Ongoing Studies And Future Directions
As investigation into the curative potential of MDT in OMPC continues, several major questions remain unanswered. Can MDT alone produce durable clinical benefits and, if so, how can patients be most appropriately selected? Does MDT provide additive benefit when combined with ADT and other systemic therapies? Does MDT have clinical benefit in oligoprogressive CRPC? Can MDT be combined with immunotherapy to encourage a systemic antitumor response?
Multiple prospective randomized clinical trials are ongoing to answer these first two questions. Similar to STOMP, the Baltimore ORIOLE trial is evaluating progression, ADT-free survival, and immunologic correlates in men with OMPC randomized to receive observation or SABR. PCS IX is investigating the clinical benefit of adding SABR to systemic treatment with ADT and enzalutamide in patients with CRPC. CORE and STEREO-OS are randomizing patients with prostate, breast, or lung cancers with 1-3 oligometastases to standard of care systemic therapy with or without SABR. STORM is randomizing patients with oligorecurrent prostate cancer confined to the lymph nodes to MDT with six months of ADT ± whole pelvic radiotherapy. Finally, the Movember GAP6 international initiative is pooling tissue samples from clinical trials such as these in order to promote collaborative efforts to facilitate further biologic understanding of the oligometastatic state in prostate cancer.
The Clinical Argument For Mdt In Oligometastatic Prostate Cancer
In their editorial Oligometastases, Hellman and Weichselbaum discuss the opposing hypotheses of cancer metastasis as well-ordered and predictable based on knowable anatomic and physiologic data or, alternatively, as the manifestation of cancer as a systemic disease with widespread, initially undetectable micrometastases present at the time of diagnosis but maturing to clinical relevance over time ultimately they propose that our understanding of cancer behavior is most consistent with a continuum spanning these extremes and with many intermediate states. Their formulation of a clinical significant state of oligometastases describes a point on this continuum where metastatic disease is present but potentially curable through consolidation of both the primary tumor and all metastases with local therapies .
The oligometastatic state in prostate cancer includes de novo hormone naïve metastatic disease present at initial diagnosis, oligorecurrent disease following definitive primary treatment with surgery and/or radiation, and isolated areas of treatment-resistant or oligoprogressive disease which persist after otherwise successful systemic therapy such as in castration-resistant prostate cancer .
How Is Mdt Using Ablative Radiotherapy Delivered
Target Volumes, Dose, and Fractionation
Optimal ablative dosing is contingent on multiple factors including radiobiological properties of prostate cancer cells and dosimetric constraints of adjacent organs at risk. Studies reporting on the use of SABR for the definitive treatment of prostate cancer have utilized regimens with biological effective doses ranging from 168 to 407 Gy with some evidence suggesting BED of 200 Gy is associated with better disease control.
STOMP, the only published prospective randomized trial of MDT in oligometastatic prostate cancer, utilized a dose of 30 Gy in 3 fractions. Other retrospective and observational studies of MDT in oligometastatic prostate cancer utilized doses ranging from 16 to 50 Gy in 1 to 10 fractions (Table 2 with some suggestion that a BED higher than 100 Gy is associated with superior local control.
Toxicity from SABR is generally mild across several lesion locations. Every other day scheduling is often used as it has shown reduced toxicity compared to daily treatments in definitive treatment of the prostate, however even with daily treatments toxicity rates remain low .
Recommended Reading: How Long For Prostate Biopsy Results
Local Therapy For Metastatic Disease
MDT intended to remove or ablate individual metastases has become increasingly feasible. The earliest evidence of MDT comes from a surgical series of pulmonary and hepatic metastasectomies. The feasibility of applying existing surgical techniques to metastatic disease laid the groundwork for demonstrating that aggressive MDT might confer a worthwhile benefit. In a number of settings, surgery remains the best option for MDT. However, given the complexity of metastatic behaviour and the number of organ systems that can be involved, there has been an effort to develop minimally or non-invasive methods for delivering definitive MDT.
Mdt In Disease Control
The development of trials and identification of patients who would benefit from MDT are currently limited by a simplistic definition of oligometastasis and minimal understanding of what drives metastatic biological potential. The most important among these, and inherent to the term itself , is the number of metastases. Although it is pragmatic to consider patients with a limited number of metastases for MDT, the advancement of radiotherapy technology has the potential to broaden MDT indications to those with numerous metastases. In such cases, it might become necessary to reassess the goal of MDT and consider the benefits beyond eradicating specific metastases. While the intention of ablative therapies is to kill or remove a metastasis completely, systemic treatments for metastatic cancer patients usually have a more modest, albeit still valuable, goal of disease control. Palma et al. pose an intriguing question of whether administering MDT in the form of SABR to more widespread metastases might be a meaningful disease control strategy. Even if ablative doses to all lesions are not achieved, which is a likely prospect when considering radiation for numerous lesions in diverse locations, lower doses of radiation are usually feasible and provide meaningful local control. SABR-COMET-10 is pushing the boundaries of this concept and should provide insight into whether the limits that determine which patients we consider for MDT should be pushed even further.
Recommended Reading: What Can Be Done For An Enlarged Prostate
Clinical Studies Of Mdt
After decades of hypothesis-generating retrospective reports, an important milestone has been achieved with the publication of randomised evidence supporting local therapy for solid metastatic disease. SABR-COMET, an open-label Phase 2 international study, randomised patients with solid tumours and up to five metastases to standard systemic therapy or standard therapy plus stereotactic ablative radiotherapy to all metastatic lesions. The studys primary endpoint of improved overall survival was met with a median OS of 28 months in the control group and 41 months in the SABR arm. With longer follow-up, they recently reported a striking 5-year OS benefit for SABR, 42.3% versus 17.7% in the control arm. A Phase 2 study from the MD Anderson Cancer Center focussed on patients with non-small cell lung cancer with up to three metastases who did not progress after at least 3 months of first-line systemic therapy, randomising between continued standard of care or local consolidative therapy to all metastatic sites. The study was closed early after the data safety and monitoring board found clear evidence of superiority in the primary endpoint of progression-free survival in patients receiving local consolidative therapy. OS, a secondary endpoint, was also improved, with a median of 17 months in the control arm and 41.2 months in the local consolidative therapy group. Clinical benefits have been shown in other Phase 2 randomised studies, as summarised in Table .
What Is The Current State Of Oligometastatic Prostate Cancer
Recently, randomized clinical trials across multiple disease sites have demonstrated improvements in progression-free survival with the addition of metastasis-directed therapy for oligometastatic disease, possibly due to ablation of subpopulations that would otherwise have led to subsequent dissemination or the nurturing of systemic microscopic disease toward macroscopic colonization. In line with this hypothesis, some of these randomized trials have demonstrated that local consolidation of macroscopic metastases delayed the time to development of new metastases and improved overall survival. Despite these early successes, key questions remain unanswered regarding the use of MDT in oligometastatic prostate cancer. How can we best identify patients likely to benefit from MDT? In the case of castration-sensitive prostate cancer, can we omit androgen deprivation therapy? What are the best MDT systemic therapy combinations?
Randomized Clinical Trials Demonstrating Improvements in Progression-Free Survival with the Addition of Metastasis-Directed Therapy
You May Like: What Is The Best Prostate Toy
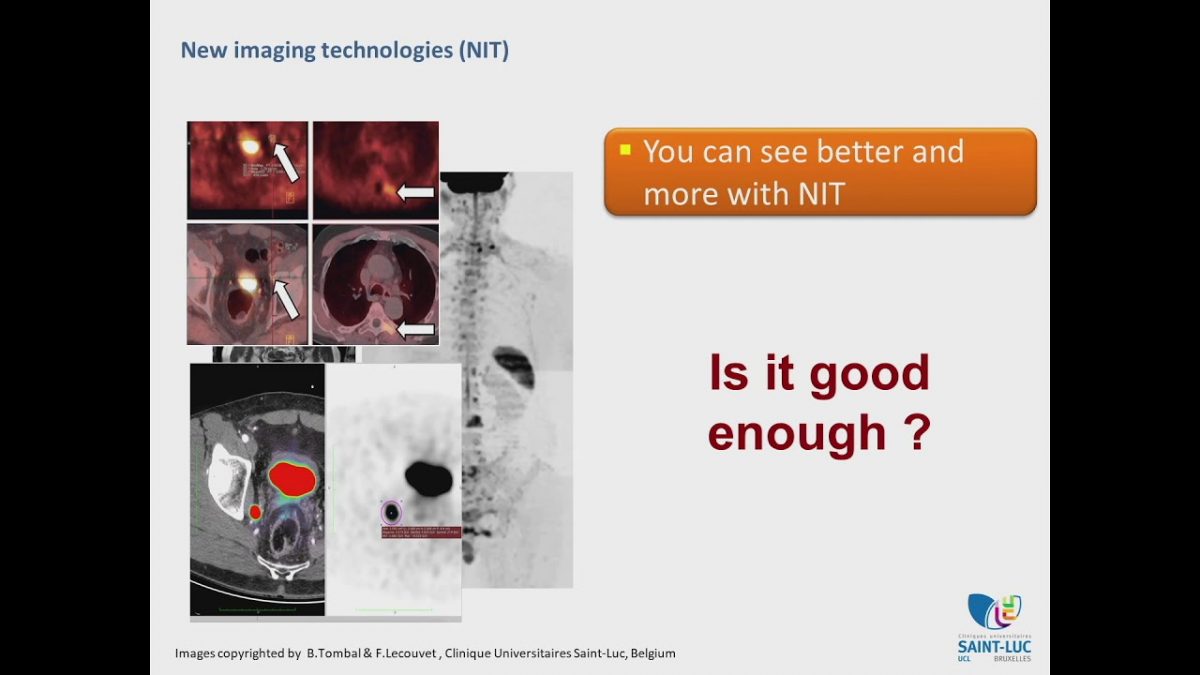
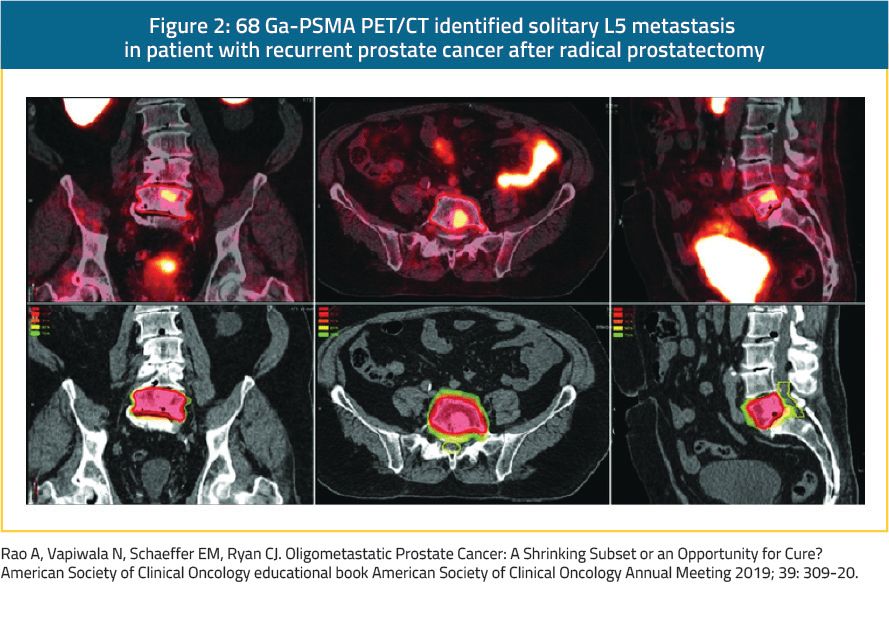
Stereotactic Ablative Radiotherapy And Molecular Imaging Are Potentially A Powerful Combination For Cure Of Oligometastatic Prostate Cancer
MDT entails direct local consolidative treatment of metastatic lesions and is commonly achieved through surgical metastasectomy or nodal dissection thermal or chemical ablation or the high-dose-per-fraction, precisely targeted radiotherapy known as SABR. Although for many metastatic lesions any of these local approaches would be reasonable as MDT, the noninvasive nature of SABR, the ease with which adjacent at-risk normal tissues can be spared, and the excellent tolerance in even the most medically comorbid has tipped the scales in favor of SABR as the MDT modality of choice. SABR may be even more effective for prostate cancer than for other histologies because of the radiobiologic characteristics of prostate cancer , leading to a widened therapeutic window and offering greater efficacy at a higher dose per fraction and shorter total treatment times.
Concurrent Adt And Other Systemic Therapies
One goal of MDT in OMPC is to avoid systemic therapy and its associated side effects. However, a more aggressive approach may involve intensification aimed at simultaneously eradicating sites of microscopic metastatic disease in addition to local consolidation with SABR through the use of concurrent ADT, non-castrating antiandrogens such as enzalutamide, chemotherapies such as docetaxel, and even complimentary forms of systemic radiation such as radium-223. No level 1 evidence exists for this treatment paradigm, however retrospective data suggests a possible improvement in distant progression-free survival with the concurrent use of ADT and SABR. Therefore, prospective studies are on-going to address this question.
Recommended Reading: High Risk Prostate Cancer Symptoms
Mdt And Symptom Management
Although MDT therapy holds substantial promise in improving the survival of patients, it is also important to consider the important roles MDT plays in symptom management. Radiotherapy has numerous roles in managing pain, bleeding, and mechanical obstruction from metastases. These well-established indications are outside of the scope of this review, but developing indications for MDT in preventing and managing adverse events is worth mentioning. One such indication is the prevention of skeletal-related events that can result from metastatic progression, such as spinal cord compression or long bone fracture. Skeletal-related events result in the use of significant healthcare resources, and the prevention of skeletal-related events has been shown to reduce healthcare costs. Our centre is carrying out a randomised study comparing standard of care versus palliative radiotherapy for asymptomatic but high-risk skeletal metastases, with a primary endpoint of reducing the rate of skeletal-related events . Although most of this review focusses on the roles of MDT in prolonging OS or PFS, quality of life and healthcare-cost-related endpoints are important parameters to consider as trials intended to prevent adverse events from metastases are developed.
Sabr May Facilitate Delay Of Adt Initiation
Controversially, the favorable safety profile and durable lesion control afforded by SABR has led to interest in using this approach to forestall initiation of ADT, in so called oligorecurrent men, in order to avoid unpleasant side effects including hot flashes, fatigue, and sexual dysfunction. The shining example of this approach is the STOMP trial, which randomized men with 3 or fewer extracranial prostate cancer metastases to surveillance alone or SABR to all detectable foci of disease. With a median follow-up of 36 months they observed that median ADT-free survival in men receiving SABR was 21 months vs 13 months with surveillance alone. The clinical relevance of this finding remains a point of active disagreement amongst experts. Those in favor of early ADT initiation may cite the TOAD trial , which showed an overall survival benefit with immediate initiation of ADT as compared to a recommended 2 year delay. Those opposed may cite the overall lack of impact on development of metastases with early ADT in the analysis of US Department of Defense patients by Moul et al. and the results of EORTC 30891, which showed similar prostate cancer-specific survival in men not suitable for local treatment receiving early vs delayed ADT. Despite the controversy, an ADT backbone is the standard of care in men with metastatic disease and other novel approaches including MDT are still best evaluated under the auspices of a clinical trial.
You May Like: When To Get A Prostate Exam
Inclusion And Exclusion Criteria
- Histologically proven initial diagnosis of adenocarcinoma of the prostate.
- mCRPC setting, with testosterone level< 50ng/dl or 1.7nmol/l .
- Oligoprogressive disease, defined as the progression of pre-existing metastatic disease, and/or the appearance of new metastases and/or the appearance of a local relapse with a maximum of 3 lesions in total. Oligoprogression is diagnosed on conventional imaging with CT and bone scan.
- Patients currently treated with ADT, whether or not combined with another systemic treatment such as ARTA, chemotherapy or radium-223. Denosumab is allowed but not considered as second-line systemic treatment.
- Prior treatment of the primary tumor by radiotherapy or surgery. If the primary tumour is not treated, local therapy should be added to the treatment.
- WHO performance status 02.
- Age> = 18years old.
- Absence of any psychological, familial, social or geographical condition potentially hampering compliance with the study protocol and/or follow-up schedule. Those conditions should be discussed with the patient before registration in the trial.
- Patient should be presented at the multidisciplinary tumour board of the local hospital in which the therapy will be given.
- Before patient registration/randomization, written informed consent must be given according to ICH/GCO and national/local regulations.
Exclusion Criteria
The Promise Of Metastasis
Historically, metastatic disease was thought to represent an all-or-nothing incurable state, distinct from curable localized disease and necessitating treatment with systemic therapy alone. The role for life-prolonging local therapy was known to be futile. This dogma was challenged in the 1990s with the reframing of metastasis as a spectrum rather than binary, resulting in the postulation of a low-volume metastatic state, given the term oligometastasis, which may actually be curable with definitive local therapy.
Read Also: How To Tell Prostate Cancer
When To Treat Prostate Cancer Metastases With Ablative Radiation
Selecting Patients for Metastasis Directed Therapy – Definitions of Oligometastatic Prostate Cancer
Quantitative cutoffs based on the number of metastatic foci are often used to define the oligometastatic state for simplicity as well as association with disease outcome. Nine prospective clinical trials have numerically defined the oligometastatic state in prostate cancer three allowed up to three metastases, two up to four, three up to five, and one up to 10. The literature of other published retrospective reviews generally included five or fewer metastatic foci.
As detection methods continue to evolve, technological differences between studies must be taken into consideration when evaluating outcomes of MDT patients with five or fewer lesions detectable with leading-edge methods may represent a population with a lower disease burden than those identified using conventional imaging alone.
Progress With Biological Correlatives
As we seek a deeper understanding of the molecular underpinnings of metastasis and biological features that could help select patients for MDT, it is also critical to maximise information obtained from completed and ongoing clinical trials. For instance, Tang et al. evaluated circulating tumour DNA , cytokines, and the T cell repertoire from biospecimens collected during the Phase 2 study of NSCLC patients receiving MDT after induction chemotherapy and found that MDT was associated with a reduction in ctDNA and the expansion of a subset of T cell clones. Interestingly, in a small subset of patients from whom serial ctDNA samples were taken, a rise in ctDNA mutation burden significantly predated clinical progression of the disease. Biological correlatives are built into the majority of ongoing studies in Table . Hypotheses generated from such analyses will provide valuable insight into the systemic response to MDT and how clinicians evaluate the success of MDT and monitor disease recurrence.
Recommended Reading: How To Determine Prostate Cancer Stage
Metastasis Directed Therapy For Oligometastatic Prostate Cancer
08 May 2020
The increasing use of PSMA PET scans to image prostate cancer means that metastatic prostate cancer can be detected and targeted more effectively. For a specific type of metastatic disease, known as oligometastatic prostate cancer, emerging evidence suggests that treating the individual oligometastatic sites of disease by metastasis directed therapy could delay both the progression of the cancer and the need for androgen deprivation therapy.
Oligometastatic prostate cancer is when metastasis occurs in a small number of unique sites in the body, the term oligo being derived from Greek oligos for small or oligoi for few. In 2016, a review article by Tosoian et al published online by the journal Nature Reviews Urology defined oligometastatic prostate cancer based on an analysis of 11 studies as prostate cancer that has spread to five or less sites outside of the pelvis region.
Studies suggest that oligometastatic prostate cancers vary considerably. In some cases, the disease progresses quickly to widespread metastatic disease, while in other cases the progression to widespread disease is much slower or does not occur at all.
These studies all show that MDT for the treatment of oligometastatic prostate cancer shows promise. But the studies were all very different in design and more research is needed before we can determine how best to treat this disease.
For a printable PDF version of this article, , or on the download link at the top of the article.
Patient And Treatment Characteristics
Eighty prostate cancer patients with oligometastatic disease underwent MDT for bone metastases. Table shows patient characteristics. Median age at diagnosis of oligometastases was 72 years . In the majority of cases, the initial T-stage was T3, and the initial N-stage was N0. Half of the patients had a Gleason score9. Most patients initial treatment was radical prostatectomy , and 31.3% subsequently had radiotherapy due to locoregional recurrence. Initial treatment was definitive radiotherapy, primary systemic therapy and no pretreatment in 5.0%, 11.3% and 3.8%, respectively. The median time between primary treatment and diagnosis of oligometastates was 22.1 months . At the time of MDT 31.3% of patients had de-novo synchronous oligometastatic disease, 46.3% had de-novo metachronous oligorecurrence after primary treatment and 22.5% had either de-novo oligoprogressive disease, repeat oligometastatic disease or induced oligometastatic disease. Forty-three patients had already ADT at some point during their disease course, 18 patients had CRPC.
Table 1 Patient characteristics
Don’t Miss: What Does Prostate Inflammation Feel Like
