also a very small risk of damage to the rectum from the balloon. If you have any concerns, please contact the MRI facility.
What Makes Your Prostate At Risk
The prostate is a small, exclusively male gland. It lies under the bladder and has the particularity surrounding the urethra, a small channel that brings urine from the bladder to the tip of the penis. This localization describes why any prostate problem can cause urinary conditions . Mri Prostate Cpt Code
Don’t Miss: Prostate Cancer Ruined My Marriage
Approved By Governing Bodies:
Magnetic resonance imaging guided or MRI/ultrasound fusion biopsy is a medical procedure that uses MRI and ultrasound devices previously approved by the U.S. Food and Drug Administration . Prostate biopsy is a surgical procedure and, as such, it is not subject to regulation by FDA.
FDA product code, ultrasound devices: IYN, ITX, IYO. FDA product code, MRI devices: LNH, LNI, MOS.
Several MRI-US fusion software-based targeted prostate biopsy platform specifications have been cleared from marketing by FDA through the 510 marketing process. Fusion software and include: Artemis , BioJet , BiopSee® , Real-time Visual Sonography , UroNav , Urostation® , and Virtual Navigator .
What Does The Equipment Look Like
The traditional MRI unit is a large cylinder-shaped tube surrounded by a circular magnet. You will lie on a table that slides into the center of the magnet.
Some MRI units, called short-bore systems, are designed so that the magnet does not completely surround you. Some newer MRI machines have a larger diameter bore, which can be more comfortable for larger patients or those with claustrophobia. “Open” MRI units are open on the sides. They are especially helpful for examining larger patients or those with claustrophobia. Open MRI units can provide high quality images for many types of exams. Certain exams cannot be performed using open MRI. For more information, consult your radiologist.
Most prostate MRI exams use high-field MRI magnets because they provide higher-quality images. However, men with metal implants may undergo low-field prostate MRI because the implants may otherwise interfere with imaging.
Read Also: What Happens If Prostate Cancer Goes Untreated
How Is The Procedure Performed
MRI exams may be done on an outpatient basis.
You will be positioned on the moveable exam table. Straps and bolsters may be used to help you stay still and maintain your position.
Devices that contain coils capable of sending and receiving radio waves may be placed around or next to the area of the body being scanned.
MRI exams generally include multiple runs , some of which may last several minutes.
Your exam may use an endorectal coil. If so, a nurse or doctor will place a disposable cover over the coil. They will lubricate the assembly and insert the coil a short distance into your rectum. After insertion, the doctor inflates the circular balloon that sits around the coil and holds it in place during the exam. When the exam is complete, the doctor deflates the balloon and removes the coil.
If a contrast material is used, a doctor, nurse or technologist;will insert an intravenous;catheter into a vein in your hand or arm that will be used to inject the contrast material.
You will be placed into the magnet of the MRI unit. The technologist will perform the exam while working at a computer outside of the room.
If a contrast material is used during the exam, it will be injected into the intravenous line after an initial series of scans. More images will be taken during or following the injection.
When the exam is complete, you may be asked to wait while the radiologist checks the images in case more are needed.
Your IV line will be removed after the exam is over.
Know Error Dna Specimen Provenance Assay
DNA Specimen Provenance Assignment Testing is a molecular diagnostic test intended for the protection and control of tissue samples to purportedly decrease the incidence of diagnostic mistakes due to an individuals misidentification, specimen transposition or cell contamination, known as specimen provenance complications . Breast and prostate tissues are most often tested but other tissue types may also be examined including, but not limited to, bone marrow.
You May Like: What Happens To The Prostate Later In Life
Radiology Question For The Week Of September 17 2018
Question:
We perform treatment-simulation planning in our magnetic resonance imaging for brain and prostate radiation procedures. The radiologist does not interpret these exams; they are performed just to send the images to other systems for their use. Is there an appropriate charge code for this type of imaging? In the past we have used 76498 but our charge-master coordinator does not think that is appropriate. Any guidance you can give is appreciated.
Answer:
Code 76498unlisted magnetic resonance procedure in Clinical Examples in Radiology.
However, if the images are obtained for simulation, then they are included in the simulation codes . The CPT® book includes the following information:
Simulation is the process of defining relevant normal and abnormal target anatomy, and acquiring the images and data necessary to develop the optimal radiation treatment process for the patient.
CPT® is a registered trademark of the American Medical Association.
This question was answered in an edition of our;Radiology Compliance Manager. For more hot topics relating to radiology services, please view our store, or call us at 1.800.252.1578 ext. 2.
Disclaimer: Every reasonable effort was made to ensure the accuracy of this information at the time it was published. However, due to the nature of industry changes over time we cannot guarantee its validity after the year it was published.
Prostate Mri With And Without Contrast
gary37907
Has anyone here had experience with the a Prostate MRI with and without contrast for prostate cancer screening? My internist suggested that I have this rather than biopsy due to possible side effects of needle biopsy. He said that MRI has become pretty accurate in detecting tumors and when it is positive for tumors it can be used as a guide for directing needle biopsy. Mine showed no masses but BPH with medial lobe involvement intruding into the blaldder neck. This all came about because my BPH symptoms got so bad that I was retaining urine in my bladder. MY urologist wanted me to have a biopsy before any BPH surgical procedures because of a history of 3 brothers with prostate cancer. My last PSA was 2.9 but it has gotten up to the low 3’s on several occasions. I don’t know what my Uro will do with these results tho I would assume it would mean a go for any procedure I decide to have. Now the hard part is deciding which procedure to get. I am an otherwise healthy 67 year old. I would appreciate some input from those who have knowledge and or experience with the prostate MRI. Thanks Gary
0 likes, 14 replies
Read Also: Enlarged Prostate Sexuality
Description Of Procedure Or Service:
Before a transrectal ultrasound-guided biopsy, a magnetic resonance imaging scan can be used to pinpoint the location of suspicious lesions in the prostate. MRI permits a targeted biopsy . The use of an MRI-guided prostate biopsy serves two functions: to identify areas in the prostate that could harbor a high-grade tumor; and to divert attention from any clinically insignificant cancers not needing treatment. In accomplishing the secondary function, patients are placed into one of two categories: those only needing active surveillance; and those needing definitive intervention.
Prostate Cancer
Prostate cancer is the most commonly diagnosed cancer and the second leading cause of cancer deaths among men in the U.S., with an estimated 248,530 new cases and 34,130 deaths to occur in 2021.;
Diagnosis
Diagnosis and grading of prostate cancer are performed by taking a biopsy of the prostate gland. A prostate biopsy typically is performed in men who have an elevated prostate-specific antigen level or who present with symptoms. The purpose of the biopsy is to determine whether cancer is present and to determine the tumor grade. Tumor grade is a major determinate in whether a patient is eligible for active surveillance or definitive intervention . Patients in active surveillance undergo periodic follow-up prostate biopsies to assess cancer progression .
Multiparametric Magnetic Resonance Imaging
Table 1. Techniques for MRI-Guided Prostate Biopsy
Avoidance Through The Kitchen
Of course, the diet plan has an influence on prostate health. It is vital to adopt a healthy and balanced diet when you desire to avoid disorders that can impact it!Make room for vegetables and fruit, abundant in antioxidant minerals and vitamins, as their role on the prostate is proven.A routine intake of omega-3 fats has a protective function versus swelling, a procedure involved in benign hypertrophy or prostate cancer!On the other hand, particular foods increase the risk of establishing prostate problems and need to be consumed in small amounts:
- Foods consisting of hydrogenated fats of animal origin have been connected with an increased danger of establishing prostate cancer
- Easy, refined sugars, contained in commercial meals, sweets, sodas, are also involved in inflammatory processes and ought to therefore be avoided!
Read Also: Can Prostatitis Go Away On Its Own
