#visualabstract: Magnetic Resonance Imaging
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.
Biparametric Mri: A New Standard For Prostate Cancer Imaging
BackA lone and discordant voice supported by few at first, biparametric prostate magnetic resonance imaging has been gradually gaining attention and visibility as a reliable, faster, and cheaper alternative to conventional multiparametric magnetic resonance imaging and could become a new standard of care in the near future.
Strengths And Weaknesses In Relation To Other Studies
PSA-based prostate cancer screening is limited by the lack of a concrete cut-off value and the poor specificity of the test. Although a serum PSA cut-off of 4.0ng/mL has been suggested, as many as 25% of prostate cancers may present with a PSA less than this threshold. Indeed, in the MRI arm of the current trial, 18% of patients with diagnosed with clinically significant prostate cancer had a PSA < 4.0ng/mL. Thus, PSA-based prostate cancer screening lacks both sensitivity and specificity to identify men with aggressive prostate cancer. MRI offers several advantages including sparing biopsy in approximately one-third of patients, greater acceptance of the recommendation for prostate biopsy if the test is abnormal, much higher negative predictive value with targeted biopsy versus standard TRUS-guided biopsy, and the potential for this screening strategy to reduce the over diagnosis of clinically insignificant prostate cancer.
Read Also: What Age Can A Man Get Prostate Cancer
Pilot Study To Examining The Feasibility Of Mri Prostate Cancer Screening
In contrast to previously described approaches, the use of mpMRI in an otherwise unselected population is relatively untested. We recently conducted a pilot study assessing the feasibility of mpMRI as an initial prostate cancer screening test . Following a newspaper based call for volunteers, 319 men agreed to participate in this study. Of these, 120 were eligible, 50 were enrolled due to limitations in funding, and 47 completed the study protocol. Serum PSA testing, mpMRI, digital rectal examination, and systematic prostate biopsies were performed on all men. Prostate cancer was identified in 18 of 47 men . MpMRI significantly outperformed PSA in the prediction of prostate cancer. In multivariable analyses including age, digital rectal examination findings, PSA and MRI score, mpMRI was the only significant predictor for the presence of prostate cancer . These findings were even stronger when we sought to predict only clinically significant prostate cancer .
Why Should I Have An Mri Scan
Consultants usually identify prostate cancer and measure its growth rate using MRI scans although non-problematic cancers are typically found using biopsy. Whenever biopsies detect prostate cancer MRI scans can be used retrospectively and facilitate quicker patient treatment planning and to clarify if and where further biopsy should be taken.
In-depth studies on MRI scanning and the powerful magnetic fields involved have shown no risks to patients, making the procedure one of the safest stages of treatment available. Ongoing global research and development is already producing breakthrough technologies with scanners that can accommodate a patients medical condition or limitation.
Patients can often be accompanied by a close friend or family member throughout their MRI scan listening to music via headphones for the duration is also a popular option. Its important to remember that the MRI procedure is physically painless and any mild discomfort thats experienced during the scan is short-lived and gone the same day.
Read Also: Life Expectancy After Metastatic Prostate Cancer
Risks Associated With Ga 68 Pmsa
The noted a possible risk for misdiagnosis of metastatic prostate cancer by Ga 68 PMSA-11. The tracer may bind to other types of cancer or certain nonmalignant regions, which may lead to errors.
In addition, because Ga 68 PSMA-11 is a radioactive agent, it contributes to a patients overall long-term radiation exposure, which could increase the risk for cancer. However, the risk of developing cancer due to the low radiation exposure by an imaging test is very unlikely, according to the American Cancer Society .
The Role Of Mri In Risk Stratification And Prediction Of Ece And Rp Outcome
MpMRI has demonstrated excellent accuracy in index lesion detection, compared to RP specimens described by recent publications. However, risk group stratification for localized PC, as defined by NCCN criteria incorporates serum PSA-level, the GS of biopsy specimen and the clinical T-stage based on digital rectal examination and lacks formal mpMRI incorporation .
In the 2012 ESUR guidelines a scoring system for extracapsular disease was published, including criteria regarding ECE, seminal vesicle infiltration , adjacent and infiltration of distal sphincter and bladder neck .
Table 3Figure 5
In contrast to clinical parameters like NCCN criteria, prostate MRI offers localized staging and allows the surgeon to sculpt the extent of PC and possible ECE . Another decision-making tool is maximum capsule contact length on MRI. Baco et al. analyzed the predictive value of MRI-determined tumor contact length to the capsule and found a correlation between ECE and tumor contact length of r=0.839 using Spearmanâs regression . Based on ROC curve analysis, the best threshold of MRI determined tumor contact length was 20 mm .
In conclusion, MR imaging can potentially improve the accuracy of the surgeonâs decision to resect or preserve the neurovascular bundle in patients undergoing RP .
You May Like: How Do They Test For Prostate Infection
Potential Advantages Of Mri
Radiologist expertise may also significantly influence the diagnostic characteristics of MRI. In a cohort of 101 patients, Branger et al. showed that a negative MRI could not exclude the presence of clinically significant cancer . However, experienced radiologists can exclude significant volumes of Gleason score â¥7 prostate cancer with a negative predictive value exceeding 95% .
Much of the data supporting the potential role for screening MRI is drawn not from the use of MRI in the screening setting but extrapolation from reports among patients with abnormal PSA test results. Thus, further research is required.
Psma And Mri For Early Prostate Cancer Detection
Lisette HiltonUrology Times Journal
Experts weigh in on whether the combined technologies could be the future power couple of prostate cancer diagnosis.
Prostate-specific membrane antigen and multiparametric magnetic resonance imaging are proving their worth, individually, in the diagnosis and treatment of prostate cancer. But each has its limitations and PSMA use is indicated only for advanced prostate cancer.
Now investigators are asking whether marrying the imaging capabilities of PSMA positron emission tomography and MRI might optimize use of imaging while limiting the need for invasive biopsies.
PSMA has an opportunity to potentially delineate areas of the prostate where the MRI can miss cancer. We know there is no perfect imaging modality that has 100% specificity and 100% sensitivity. So to layer in a PET scan like PSMA with MRI has the potential to find additional tumors. The caveat to this is while it is what we believe and hope to happen, until we have definitive clinical trials that show this, we cannot assume thats the case, said Peter A. Pinto, MD, an investigator and urologic senior surgeon in the Urologic Oncology Branch of the National Cancer Institute, National Institutes of Health, Bethesda, Maryland.
The challenges will be in establishing clinical pathways that allow urologists and others to rely on the accuracy of these tests and understand how to best incorporate them into practice.
Also Check: How Many Prostate Glands Do Males Have
Fda Clears New Ai Software For Mri Detection Of Prostate Cancer
The ProstatID, an adjunctive artificial intelligence software that radiologists can utilize with traditional magnetic resonance imaging , reportedly measures prostate gland volume, and suggests PI-RADS scoring of suspicious lesions.
An emerging artificial intelligence software program that may enhance the efficiency and accuracy of prostate cancer diagnosis has received 510 clearance from the Food and Drug Administration .
Through computer-aided detection , ProstatID offers a colorized translucent overlay of two-dimensional axial T2 magnetic resonance imaging to identify soft tissue lesions that may warrant closer inspection for potential malignancy. The ProstatID algorithm also utilizes the Prostate Imaging Reporting and Data System to score the cancer probability of suspicious lesions, according to Bot Image. The company noted that two internal studies showed improved accuracy and a reduced false positive rate with the use of ProstatID.
While other technologies have enhanced formatting and segmentation of MRI images of the prostate, Bot Image said ProstatID is a significant advance for the diagnosis of prostate cancer.
Bot Image noted that ProstatID is available to radiologists as a software as a service tool, which provides secure, HIPAA compliant connectivity between a cloud-based ProstatID server and a facilitys radiology department server.
Related Content:
Additional Uses Under Investigation
How might this technology be used in the future?
Were working toward performing biopsies directly through MRI guidance, probably by superimposing MRI information onto an ultrasound image. In this way, we could maximize benefits of MRI in identifying areas to target during biopsy, to increase the chances that cancer is sampled.
Many men are undergoing active surveillance, which means that their cancer has been diagnosed, but they are monitoring its progression before undergoing treatment. Have you had any experience with whether MRI could help such men to monitor cancer progression?
Thats another area were studying. But weve already been following individual men, on a case-by-case basis, who are undergoing serial MRIs at Beth Israel Deaconess Medical Center because they are undergoing active surveillance. In some of those patients, weve actually seen the cancer grow in size.
Are there any differential MRI appearances according to the Gleason score of the prostate cancer, as finally determined by pathology?
Don’t Miss: Prognosis For Prostate Cancer That Has Spread To Lymph Nodes
Extended Systematic And Saturation Biopsies
The debate on the optimal number of biopsy core samples that should be taken is still open. Ploussard et al. have demonstrated that an increase from 12 to 21 cores significantly increases the detection rate of significant PC . Transperineal mapping biopsy aims for optimal staging and detection of all significant PC by using an external grid of 5 mm . Lecornet et al. have shown that TPMB detects nearly all significant PC lesions above 0.5 mL . However, TPMB is significantly more invasive than SB leading to urinary retention and the potential for oversampling of clinically insignificant PC, which often results in overtreatment. Valerio et al. report that, beside an accurate index lesion detection, insignificant PC was detected in up to 42.9% of TPMB . Additionally, the prostate is mobile, deformable and swells during biopsy, so real-time sampling errors in vivo might still occur . Thus, Ukimura et al. conclude that the specific clinical indication for TPMB, remains under debate .
Strengths And Limitations Of This Study

-
This is the first randomised trial to directly compare serum prostate-specific antigen testing and prostate MRI for prostate cancer screening purposes.
-
Participants in each arm did not undergo the reciprocal test at the time of randomisation.
-
Limitations of the current study include the conduct of the trial at a single centre and the higher drop-out rate seen in the PSA arm.
-
The study was terminated prematurely due to accrual challenges and difficulties accessing MRI resources and PSA follow-up data due to resource limitations and patient reluctance during the COVID-19 pandemic as a result, the study was underpowered.
-
Nevertheless, this randomised trial confirms the utility and public acceptance of the use of MRI in this setting.
Read Also: Is Zinc Good For Prostate Problems
Could Mri Be The New Answer For Prostate Cancer Screening
Oh, that dreaded prostate exam. Yes, theyre uncomfortable, intrusive, and not at all something you look forward to. In fact, many men will delay a prostate exam for as long as possible, perhaps rescheduling the appointment just to put it off a little longer. This is unwise and can be dangerous, especially for men over 65 who are more likely to develop prostate cancer.
However, physical prostate exams may soon be a thing of the past, as new studies have proven MRI for prostate cancer screening to be quite effective. Men may be able to forego a physical exam in the future in favor of digital imaging, which is often more accurate . It is still unclear whether an MRI can simply replace a prostate-specific antigen test, or replace the entire cancer screening process altogether, but it is exciting to know that men will have access to even more precise diagnoses.
Better screening is needed because PSA testing, which is used when prostate cancer symptoms are present or a mass is detected in the prostate, is not always accurate. Aggressive prostate cancer can go undetected, as well as nonaggressive cancer, which couldve been monitored through simple exams or digital imaging. A lack of early detection can unfortunately lead to more invasive testing.
Statement Of Principal Findings
From this randomised controlled study where patients underwent a stand-alone PSA or prostate MRI test for prostate cancer screening, we found that patients in the MRI screening arm were less likely to be recommended to undergo prostate biopsy . Despite a lower biopsy rate in the MRI group, there was a trend towards higher prostate cancer and clinically significant prostate cancer detection, although this did not reach statistical significance. Further, among the subgroup of patients in the MRI arm who had an end-of-study PSA test, recommendations based on a single screening PSA test would have both potentially missed patients with cancer and conversely, unnecessarily recommended prostate biopsy.
Don’t Miss: How To Detect An Enlarged Prostate
Strengths And Weaknesses Of The Study
To our knowledge, this is the first randomised trial to directly compare serum PSA testing and prostate MRI for prostate cancer screening purposes. A major strength of our study is that each arm did not undergo the reciprocal test at the time of randomisation. More specifically, patients in the MRI arm did not have a PSA test at the time of randomisation. Thus, the potential bias introduced with a PSA test with the MRI could have led to violations in the study protocol with misleading results. The end-of-study PSA tests among patients in the MRI clearly showed how PSA levels could have affected biopsy and cancer detection rates.
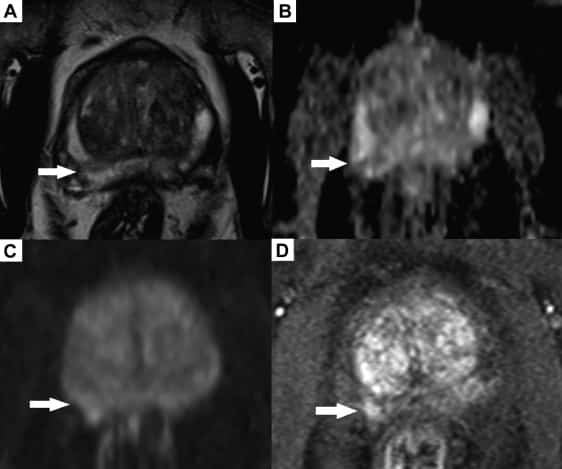
Limitations of the current study include the conduct of the trial at a single centre and the higher drop-out rate seen in the PSA arm. Given the nature of the interventions, blinding was not possible. Biparametric MRI was used in this trial however, bpMRI has been shown to have similar sensitivity and specificity compared with mpMRI and may be more cost-effective. The Siemens Prisma system 1 is one of the highest performance gradient systems for MRI. This can help improve the quality of DWI compared 3T gradient systems used in routine clinical practice. Given MRI interpretation was done by a single experienced reader on a high-performance system, our results may be optimistic if compared with multiplatform and reader performance.
Researchers Awarded 1m To Trial Quicker Diagnostic Tools For Prostate Cancer
13 January 2022
Researchers have been awarded £1 million to trial new MRI scanning methods to diagnose prostate cancer.
The team, from Imperial College London and Imperial College Healthcare NHS Trust, will explore whether a new type of magnetic resonance imaging scan can detect signs of prostate cancer more quickly than current methods. They will also assess whether new imaging technology to help doctors carry out targeted prostate biopsies is better at detecting prostate cancer compared to traditional biopsies. If proved effective, the team hopes the new technology will be more accurate and faster at diagnosing prostate cancer, and they estimate it could save the NHS £15 million per year.
Funded by Cancer Research UK, the work is led by Professor Hashim Ahmed, from the Department of Surgery and Cancer at Imperial College London, who is Consultant Urological Surgeon at Imperial College Healthcare NHS Trust. Prostate cancer is the most common cancer in men in the UK with around 52,300 new cases diagnosed each year. It develops when cells in the prostate grow in an uncontrolled way. Prostate cancer develops slowly and symptoms such as the blood in the urine do not appear until the disease has developed. It usually affects men over 50 and often men with a family history of the disease. Black men are disproportionately impacted by the disease and deaths from prostate cancer have now overtaken those from breast cancer.
Recommended Reading: Early Signs Of Prostate Cancer Symptoms
Distribution Of Tumour And Benign Voxel Values
KolmogorovSmirnov tests showed that data distributions between tumour and benign voxel values for all MRI parameters, both for all tumours and when tumours were separated into high grade and low grade, were significantly different to benign voxel values and could be considered to come from different data distributions.
Figure shows box and whisker plots for selected parameters, comparing the distribution of benign voxel values with low grade and high grade tumour voxel values. The mean DCE MRI parameters Ktrans, IRE, iAUGC60, AUC and ME were higher in tumour than benign tissue, while the mean ADC and DCE MRI parameter TTP were lower in tumours when compared with benign tissue.
Fig. 3
Box and whisker plots showing the distribution of benign, low grade , high grade and all tumour voxel values from T2w, ADC, TTP, IRE, AUC, ME, Ktrans Parker, Ve Parker and iAUGC60
For all high grade tumour models, when Ktrans was included it was the second most important parameter after ADC, ranging from 16 to 30%. The importance of T2w MRI in the RF models was consistently lower than for ADC and decreased with additional DCE MRI parameters. When quantitative or semi-quantitative DCE MRI parameters were included, they contributed between 34 67% in feature importance for the low grade models and between 30 54% for the high grade models.
Psma/mri With Focal Treatment
Research here to improve focal therapy is focused on the belief that in-field cancer recurrence is not due to the type of ablative modality used rather, it has to do with being able to see the tumor and its borders well, Pinto said. PSMA/MRI may help us to better select patients for focal therapy and help guide or follow up patients in that capacity.
Also Check: What To Expect After Your Prostate Biopsy
