Testosterone As A Drug
The male hormone testosterone can feed the growth of prostate cancer, but in an interesting twist, when given in a very specific way, it may also cause its demise. Drugs that block the action of testosterone are commonly used to treat men with advanced prostate cancer therapy. Cutting off the supply of testosterone to the cancer works for a time, but eventually prostate cancer cells figure out a way around it and begin to grow again. Other drugs work at the molecular level to cut off prostate cancer cells access to testosterone, but their impact is temporary and comes with unpleasant side effects. Men who have long-term hormone ablation have a good response initially, but eventually they become resistant to therapy, and then there arent many options left for them, says prostate cancer expert Samuel Denmeade. These are the men most at risk of dying from prostate cancer.
Men were hugging me because they felt so good. People are clamoring for it, says Denmeade. We get emails from men all over the country and the world. Denmeade says they are still learning about the best way to safely give the therapy. So far, the side effects have been low grade, as long as the treatment is limited to men who are asymptomatic without any pain due to prostate cancer, he says. In some cases, the testosterone therapy makes men feel increased energy, less fatigue and restored sexual function.
Some Characteristics Of Testosterone
Testosterone is principal male androgen, sex hormone and anabolic steroid. It is found not only in humans, but also in many other vertebrates. In males, testosterone is secreted by Leydig cells in testicles, in females by theca cells in ovaries. Small amount is produced also in zona reticularis of adrenal cortex in both genders and in placenta. Chemically , it is white powder, soluble in methanol, name is17beta-Hydroxyandrost-4-en-3-on or 4-Androsten-17beta-ol-3-on, Chemical Abstracts Service number 58-22-0, ATC code G03BA03. It is a controlled substance, in US by Drug Enforcement Administration . Its inactive epimer difference in configuration of OH at C17 is called epitestosterone. Testosterones biosynthesis starts from cholesterol. Metabolism: up to one tenth of testosterone is converted by 5-alpha reductase to dihydrotestosterone, less than 0.5% by aromatase to estradiol. Most of testosterone is deactivated and excreted as glucoronides.
Figure 1.
Jeffrey Turner Md Prostate Oncology Specialists Marina Del Rey California
Low testosterone , or hypogonadism, is typically encountered by men when they arrive at middle or late stages of life. The symptoms are increased body fat, weight gain, low sex drive, fatigue, anemia, depression, poor memory, osteoporosis, and a higher risk of diabetes. The first step when considering whether testosterone replacement is appropriate is to determine if the cause is primary or secondary. Primary hypogonadism is when the testicles themselves fail to produce adequate amounts of testosterone. Secondary hypogonadism occurs when the pituitary gland stops producing sufficient amounts of LH , the hormonal factor that stimulates the testicles to produce testosterone.
When a diagnosis of primary hypogonadism is made, direct replacement with testosterone is a reasonable course of action. In secondary hypogonadism, men can take medications, such as Clomid, which work by stimulating the pituitary gland to produce more LH, which in turn stimulates increased production of testosterone from the testicles.
Why do we care about the specific methodology of increasing testosterone? Because long-term testosterone replacement can further suppress any residual testosterone production from the testicles, causing testicular atrophy. By stimulating natural production with Clomid, the functionality of the testicles is maintained in a natural state.
Read Also: Immunotherapy For Metastatic Prostate Cancer
How Is Hormone Therapy Used To Treat Hormone
Hormone therapy may be used in several ways to treat hormone-sensitive prostate cancer, including:
Early-stage prostate cancer with an intermediate or high risk of recurrence. Men with early-stage prostate cancer that has an intermediate or high risk of recurrence often receive hormone therapy before, during, and/or after radiation therapy, or after prostatectomy . Factors that are used to determine the risk of prostate cancer recurrence include the grade of the tumor , the extent to which the tumor has spread into surrounding tissue, and whether tumor cells are found in nearby lymph nodes during surgery.
The use of hormone therapy before prostatectomy has not been shown to be of benefit and is not a standard treatment. More intensive androgen blockade prior to prostatectomy is being studied in clinical trials.
Relapsed/recurrent prostate cancer. Hormone therapy used alone is the standard treatment for men who have a prostate cancer recurrence as documented by CT, MRI, or bone scan after treatment with radiation therapy or prostatectomy.
Hormone therapy is sometimes recommended for men who have a “biochemical” recurrencea rise in prostate-specific antigen level following primary local treatment with surgery or radiationespecially if the PSA level doubles in fewer than 3 months.
Testosterone Measurement And Prostate Cancer
Submitted: May 2nd, 2012Published: January 16th, 2013
DOI: 10.5772/52525
There are two ways to cite this chapter:
There are two ways to cite this chapter:
- Medical Faculty, University of Maribor, Maribor, Slovenia
- Division of Urology, Department of Surgery, General Hospital Murska Sobota, Slovenia
*Address all correspondence to: tine.hajdinjak@gmail.com
Read Also: Side Effects Of Brachytherapy For Prostate Cancer
Relationship Between Total Testosterone And Characteristics Of Pca
Patients diagnosed with PCa were separated according to their total testosterone levels based on a cutoff value of 350 ng/dL. No significant difference was found between the cut-off levels for testosterone among high-risk patients regarding Gleason scores, cancerous core involvement rates or the risk stratification according to Damico criteria .
Urological Referrals For Consideration Of Prostate Biopsy And Rates Of Prostate Biopsy And Diagnosed Prostate Cancer
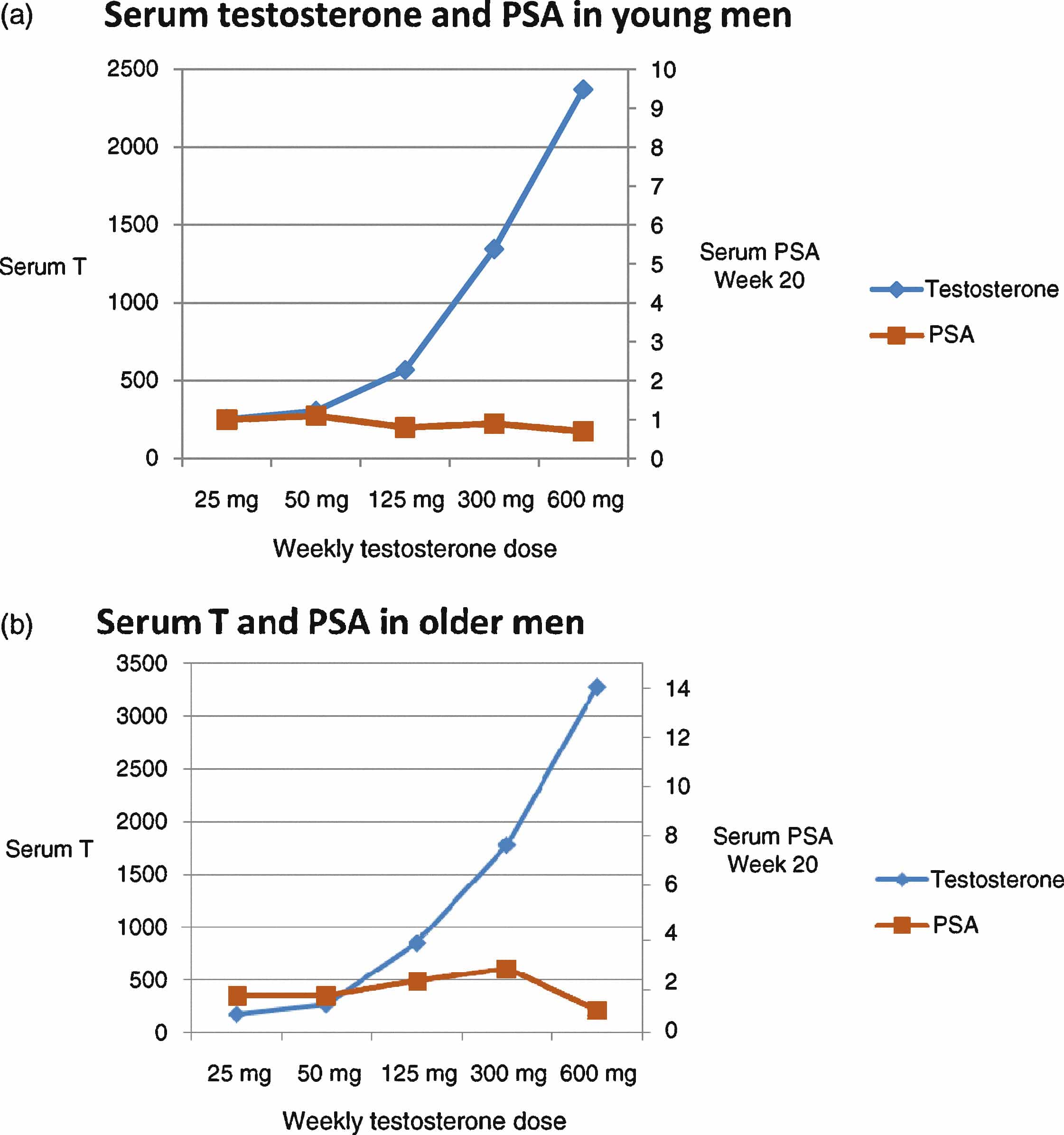
Twenty-six of the 743 men who had at least one postbaseline PSA measurement had a confirmed increase in adjusted serum PSA of > 1.0 ng/mL, and 1 man had a prostate nodule but not an increase in PSA , outcomes mandating referral to a site or personal urologist for evaluation. Twenty-two men were evaluated by a urologist, and 1 man died of a stroke prior to urological evaluation. Six men underwent prostate biopsies. Five of these men had increases in adjusted PSA > 1.0 ng/mL and a PSA > 4.0 ng/mL. The sixth man had a prostate nodule but not an increase in serum PSA. Reasons that the urologists did not perform a biopsy included adjusted PSA increase < 1.0 ng/mL when repeated by the urologist , PSA less than age-related PSA criterion , normal digital rectal examination by urologist , and refusal of biopsy .
Of the four men treated with testosterone who underwent biopsy, three had cancer, two of which were Gleason 4+4 = 8 . Of the two men treated with placebo who underwent biopsy, one had cancer.
Recommended Reading: Vitamins And Supplements For Prostate Health
Don’t Miss: Does Losing Weight Help Enlarged Prostate
Impact Of Raising Testosterone Levels In Men After Radical Prostatectomy
A testosterone challenge approach appears to allow for early detection of prostate cancer recurrence in men with low testosterone after radical prostatectomy , according to a study presented at the 2021 Sexual Medicine Society of North America Fall Scientific Meeting.1
The investigators found that 5 of 22 men who underwent the challenge had a rise in prostate-specific antigen level following testosterone therapy.
Given that PSA secretion is testosterone-dependent, the investigators sought to raise testosterone levels in men who had undergone RP and analyze the effects. This would determine whether low testosterone levels in this group of men were factors in producing artificial, undetectable PSA levels.
Twenty-two patients were evaluated, including men who underwent RP with an undetectable PSA level and a total testosterone level of less than 200 ng/dL. Mean preoperative PSA among this population was 6.2 ng/mL, mean post-RP total testosterone value was 140 ± 35 ng/dL 2.2, median Gleason sum was 7 , mean post-RP pre-challenge testosterone value was 140 ± 35 ng/dL, and mean time from RP to testosterone challenge initiation was 7 ± 9 months.
The investigators found that 5 out of 22 men experienced an elevated PSA level after the testosterone injection, 2 of whom experienced immediate rises of in PSA.
Reference
Related Content:
Drugs That Stop Androgens From Working
Anti-androgens
For most prostate cancer cells to grow, androgens have to attach to a protein in the prostate cancer cell called an androgen receptor. Anti-androgens are drugs that also connect to these receptors, keeping the androgens from causing tumor growth. Anti-androgens are also sometimes called androgen receptor antagonists.
Drugs of this type include:
They are taken daily as pills.
In the United States, anti-androgens are not often used by themselves:
- An anti-androgen may be added to treatment if orchiectomy or an LHRH agonist or antagonist is no longer working by itself.
- An anti-androgen is also sometimes given for a few weeks when an LHRH agonist is first started. This can help prevent a tumor flare.
- An anti-androgen can also be combined with orchiectomy or an LHRH agonist as first-line hormone therapy. This is called combined androgen blockade . There is still some debate as to whether CAB is more effective in this setting than using orchiectomy or an LHRH agonist alone. If there is a benefit, it appears to be small.
- In some men, if an anti-androgen is no longer working, simply stopping the anti-androgen can cause the cancer to stop growing for a short time. This is called the anti-androgen withdrawal effect, although it is not clear why it happens.
Newer anti-androgens
Enzalutamide , apalutamide and darolutamide are newer types of anti-androgens. They can sometimes be helpful even when older anti-androgens are not.
These drugs are taken as pills each day.
Also Check: Metastatic Castration Resistant Prostate Cancer Mcrpc
The Relationship Between Gleason Scores Core Involvement Rates And Testosterone Levels
The two parameters for the aggressiveness of PCa were also evaluated as Gleason score of < 7 or 7 and core involvement of < 50% or 50% in patients with diagnosed PCa according to their mean total, free and bioavailable testosterone levels . Although mean total testosterone levels were comparable, patients who exhibited Gleason score of 7 had significantly lower mean free and bioavailable testosterone levels, evidencing the negative correlation between the aggressiveness of the cancer and blood testosterone levels. However, no significant difference was found between mean total, free and bioavailable testosterone levels and percentage of core involvement .
What Are Male Sex Hormones
Hormones are substances that are made by glands in the body. Hormones circulate in the bloodstream and control the actions of certain cells or organs.
Androgens are a class of hormones that control the development and maintenance of male characteristics. The most abundant androgens in men are testosterone and dihydrotestosterone .
Androgens are required for normal growth and function of the prostate, a gland in the male reproductive system that helps make . Androgens are also necessary for prostate cancers to grow. Androgens promote the growth of both normal and cancerous prostate cells by binding to and activating the androgen receptor, a protein that is expressed in prostate cells . Once activated, the androgen receptor stimulates the expression of specific genes that cause prostate cells to grow .
Almost all testosterone is produced in the testicles a small amount is produced by the adrenal glands. Although prostate cells do not normally make testosterone, some prostate cancer cells acquire the ability to do so .
Also Check: 10 Foods To Avoid For Prostate Health
You May Like: What Happens If Prostatitis Is Not Treated
Testosterone Therapy And Prostate Cancer
Testosterone therapy may increase the risk of prostate cancer recurrence for some people.
Some factors that are particularly associated with a high risk of recurrence:
- Extraprostatic extension
- Positive margins
- Gleason scores of 8 or more on biopsy
- Invasion of the seminal vesicles
There are some situations when testosterone therapy would not be harmful and may be beneficial for people who have had prostate cancer.
- Men who have low-grade or benign tumors
- Men who have completed therapy with surgery or radiation and appear to be cured can use testosterone therapy after an appropriate waiting period between two and five years. The risk of cancer recurrence at this point is generally quite low.
- When a man with known prostate cancer has a low testosterone level and severe physical infirmity or very advanced muscle loss that is associated with notable weakness.
The Dynamic Model And The Effect Of Age On Pca
After the age of 50, the incidence of PCa increases exponentially with age . Prior studies have yielded rich data regarding the age patterns of testosterone. Testosterone levels are increased in pubertal adolescence, then peak between 30-40 years, and subsequently falling thereafter at the rate of 23 % per year . In some men, normal prostate cells develop into tumor cells with age after testosterone level reaches blow a certain level , leading to PCa. Figure illustrates the parallels of PCa development and declining testosterone levels. Studies of age patterns of testosterone levels suggest that only a small proportion of individuals have testosterone levels below the threshold before age 50. Consequently, PCa risk is very low among this young population. However, after age 50, the proportion of individuals with testosterone levels below the threshold increases dramatically with each. As a result, PCa risk also increases exponentially.
Read Also: How Do You Get Your Prostate Checked
When Is Hormone Therapy Used
Hormone therapy may be used:
- If the cancer has spread too far to be cured by surgery or radiation, or if you cant have these treatments for some other reason
- If the cancer remains or comes back after treatment with surgery or radiation therapy
- Along with radiation therapy as the initial treatment, if you are at higher risk of the cancer coming back after treatment
- Before radiation to try to shrink the cancer to make treatment more effective
Dr Thompsons Perspective On Testosterone Replacement
What concerns do you have about prescribing testosterone to men who have been successfully treated for prostate cancer?
Obviously, testosterone supplementation has salutary effects for someone who is hypogonadal and suffering from osteoporosis, muscle loss, erectile dysfunction, and other problems. Unquestionably, otherwise healthy men given the choice of being on testosterone or being off testosterone would rather be on it. So, why not prescribe testosterone supplements to men who are hypogonadal and have been treated for prostate cancer?
Well, imagine two men with prostate cancer. The first man had a 12-core biopsy that showed cancer in just a small percentage of one core, cancer that was graded a Gleason 3 + 3. Hes had several prior biopsies, all of which have been negative, and his PSA is 2.5 ng/ml, which is within the normal range. The second mans biopsy shows cancer in every core on the right side of his prostate, graded a Gleason 5 + 4. The cancer can be felt during a digital rectal exam but is confined to the prostate capsule. Both men have undergone treatment.
How does that happen? Testosterone could reactivate existing disease. Or, if the patient had external beam radiation, not all of the tissue becomes fibrotic. Some normal epithelium, the cell layer that lines the prostate, will persist, and that normal epithelium is at risk of becoming cancerous.
Do you have patients who are on testosterone therapy?
So whats your biggest concern?
About the Author
Don’t Miss: What Is The Color Ribbon For Prostate Cancer
Intermittent Versus Continuous Hormone Therapy
Most prostate cancers treated with hormone therapy become resistant to this treatment over a period of months or years. Some doctors believe that constant androgen suppression might not be needed, so they advise intermittent treatment. This can allow for a break from side effects like decreased energy, sexual problems, and hot flashes.
In one form of intermittent hormone therapy, treatment is stopped once the PSA drops to a very low level. If the PSA level begins to rise, the drugs are started again. Another form of intermittent therapy uses hormone therapy for fixed periods of time for example, 6 months on followed by 6 months off.
At this time, it isnt clear how this approach compares to continuous hormone therapy. Some studies have found that continuous therapy might help men live longer, but other studies have not found such a difference.
Different Roles Of Testosterone In The Onset And Progression Of Pca
To date, no documented epidemiological studies have distinguished testosterone as a cause of PCa from a promotor of PCa growth. One advantage of our dynamic model is that it can be used to assess the role of testosterone in the onset of PCa. As the model suggests, the prostatic carcinogenesis may be a process by which the normal prostate cells first adjust themselves to progressive declining testosterone levels at the cellular and receptor levels. As testosterone levels fall below the threshold when normal prostate cells are not able to make additional adjustments without mutations, some of the normal prostate cells may evolve into cancer cells. If additional testosterone is added before reaching the threshold level, it may change the course of the disease. Among the mutated cancer cells, some of them may become testosterone sensitive and increases in testosterone may therefore promote these cancer cells to grow. This notion is supported by evidence that castration can inhibit PCa progression , while administration of exogenous testosterone can promote PCa progression . Therefore, our dynamic model can also be used to interpret the seemingly conflicted findings that higher testosterone can prevent PCa onset but promote PCa progression after the disease occurs.
Read Also: Best Treatment For Intermediate Prostate Cancer
Also Check: Can Prostate Cancer Be Detected In Blood Test
Testosterone As A Predictor Of Cancer Progression And Biochemical Recurrence
A study by Yamamoto et al. observed 272 localized prostate cancer patients divided into hypogonadal and eugonadal arms. Results suggested that those men who check a low testosterone level prior to radical prostatectomy are much more likely to have a biochemical recurrence than those men with normal testosterone values. The study also found that independent and significant predictors of PSA recurrence were Gleason score, surgical margin status, PSA, and preoperative testosterone.
Dr. Khera argues that there is a utility for checking testosterone during active surveillance . A study by Ignacio et al. followed 154 men with AS for prostate cancer. Out of those men, 54 progressed to AS and had significantly lowered free testosterone levels than those who remained on AS. Notably, free testosterone levels less than 0.45 ng/dL correlated with a sevenfold risk of disease increase.
