Gene Set Enrichment Analysis And Functional Enrichment Analysis
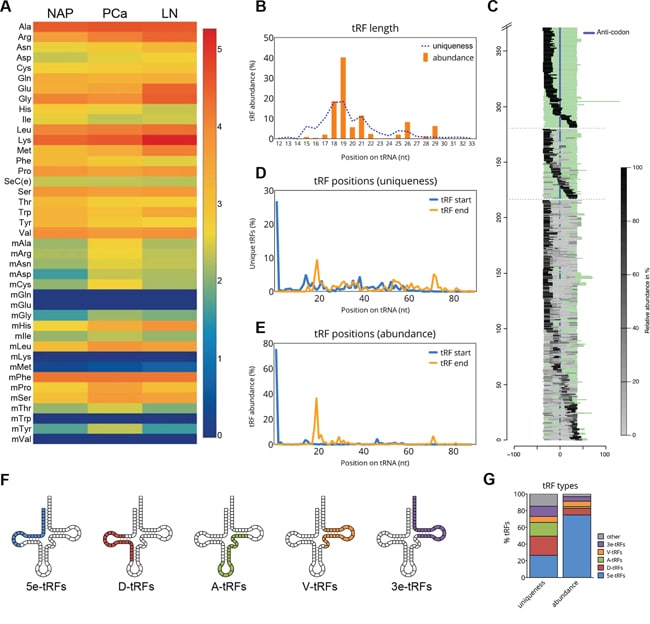
GSEA software was utilized to identify significantly related genes of low- and high-risk cases with 1000 permutations. Adjusted p values < 0.01 and false discovery rate < 0.25 were applied to define the differential expression genes with Benjamini and Hochberg method using the Limma package . Heatmap was plotted to visualize the difference in gene expression between the high- and low-group. Proteinprotein interaction network was constructed to reveal the correlations of DEGs using the Search Tool for the Retrieval of Interacting Genes online database. Most significant hub genes were selected using the Molecular Complex Detection plug-in of Cytoscape software . Functional annotations including Kyoto Encyclopedia of Genes And Genomes , molecular functions , biological processes , and cellular components were investigated to identify potential function enrichments of hub genes using the Cluster Profiler package of R software . Cancer Single-Cell State Atlas was utilized to investigate the potential function of the molecules involved in the TGF/SMAD4 signaling pathway.
What Is A Grade Group
In 2014, the International Society of Urological Pathology released supplementary guidance and a revised prostate cancer grading system, called the Grade Groups.
The Grade Group system is simpler, with just five grades, 1 through 5.
*Risk Groups are defined by the Grade Group of the cancer and other measures, including PSA, clinical tumor stage , PSA density, and number of positive biopsy cores.
Many hospitals report both the Gleason score and the Grade Group, but there may be hospitals that still report only the old Gleason system.
Impact Of Percent Gleason Pattern 4 On Active Surveillance
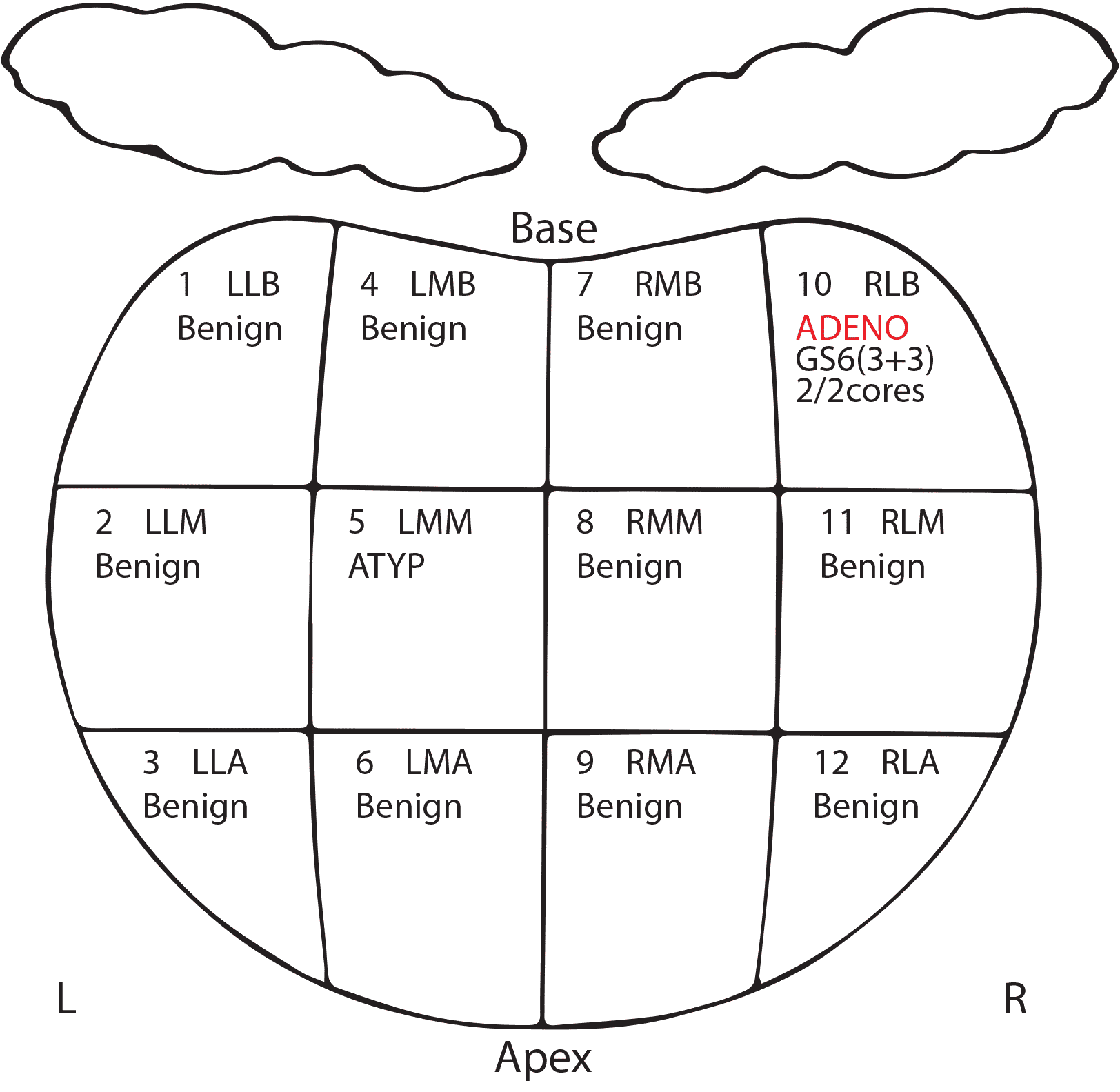
Active surveillance is now common practice for patients with clinically localized, low-volume Gleason score 3+3=6 prostate cancer . In addition, depending on age, comorbidity, PSA level, tumor extent, and patient desire, some Gleason score 3+4=7 tumors, with only focal, low-volume areas of pattern 4 disease, may be appropriate for active surveillance . Therefore, recording the percentage of pattern 4 in the pathology report is clinically relevant in such cases.
Recommended Reading: How To Milk Your Own Prostate
The Bogus Gleason 6 Prostate Cancer
The very common Gleason 6 type of prostate cancer href=http://www.ascopost.com/issues/june-10-2016/prostate-cancer-opinions-vary-on-gleason-scores-and-surgery/ rel=noopener> fails to behave as a cancer and should NOT be called a cancer. The all-inclusive prostate cancer label is deceitful by implying that all prostate cancers are equal and have the power to kill rapidly. It has been well established fact that the common Gleason 6 type of prostate cancer should not be called a cancer at all.
Dont Miss: Best Prostate Over The Counter Medicine
Correlation Of Percent Pattern 4 Between Needle Biopsy And Radical Prostatectomy Specimens
Correlations between Gleason scores at needle biopsy and corresponding radical prostatectomy remain a major issue, although the modified Gleason grading system has contributed to achieving better concordance. For instance, a study involving 7,643 matched biopsiesâprostatectomies published in 2012 revealed up-grading in 36.3%, 25.8%, and 30.6% of cases with biopsy Gleason scores 5â6, 3+4, and 4+3, and down-grading in 12.0% and 41.1% cases with biopsy with Gleason scores 3+4 and 4+3, respectively . To the best of our knowledge, only a few studies have assessed the concordance between the quantity of Gleason pattern 4 in prostate biopsy and prostatectomy findings.
In one study, a total of 256 biopsy cases with Gleason score 7 cancer divided into five groups, 1â20%, 21â40%, 41â60%, 61â80%, and 81â100%, according to the highest percentage of GP4 in the biopsy were correlated with histopathological findings of matched radical prostatectomy . Up-grading at prostatectomy was observed in 15.9% of biopsy Gleason score 3+4=7 cases and 11.5% of biopsy Gleason score 4+3=7 cases. Higher percentage of Gleason pattern 4 in biopsy was significantly associated with not only higher incidence of Gleason score â¥7 but also larger tumor volume and higher pathologic stage in prostatectomy specimens.
Also Check: What Can You Take For An Enlarged Prostate
Limitations Of The Gleason Grading System
Although current revisions have improved the Gleason grading system, it continues to have limitations. Recent modifications have made the Gleason grading system much more complex than its original version. This complexity can be confusing for patients and clinicians. Gleason score 6 is now recommended as the lowest grade to be assigned on prostate biopsy. This is counterintuitive in that the Gleason scale ranges from 2 to 10. Patients may assume that a diagnosis of Gleason score 6 on biopsy means their tumor is in the mid-range of aggressiveness rather than having the best prognosis. In addition, many former Gleason score 6 tumors are now reclassified as Gleason score 7 in the modified system. Modern Gleason score 6 tumors have a much better prognosis than reported in the older literature. Studies have shown that virtually no pure Gleason score 6 tumors are associated with disease recurrence after radical prostatectomy and pure Gleason 6 cancer at radical prostatectomy lacks the potential for lymph node metastases . Another problem in the modern Gleason grading system is the lumping of Gleason score 7, as noted above in the NCCN Risk Classification System. Whereas many clinicians consider Gleason score 7 on biopsy to be intermediate risk, multiple studies have shown that Gleason score 4+3=7 demonstrates worse pathological stage and biochemical recurrence rates than 3+4=7 .
How Do Doctors Find Out Your Grade Group
The pathologist grades each sample of prostate cancer cells from 3 to 5 based on how quickly they are likely to grow or how aggressive the cells look. You may hear this score being called the Gleason grade.
Doctors then work out an overall Gleason score by adding together the 2 most common Gleason grades. So for example, if the most common Gleason grade is 3, and the second most common is 4, then the overall Gleason score is 7. Or they might write the scores separately as 3 + 4 = 7. This combined score is now called the Grade Group.
There are 5 Grade Groups. Grade Group 1 is the least aggressive and Grade Group 5 is the most aggressive.
This is how the Gleason score and Grade Groups match up and what it means:
| Gleason score |
|---|
You May Like: Is Fish Oil Linked To Prostate Cancer
What Is Gleasons Sum
The Gleason scoring system has been revised recently. Only three Gleason grades, 35, are currently recognized in the revised system instead of the five original Gleason grades, 15. Original Gleason grades 1 and 2 are now included within the Gleason grade 3 tumors and considered to be nonaggressive. Gleason grades 4 and 5 tumors are considered more aggressive with metastatic potential and worse clinical outcomes. Prostate tumors are heterogeneous in terms of grade and behave according to the composition of grades within the tumor. Thus, tumors are graded by the sum of the two most important grades present as a Gleason score ranging from 6 to 10. Tumors of GS 6 are considered low grade , while GS 7 with Gleason grades 4 and 5 are high grade . GS is currently the best prognostic variable available to predict the clinical outcome of this disease.
Changing Role Of Caregivers
Family members and friends may also go through periods of transition. A caregiver plays a very important role in supporting a person diagnosed with cancer, providing physical, emotional, and practical care on a daily or as-needed basis. Many caregivers become focused on providing this support, especially if the treatment period lasts for many months or longer.
However, as treatment is completed, the caregiver’s role often changes. Eventually, the need for caregiving related to the cancer diagnosis will become much less or come to an end. Caregivers can learn more about adjusting to life after caregiving.
Read Also: What Problems Does An Enlarged Prostate Cause
Estimation Of Immune Cell Type Fractions
CIBERSORT is an analytical tool for estimating the cell composition of tissues from their gene expression profiles . In CIBERSORT, the fraction of 22 human immune cell types including naïve and memory B cells, seven T cell types, NK cells, plasma cells, and myeloid subsets in PCa tissues was estimated using the leukocyte gene signature matrix, termed LM22. PCa patients were divided into high- and low-SMAD4 expression groups, and the correlations between the fraction of each immune cell type and SMAD4 expression level were investigated and visualized using the vioplot package of R software. Pearsons co-expression analysis was performed to identify the proteins associated with the prognostic model and 0.4 was the cutoff value of the correlation coefficient. Spearman correlation analysis was utilized to investigate the correlated proteins with SMAD4. TGF- signaling pathways were visualized with BioRender.com.
A New Perspective On Your Health
For many people, survivorship serves as a strong motivator to make lifestyle changes.
People recovering from prostate cancer are encouraged to follow established guidelines for good health, such as not smoking, limiting alcohol, eating well, exercising regularly, maintaining a healthy weight, and managing stress. Regular physical activity can help rebuild your strength and energy level. Your health care team can help you create an appropriate exercise plan based upon your needs, physical abilities, and fitness level. Learn more about making healthy lifestyle choices.
It is important to have recommended medical checkups and tests to take care of your health.
Talk with your health care team to develop a survivorship care plan that is best for your needs.
Don’t Miss: Pet Scan For Prostate Cancer Recurrence
Stages Of Prostate Cancer
|
Any T, any N, M1 Any Grade Group Any PSA |
The cancer might or might not be growing into tissues near the prostate and might or might not have spread to nearby lymph nodes . It has spread to other parts of the body, such as distant lymph nodes, bones, or other organs . The Grade Group can be any value, and the PSA can be any value. |
Prostate cancer staging can be complex. If you have any questions about your stage, please ask someone on your cancer care team to explain it to you in a way you understand.
While the stage of a prostate cancer can help give an idea of how serious the cancer is likely to be, doctors are now looking for other ways to tell how likely a prostate cancer is to grow and spread, which might also help determine a mans best treatment options.
Screening Of Prognostic Proteins
![[1/3] AI based Gleason Grading for Prostate Cancer [1/3] AI based Gleason Grading for Prostate Cancer](https://img.healthyprostateclub.com/wp-content/uploads/13-ai-based-gleason-grading-for-prostate-cancer-by-zsfvishnu-medium.jpeg)
To evaluate the prognostic value of each protein, survival analyses were performed using the KaplanMeier method and univariate Cox regression method by log-rank test with 95% confidence intervals . The primary endpoint was overall survival , which was assessed from the date of receiving pathologic diagnosis to the date of death or the last follow-up. Based on the results of univariate Cox regression analysis, a total of 17 proteins significantly correlated with the prognosis of PCa were initially screened as candidate proteins, which were subsequently divided into low- and high-risk protein groups based on the hazard ratio =1 as the cut off value. The volcano map was plotted by R software using the ggplot2 package for visualizing the low- and high-risk candidate proteins . Next, to further elevate the prognostic accuracy, proteins with p value< 0.05 in both KaplanMeier analysis and univariate Cox logistic regression analysis were determined as prognostic proteins, including RAD50, SMAD3, and SMAD4. After multivariate Cox regression analysis, only RAD50 and SMAD4 were identified as proteins with the most prognostic value. Survival curves of PCa patients were plotted based on the expression of each prognostic protein respectively using the survival package of R software . The receiver operating characteristic curve was constructed and the area under the curve was calculated to evaluate the specificity and sensitivity of the prognostic value of proteins.
Recommended Reading: Institute For Prostate Cancer Research
Understanding Prostate Cancer: The Gleason Scale
Knowing the numbers
If you or a loved one has been diagnosed with prostate cancer, you may already be familiar with the Gleason scale. It was developed by physician Donald Gleason in the 1960s. It provides a score that helps predict the aggressiveness of prostate cancer.
A pathologist begins by examining tissue samples from a prostate biopsy under a microscope. To determine the Gleason score, the pathologist compares the cancer tissue pattern with normal tissue.
According to the
What Happens When Prostate Cancer Is Left Untreated
While most men undergo some form of treatment for their prostate cancer, some men today choose to not be treated for their prostate cancer. Instead, they may choose to have their healthcare providers monitor their cancer.
Known as active surveillance, it is common when the cancer is expected to grow slowly based on biopsy results, confined to the prostate, not causing any symptoms, and/or small. In active surveillance, healthcare providers will initiate cancer treatment only if cancer starts growing.
Others men may choose to not undergo cancer treatment because of a short life expectancy or other serious medical problems. They may feel that the risks or side effects of cancer treatment outweigh their potential benefits.
This option is certainly OK and reasonable in the right circumstancesrequiring a careful and thoughtful discussion with your healthcare provider and family.
Don’t Miss: How To Determine Prostate Cancer Stage
What Is The Gleason Grading System
Your Gleason score isn’t a separate test. It’s a number based on the results of your biopsy. You usually get it when you’re first diagnosed with prostate cancer.
The doctor uses the numbers 1 to 5 to grade the most common and second most common patterns of cells found in a tissue sample:
- Grade 1. The cells look very much like normal prostate cells.
- Grades 2-4. Cells that score lower look closest to normal and represent a less aggressive cancer. Those that score higher look the furthest from normal and will probably grow faster.
- Grade 5. Most cells look very different from normal.
The two grades added together are your Gleason score. Cancers will score 6 or more. A score of 7 means the cancer is intermediate, and a higher score means the cancer is more likely to grow and spread.
Your doctor will use this combined score along with the results of your PSA blood test and digital rectal exam to see how advanced your prostate cancer is. They’ll use this information to suggest the best treatment for you.
How The Gleason Scale Is Calculated
The scale is made up of a Gleason grade from your prostate biopsy.
1 being the least aggressive and looking mostly like normal prostate cells, and 5 being the most aggressive and looking mostly like irregular prostate cancer cells.
The scores are based on combining the grades of two differant biopsy sections .
The primary section which is graded from 1 to 5.
And the secondary section , also graded from 1 to 5.
Therefore your score consists of 2 Gleason scale grades
1 to 5 + 1 to 5 = 2 to 10.
i.e. 4 + 3 = 7. A GS of 7.
You May Like: What Kind Of Doctor Checks For Prostate Cancer
Active Surveillance For Gleason 6 Cancer
Per the Cancer Care Ontario guideline,1 active surveillance for patients with Gleason 6 disease should include:
- PSA testing every 3 to 6 months
- Annual digital rectal exam
- 12- to 14-core confirmatory transrectal ultrasound biopsy, including anterior-directed cores, within 6 to 12 months of starting surveillance, and then a serial biopsy every 3 to 5 years thereafter
REFERENCES
1. Chen RC, Rumble RB, Loblaw DA, et al: Active surveillance for the management of localized prostate cancer : American Society of Clinical Oncology Clinical Practice Guideline Endorsement. J Clin Oncol 32:2182-2190, 2016.
2. Cooperberg MR, Broering JM, Carroll PR: Time trends and local variation in primary treatment of localized prostate cancer. J Clin Oncol 28:1117-1123, 2010.
3. Loeb S, Folkvaljon Y, Curnyn C, et al: Uptake of active surveillance for very low-risk prostate cancer in Sweden. JAMA Oncol 3:1393-1398, 2016.
4. American Cancer Society: Key statistics for prostate cancer. Available at www.cancer.org/cancer/prostate-cancer/about/key-statistics.html. Accessed June 26, 2018.
5. Morash C, Tey R, Agbassi C, et al: Active surveillance for the management of localized prostate cancer. Available at www.cancercareontario.ca/en/guidelines-advice/types-of-cancer/2286. Accessed June 26, 2018.
6. Hamdy FC, Donovan JL, Lane JA, et al: 10-Year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med 375:1415-1424, 2016.
What Does It Mean If My Biopsy Mentions That There Is Perineural Invasion
Perineural invasion means that cancer cells were seen surrounding or tracking along a nerve fiber with the prostate. When this is found on a biopsy, it means there is a higher chance that the cancer has spread outside the prostate. Still, perineural invasion does not mean that the cancer has spread, and other factors, such as the Gleason Score and amount of cancer in the cores are more important. In some cases, findings perineural invasion may affect treatment, so if your report mentions perineural invasion, you should discuss it with your doctor.
Also Check: What Color Ribbon Is For Prostate Cancer
What Does Gleason 6 Mean
A Gleason score of 6 is different from other prostate cancer diagnoses because it means all the biopsy samples are grade 3 . Though the samples dont look like normal tissue, no grade 4 or 5 samples were found.
Gleason 6 prostate tumors are:
- Confined to the prostate
- Not causing any symptoms
There are changes at the cellular level, but the prostate cancer is likely slow-growing and has a low-risk of metastasizing, or spreading to other areas of the body.
This knowledge allows your doctor to monitor you and see how your tumor changes over time.
Tests To Identify Prostate Cancer Stage
After a prostate cancer diagnosis, your doctor will do tests to see how far the cancer has spread. Not all men need every test. It depends on the results of your biopsy, a test that checks tissue from your prostate gland for cancer. Tests that help your doctor figure out the stage of your prostate cancer include:
- CT scan of the abdomen and pelvis to see if the cancer has spread
- Nuclear medicine bone scan to see if the cancer has spread to your bones
- Surgery to check the lymph nodes in your pelvis for prostate cancer spread
Don’t Miss: Can Low Grade Prostate Cancer Become Aggressive
