Monitoring Of Metastatic Pca
Extent of Disease
New imaging modalities such as MRI, choline, fluciclovine, and PSMA-PET/CT, appear to have excellent sensitivity and specificity for lesion detection, although they have not yet been adequately tested in formal clinical trials. For example, the lymph node detection sensitivity of choline-PET/CT varies from 41.5 to 56%, while the specificity varies from 94 to 98.8%, with higher sensitivity observed for the detection of LN > 5 mm, and particularly outside lymphadenectomy territories . Data on the impact of this gain in sensitivity on patient care is lacking. Moreover, the CT scan of the past bears little resemblance of the CT scanning we use today, particularly with resolution. And PSMA-scans vary in the radio-isotope used as well as the molecules used as imaging probes. These PSMA-scans are generally undertaken in conjunction with an axial imaging modality.
Table 6. Assessment exams in former phase III trials.
Table 7. Assessment exams in former phase III trials in patients who are resistant to castration in the first line setting.
Table 8. Assessment exams in former phase III trials in patients who are resistant to castration in subsequent lines.
Response to Treatment
To date, limited data are available on the use of modern imaging in the evaluation of therapeutic response. This is particularly the case with fluciclovine-PET/CT.
Choline-PET/CT
PSMA-PET/CT
NaF-PET/CT
Bone-scan
MRI
Search For Metastases In Recurrent Disease: Restaging
About 30% of patients treated radically for high or very high risk PCa have biochemical recurrence , and with modern imaging, the diagnosis of oligometastatic PCa has become more common . Current guidelines from NCCN and EAU but stay heterogeneous across different parts of the world. For example, National Comprehensive Cancer Network guidelines consider 18F fluciclovine-PET-CT for prostate cancer biochemical recurrence after radical prostatectomy1 , whereas European Association of Urology guidelines recommend prostate-specific membrane antigen PSMA-PET/CT . Tables 4, 5 summarize the literature on the following issues.
Table 4. Currently available functional and targeted imaging methods for detection of suspected recurrence in PCa with biological relapse in patient-based analyses.
Table 5. Sensitivity and specificity of currently available functional and targeted imaging methods for detection of suspected recurrence in PCa with biological relapse in patient-based analyses.
Is There Residual Tumor in the Prostate Bed?
If abnormalities were best appreciated on T2W axial images as focal hypointense lesions , dynamic contrast-enhanced imaging or DWI in combination with T2W at 3T with a phased-array coil, appears to be more useful than T2W alone in evaluating suspected soft tissue lesions of the prostate bed after RP .
Is There LN Involvement?
Is There Bone Disease?
Developmental History Of Wb
Reports comparing BS with MRI for the detection of bone metastases have been available since the last century . However, our research has indicated that the oldest reports that included the term whole-body MRI date back to 1997 . Since the beginning in the twenty-first century, various devices have been developed to enable a whole-body scan in a single session without the need to change the directions of the body, which include multichannel coil and table-top extenders .
In 2004, Takahara et al. used DWI with background body signal suppression . Until the development of this method, DWI was predominantly used for investigations of the central nervous system, especially in cases of acute stroke . However, several researchers have reported that various malignancies in the body show similar high signal intensities .
To date, many therapeutic agents have been developed , such as radium-223 dichloride for castration-resistant prostate cancer , which has a high occurrence of bone metastases . With the increase in the number of treatment options and improvements in patient survival, the use of WB-MRI for providing accurate diagnosis and therapy monitoring has become crucial.
Since the mid-2010s, research has focused on the standardization and therapy monitoring of WB-MRI .
Fig. 4
MET-RADS-P template . The MET-RADS-P template form allocates the presence of unequivocally identified disease to 14 predefined regions of the body
Don’t Miss: Will Blood Test Show Prostate Cancer
The Role Of Radiology In Metastatic Prostate Cancer
Rajan T. Gupta, MD:Imaging is used for the diagnosis of metastatic prostate cancer in many different ways. We can be looking for solid organ metastatic disease as well as bone metastatic disease. Depending on the situation with the PSA, we may be looking at different areas. So, the different modalities that are available inside of the armamentarium of the radiologist, as well as the oncologist, is CT, PET/CT, MRI, and then also some multiparametric MRI of the prostate.
The decision tree about when to do imaging in patients with metastatic prostate cancer is dependent on local patterns as well as some of the national guidelines. I think the key things we have to be looking at are, what kind of treatment the patient had, what their PSA trajectory is, and what is their level of suspicion that they have metastatic diseasewhether that be clinical symptoms, etc.
So, the patient who we talk about in this case here is really interesting in the fact that they had what was suspected to be low-grade disease and then they were on active surveillance for a long time. Once a decision was made to actually pursue more active treatment, part of that was informed by a biopsy change that had shown that they actually had more aggressive disease, and I think that thats a potential place where we could implement something like multi-parametric MRI to assist.
Transcript edited for clarity.
Addressing Concerns About Previous Trials
In recent decades, a number of randomized clinical trials have tested different ways to use radiation therapy for bone metastases. These studies employed the tools available at the time, including 2-dimensional radiation therapy, and a relatively low dose of radiation, such as 8 gray .
Results from some of the trials have suggested that delivering palliative radiation in a single dose provides equivalent pain relief as delivering it in multiple smaller doses, the study authors noted.
But single-dose regimens have also been associated with higher rates of having to re-treat patients whose pain has returned, the authors added.
Our study addresses the concerns with the previous trials that may contribute to reasons clinicians are not using the single-dose treatment for patients, said Dr. Nguyen. The trial’s goal, she continued, was to show that the single dose was equivalent, or not inferior, to the multiple-dose regimen in terms of pain relief.
Patients in the single-dose group received a higher dose than previous trials, either 12 or 16 Gy, depending on the size of their metastatic bone tumors. Patients in the other group received a total of 30 Gy, delivered over the course of 10 treatment sessions.
To compare the outcomes of the two treatment regimens, the researchers analyzed pain questionnaires filled out by patients and measured how much pain medication each patient used.
Don’t Miss: Does Regular Ejaculation Help Prostate
Inclusion And Exclusion Criteria
Only original manuscripts and reviews published in indexed and peer-reviewed journals and written in English between August 1999 and December 2019 were considered. Cross-sectional studies, case reports, published abstracts, dissertation materials, and conference presentations were excluded. Of 1,725 potential articles from the literature search, 105 were selected, including 16 literature reviews, 5 meta-analyses, 11 guidelines or position papers, and 73 original articles.
Concluding Assessment And Discussion
The detection and evaluation of bone metastases is a matter of high clinical importance. Bone metastases are revealed by imaging studies either by anatomical visualization or by the detection of metabolic turnover in the metastasis itself or in the surrounding bone.
An analysis of the literature on bone metastases indicates a number of current trends:
Also Check: Mouse Prostate Cancer Cell Line
Mri Can Track Bone Mets Treatment Response In Prostate Cancer
MRI offers new hope for evaluating how well prostate cancer bone metastasis are responding to chemotherapy. An exciting new paper by a British team at the Institute of Cancer Research reports their original pilot study confirming MRI tracking success.i
The authors explain that when advanced prostate cancer no longer responds to androgen deprivation therapy and begins to spread , about 84% of patients will have bone mets. Standard CT imaging and bone scintigraphy are often not accurate in assessing the extent and volume of the bone mets, nor can they accurately tell how well the mets are responding to chemotherapy treatment. The PSA blood test is also not a reliable indication of treatment progress. This is disheartening for doctor and patient alike.
Although the 2017 study had a small sample size, it is still the largest series to date using whole body MRI/DWI to monitor bone mets treatment response in mCRPC patients. The authors point out that these data indicate that whole-body DWI may have a role in bone metastases response assessment in mCRPC, without the need for ionizing radiation or intravenous contrast material Many patients are concerned about exposure to radiation or the radioactive isotopes used in bone scan contrast agents, while MRI is radiation-free. In addition, whole body MRI/DWI has the potential to detect mets in soft tissue and lymph nodes as well as bones, giving more detailed information about a patients burden of disease.
- CATEGORY:
Incidence Of Intracranial Metastasis In Patients With Prostate Cancer
This review identified a total of 5644 imaging examinations, inclusive of the brain, performed on 4341 unique prostate cancer patients. A total of eight prostate cancer patients were identified as having an intracranial metastasis from prostate cancer, yielding an incidence of 0.18%. Of the 5644 imaging examinations reviewed, the majority were 68Ga-PSMA PET/CT scans followed by FDG PET/CT and brain MRI scans. Although 68Ga-PSMA PET/CT scans are the standard method used at our center for prostate cancer staging/restaging, it is not uncommon for patients to undergo FDG PET/CT instead, reasons for this are typically either because of the presence of a prostate cancer variant with limited PSMA expression or because the patient has concurrent primary cancers and the FDG PET/CT scan is performed to monitor both cancers. Brain MRIs are largely performed to investigate spinal cord and cranial disease, new neurological symptoms, or new lesion/s observed on other imaging modalities.
Recommended Reading: At What Age Should You Have Your Prostate Checked
Table : Diagnostic Imaging Equipment In Canada335253
| PEI, YT, NT, NU | NL, PEI, SK, YT, NT, NU |
NA = not available NS = Nova Scotia NT = Northwest Territories NU = Nunavut PEI = Prince Edward Island YT = Yukon.
Return to Summary Table
Criterion 11: Relative cost of the test
Fee codes from the Ontario Schedule of Benefits were used to estimate the relative costs of bone scanning and its alternatives. Technical fees are intended to cover costs incurred by the hospital . Maintenance fees are not billed to OHIP estimates here were provided by St. Michael’s Hospital in Toronto. Certain procedures are paid for, in part, out of the hospital’s global budget these estimates were provided by The Ottawa Hospital. It is understood that the relative costs of imaging will vary from one institution to the next.
According to our estimates , the cost of whole body bone scan with 99mTc-based radioisotopes is $278.70. 18F-PET and 18FDG-PET are significantly more costly alternatives.
Mri For Assessment Of Bone Metastases
Magnetic resonance imaging is potentially the technique of choice in evaluating prostate bone metastases as it is sensitive to early changes in bone marrow that precede the osteoblastic response in the bone matrix. Metastasis to bone marrow leads to a lengthened T1 relaxation time and signal loss, which contrasts with the surrounding high signal marrow fat. The conspicuity of bone metastases can sometimes be increased by T2-weighted fat-suppressed sequences such as short tau inversion recovery .
Schematic describing the relationship between patterns of tumour seeding in bone marrow and imaging findings.
The RECIST criteria applied to MRI of the axial skeleton in one small study have confirmed the superior sensitivity of MRI to bone scintigraphy in the detection of bone metastases and have shown that it may have a role in quantitatively following bone metastases. Despite classifying diffuse bone involvement as non-measurable because it was impossible to obtain longest axis dimensions, this study increased the number of patients with measurable metastatic lesions by 29% .
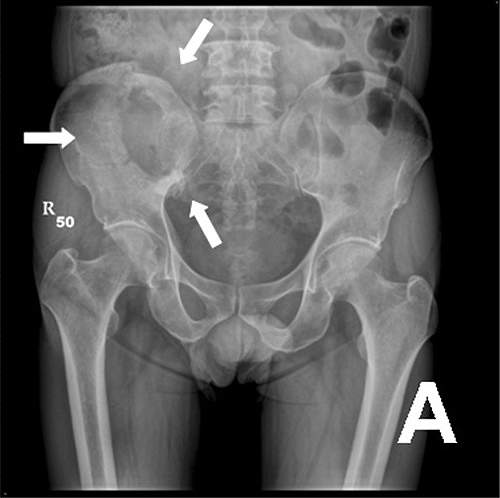
Comparison of MRI and MDP bone scintigraphy: pelvic T1W MRI and b750 DWI of a patient with carcinoma of the prostate shows a new small metastasis involving the left neck of femur. This small intramedullary lesion has not evoked enough osteoblastic reaction to become visible on bone scintigraphy .
You May Like: When Should Guys Start Getting Prostate Exams
Intracranial Metastasis From Prostate Cancer: Investigation Incidence And Imaging Findings In A Large Cohort Of Australian Men
- Received:
How to cite this article: McBean R, Tatkovic A, Wong DC. Intracranial metastasis from prostate cancer: Investigation, incidence, and imaging findings in a large cohort of Australian men. J Clin Imaging Sci 2021 11:24.
Local Rt In Oligometastatic Disease

As aforementioned, there are indications that the benefit of local RT may be dependent on the burden of metastatic disease. As a result, several studies have explored the role of RT in oligometastatic disease, albeit with no general consensus regarding the definition of oligometastatic disease. An early study defined it as an intermediate state between purely localized lesions and widely metastatic disease . Subsequent studies have found better survival in patients who had less than five and six bone metastases respectively, lending further credence to the idea of oligometastases .
Don’t Miss: Metastasis Directed Therapy Prostate Cancer
Citation Doi & Article Data
Citation:DOI:Assoc Prof Frank GaillardRevisions:see full revision historySystems:
- Mixed sclerotic and lytic bone metastases
- Mixed osteolytic and osteoblastic metastases
- Mixed lytic and blastic bone metastases
Mixed lytic and sclerotic bone metastases refer to metastatic bone disease with both sclerotic and lytic bone metastases or bone metastases with both components.
Search For Metastases In Localized And Locally Advanced Prostate Cancers
The search for metastases was performed based on the presence of clinical symptoms, from the diagnosis of localized PCa in asymptomatic patients, or in the follow-up of treated PCa. Lymph node or bone metastases are rarely detected in this context .
In patients followed-up for localized PCa, metastases should be sought according to the risk group defined by the National Comprehensive Cancer Network or by the European Association of Urology guidelines , to estimate the 5-year biological relapse risk. These guidelines are heterogeneous across the world. Hence, it is of interest to provide answers for routine clinical practice to the following question: How can metastases in LN, bone, or locoregional disease in seminal vesicles be better diagnosed?
Is There Disease in the LN ?
Computed tomography scans are mainly performed to diagnose LN involvement. Nevertheless, there is difficulty with CT scan validation, either at initial diagnosis or for recurrence.
Table 1. Sensitivity and specificity of currently available functional and targeted imaging methods for LN staging of PCa.
Is There Disease in Seminal Vesicles ?
Table 2. Sensitivity and specificity of currently available functional and targeted imaging methods for detection of SVI in PCa.
Is There Disease in Bones ?
Table 3. Sensitivity and specificity of currently available functional and targeted imaging methods for bone staging of PCa.
You May Like: What Is Grade Group 2 Prostate Cancer
Eligibility Criteria And Patient Characteristics
We identified consecutive PCa patients who underwent prostate MRI before treatment at our institution between January 2000-June 2014 . Patients were excluded if they had recurrent prostate cancer, pre-existing cancer diagnosis in another organ, < 1 year follow up, or incomplete data , resulting in a final population of 3765 patients.
Nested within this cohort, we used a stratified sampling design to define a subset of patients. Stratifying on the year in which the prostate MRI was done, we selected three patients without bone metastases for every patient with bone metastases. Two independent readers evaluated the prostate MRI exams for MRI features in this subsample. This sampling design was used to facilitate the image review for the purpose of this study without the need for re-interpreting each of the 3700 MRI examinations in the entire cohort.
Skeletal Scintigraphy Spect And Spect
Skeletal scintigraphy with labeled phosphonates enables visualization of local bone metabolism , which is activated in an early phase of some types of cancer. It thus detects metastases best when they are associated with marked reactive hypermetabolism of bone or generate bone matrix themselves . In contrast, scintigraphy is relatively insensitive for tumors that cause areactive osteolysis or isolated bone-marrow infiltration . Moreover, bone matrix regeneration after the successful treatment of a bone metastasis can induce metabolic activation, which is sometimes misinterpreted as progressive diseasethe so-called flare phenomenon. Skeletal scintigraphy is obligatory before radionuclide treatment with phosphonates coupled to alpha- or beta-emitting isotopes, e.g., 223Ra treatment for prostate cancer.
Skeletal scintigraphy and SPECT. In this patient with prostate cancer, 99mTc-MDP scintigraphy reveals bone metastases. The SPECT image is free of superposition effects and thus enables the precise localization of many metastases.
Recommended Reading: What Is Life Like Without A Prostate
