Predictable Mri Patterns Help Identify Suspicious Lesions In The Whole Gland
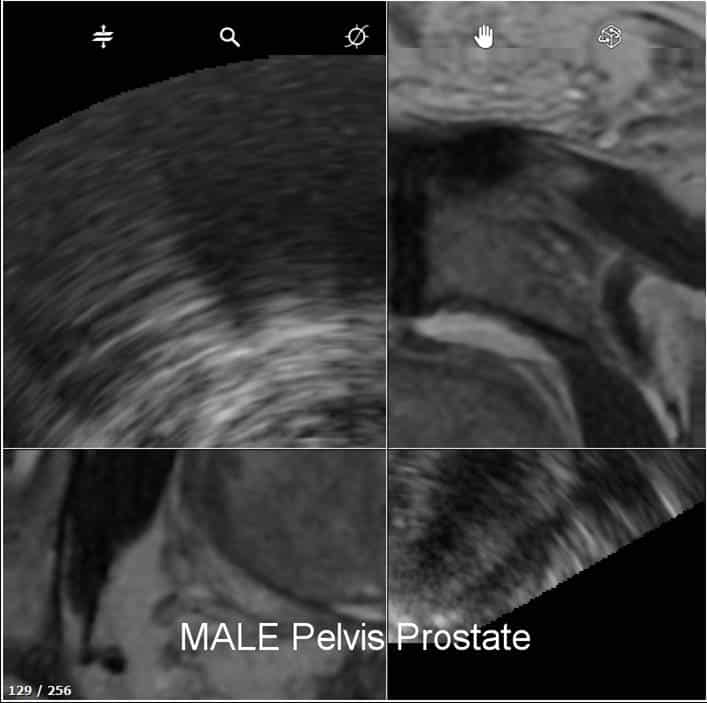
Depending upon the Gleason score and prior therapies, prostate carcinoma has a certain predictable pattern on multiparametric MRI, according to Dr. Steiner. In general, lesions in the peripheral zone have decreased T2-weighted signal and are relatively focal, he says. In the transitional zone, these lesions are more difficult to evaluate on T1 and T2, but are generally non-encapsulated.
We especially look at diffusion-weighted images and the ADC map. Prostate neoplasms generally have diffusion restriction, so they are bright on diffusion-weighted imaging and dark on an ADC map, which is one of the most important characteristics of neoplasms.
The third characteristic we look at, flow, is somewhat less specific but may be quite important in deciding whether a lesion is significant or insignificant. Prostate neoplasms often have a hypervascular tumor flow pattern, meaning that there is rapid inflow of blood into the lesion and then rapid outflow due to a disrupted capillary bed. This can be graphed on multi-parametric images, allowing us to define regions of interest and look at the actual flow within these regions.
I perform this interrogation using DynaCAD prostate, which also provides an easy way to determine PI-RADS score and create the report for the urologist.
What Does An Elevated Psa Mean
The PSA test, which detects the level of prostate-specific antigen in a mans blood, is a valuable screening tool for prostate cancer. While the normal PSA range can vary based on a patients age and other factors, a PSA of 4.0 ng/mL or higher is generally considered abnormal for men over 60. Most cases of an abnormal or elevated PSA result can be attributed to a benign condition, though a PSA elevation can also be an indicator of prostate cancer. The most common causes of an elevated PSA include:
- Inflamed prostate
- Injury or trauma to the prostate
- Prostate cancer
Depending on the degree of elevation, the patients PSA history, the patients risk for prostate cancer, and other factors, further diagnostic testing and/or biopsy may be required to rule out disease. Kasraeian Urology is proud to offer the most advanced prostate cancer screening tools available in Greater Jacksonville, including:
- MRI/US fusion biopsy
Rapid Scanning Time And More Patientcomfort With Elition
Dr. Steiner currently performs all prostate MRI examinations on the Ingenia Elition 3.0T scanner. Previously, our scans were over 45 minutes per patient. However, with Elition and Compressed SENSE we have now decreased our scanning time to approximately 25 to 28 minutes, with more patient comfort, says Dr. Steiner. We have also achieved significantly improved resolution and more consistent parameters for interpretation. VitalEye, VitalScreen and other workflow features all add significantly to the patient experience as well as patient throughput.
You May Like: Can Young Men Get Prostate Cancer
Advanced Magnetic Resonance Mapping Targets Cancer
Using a cutting-edge technique for prostate cancer diagnosis and management, our team at University Hospitals uses MRI mapping to identify the exact location of suspicious tissue. We use images from the MRI to distinguish abnormal tissue from normal tissue. This allows our physicians to more accurately identify prostate cancer tumors and lesions, while also tracking their growth.
Although historically believed that MRI machines couldnt detect cancerous tissue, we now know that MRI images accurately identify aggressive cancers. So, with this knowledge, UH physicians developed the non-invasive fingerprinting technique to map the prostate and help distinguish normal from abnormal prostate tissue.
This breakthrough procedure lets UH physicians also monitor the prostate without making men go through unnecessary biopsies or other invasive examinations. As part of our active surveillance treatment, our team is able to monitor the growth of the tumor and determine if more interventional prostate cancer treatment is needed.
Future benefits may be even brighter: University Hospitals has been awarded a $5 million grant from the National Institutes of Health to further develop MRI mapping and the use of artificial intelligence to predict the likelihood of a cancer diagnosis.
Mri Fusion Prostate Biopsy
New River Urology is pleased to offer the first MRI-Ultrasound fusion prostate biopsy procedure in the Lowcountry.
For almost 30 years, urologists have utilized ultrasound to guide the prostate biopsy procedure. This is essentially a blind technique whereby ultrasound is merely used to ensure that the biopsy needles have hit the prostate. This has led to false negative biopsies in many instances, as well as over detection of slow growing, non-lethal cancers which may not even require any treatment.
Recent advances in MRI technology now allow us to identify potentially lethal cancers that before could not be visualized on ultrasound. We can now offer patients a screening prostate MRI and if a suspicious lesion is found, specifically target that lesion with our biopsy procedure using a fusion ultrasound device. Using this MRI targeted biopsy, the detection rate of insignificant cancers is lower than with systematic blind ultrasound guided biopsy. Further, when MRI findings have been correlated with pathologic findings, tumor localization appears to be significantly better with MRI than with the digital rectal examination or with ultrasound guided blind biopsy, and in the detection of prostate cancer that is clinically significant, MRI appears superior to all other imaging modalities evaluated to date.
Who should have a targeted prostate biopsy?
Our Locations
Read Also: Can You Drink Alcohol With Prostate Cancer
Interpretation And Reporting Of Multiparametric Mri
The magnetic resonance imaging has been used for locoregional staging in patients with proven prostate cancers since the 1980s . The multiparametric protocol has been introduced to discriminate nonmalignant tissue and potentially cancerous lesions. Since its introduction, the field of PCa diagnosis has been revolutionized.
According to the European Society of Urogenital Radiology guidelines, the multiparametric MRI protocol should include three MRI modalities: triplanar T2-weighted sequences, axial diffusion-weighted imaging with apparent diffusion coefficient mapping, and dynamic contrast-enhanced images .
To standardize the evaluation and reporting of prostate mp-MRI examinations, a consensus-based guideline, known as Prostate Imaging Reporting and Data System version 1, was introduced in 2012. Most recently, a revised version of the document was published.
One of the main aims of the PI-RADS v2 document was to develop categories summarizing the levels of suspicion each detected lesion in the prostate gland is assigned a score that goes from 1 to 5. The 5-point scoring, based on the likelihood that MRI findings correlate with the presence of Cs PCa, is defined as follows:
very low risk
intermediate risk
According to PI-RADS v2, a cancer is considered to be clinically significant when Gleason score > 7, and/or tumor volume > 0.5 ml, and/or an extraprostatic extension is diagnosed .
What Are The Advantages Of An Mri
Research has shown that using an MRI image to guide a biopsy improves detection of prostate tumors that require treatment, while finding fewer tumors that are called biologically insignificant. This means that they do not need any immediate treatment and are not likely to pose a threat to the patient. Because using an MRI image gives doctors better information and reduces the chance that a serious tumor will be missed, it should also mean that patients with blood-test results that suggest possible prostate cancer are less likely to need repeat biopsies because the first one may have produced a false negative.
Also Check: What Does A Nodule On The Prostate Mean
We Do Not Need A Rectal Coil With Our Elition 30t System And Its High Quality Gradients Providing High Quality Imaging
Many patients have had prior MRIs, which they disliked, because its noisy, uncomfortable, boring, and the gantry is tight. And invariably, after we scan them in our Elition, most of them say, Hey, this wasnt as bad as I thought it was going to be. I would say that patients are pleasantly surprised that the scan was quicker than theyve experienced in the past the immersive experience is pleasant for them, and the bore seems more open than they remember. The Elition system is definitely a step up in terms of patient comfort and frankly in imaging too.
When asked if he would recommend 3.0T for prostate imaging, Dr. Steiner says: Undoubtedly! When I look back at our prior scans that were done on a 1.5T, then the quality, the conspicuity of lesions and my diagnostic confidence are unquestionably improved with the Elition 3.0T. We had looked at all major vendors and selected Philips, because I thought Philips excels in technology as well as the ability to use ExamCards and the ability to cross-train our technologists.
From Mri To Lesion Segmentation To Biopsy An Efficient Process
For Dr. Steiner, DynaCAD is essential as a diagnostic tool for the interpretation of multiparametric prostate MRI. I have a custom layout that Im comfortable with it allows me to link all of the images and shows the T1, T2, diffusion-weighted images and ADC map on one screen. It also shows me the flow patterns on a second screen so that I can actually cross-link and read all of the images at the same time I just scroll through the depth of the image, says Dr. Steiner. DynaCAD also has a PI-RADS module and I can actually annotate anything I dictate and have that as a report to show to the patient or the urologist.
We generate over 4500 images per case. Not utilizing an automated process would make interpretation quite difficult. Most people interpret prostate MRIs in a zonal manner, so we need a program such as DynaCAD that allows us to look at the flow pattern in basically one dataset.
Also Check: Do Prostate Exams Feel Good
The Day Of The Biopsy
The morning of the exam, take one tablet of Cipro and take two tablets of Keflex. Take another two tablets of Keflex right before your biopsy procedure.Give yourself a Fleet enema, following the instructions on the side of the box.
You may eat a light breakfast and a light lunch before your biopsy, but then must limit your intake to liquids .
One hour before your biopsy, drink two glasses of water. A full bladder enables the physician to see your prostate more clearly.
If you take prescription medications on a daily basis, please take them to day of your biopsy.
Mri/ultrasound Fusion Guided Biopsy For Prostate Cancer
How we detect prostate cancer has changed little in the past 30 years. University of Iowa urologists and Holden Comprehensive Cancer Center experts now offer a new technology to help improve the accuracy of prostate cancer biopsies.
MRI/Ultrasound fusion guided biopsy combines a specialized magnetic resonance imaging scan with an ultrasound image to help urologists precisely target the area of the prostate that needs to be biopsied. This approach allows our doctors to ensure they sample the exact site in the prostate where there is concern for cancer.
Recommended Reading: Nanoknife Treatment For Prostate Cancer
Getting The Results Of The Biopsy
Your biopsy samples will be sent to a lab, where they will be looked at with a microscope to see if they contain cancer cells. Getting the results usually takes at least 1 to 3 days, but it can sometimes take longer. The results might be reported as:
- Positive for cancer: Cancer cells were seen in the biopsy samples.
- Negative for cancer: No cancer cells were seen in the biopsy samples.
- Suspicious: Something abnormal was seen, but it might not be cancer.
If the biopsy is negative
If the prostate biopsy results are negative , and the chance that you have prostate cancer isnt very high based on your PSA level and other tests, you might not need any more tests, other than repeat PSA tests sometime later.
But even if many samples are taken, biopsies can still sometimes miss a cancer if none of the biopsy needles pass through it. This is known as a false-negative result. If your doctor still strongly suspects you have prostate cancer , your doctor might suggest:
- Getting other lab tests to help get a better idea of whether or not you might have prostate cancer. Examples of such tests include the Prostate Health Index , 4Kscore test, PCA3 tests , and ConfirmMDx. These tests are discussed in Whats New in Prostate Cancer Research?
- Getting a repeat prostate biopsy. This might include getting additional samples of parts of the prostate not biopsied the first time, or using imaging tests such as MRI to look more closely for abnormal areas to target.
Prostate cancer grade
Gleason score
What Is An Mri Fusion Biopsy
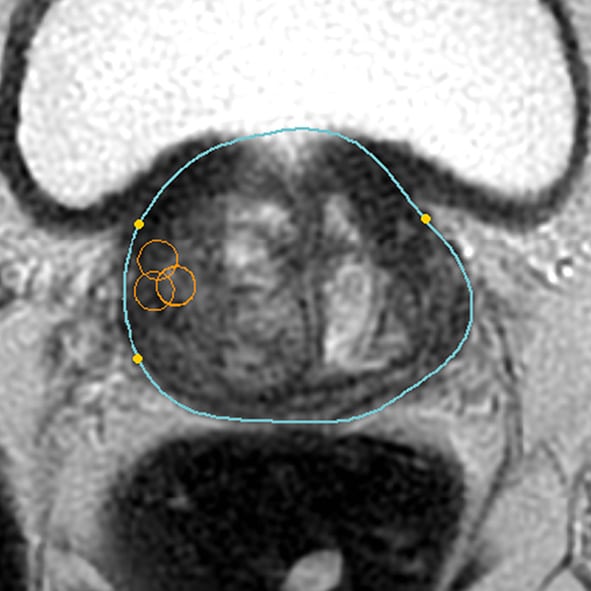
An MRI fusion biopsy is one of the most valuable tools for diagnosing and staging prostate cancer. This advanced procedure combines imaging technology with targeted tissue sampling for ultimate precision and accuracy. During an MRI fusion biopsy in the Jacksonville, FL area, patients will first have an MRI performed to identify the exact locations from which tissue samples should be taken. On the day of the biopsy, Dr. Ali Kasraeian will use ultrasound imaging along with the MRI image results to guide the needle to the precise locations that need to be biopsied.
Read Also: How Long For Prostate Biopsy Results
Summary Of Dr Steiners Experiences:
- High confidence in identifying and segmenting suspicious prostate lesions with multiparametric MRI
- Multiparametric MRI allows visualization of lesions in prostate areas that can hardly be seen via transrectal ultrasound
- Patients needing prostate MRI are directed to 3.0T as the high field strength benefits diagnostic confidence
- Examination time reduced from about 45 min. to about 28 min. thanks to Elition 3.0T with Compressed SENSE and excellent gradient technology
- Patient comfort features and short exam time with Elition are noticed and appreciated by patients
- DynaCAD prostate package allows fast and easy data analysis and PI-RADS score determination, as well as creating well-structured, comprehensive standardized reporting
- Easy transfer of MRI data including segmentation from DynaCAD to UroNav tool for targeted fusion biopsy
- Real-time biopsy guidance by MRI images fused to ultrasound by UroNav probe handling quite similar to TRUS biopsy
- Impressive results seen with MRI/ultrasound fusion biopsies in patients with clinically significant prostate carcinoma that experienced multiple negative TRUS biopsies before
- Entire procedure is reimbursed and the biopsy setup allowed to quickly break even regarding costs
Suspicious Areas Seen On The Mri Can Be Tracked And Targeted During Prostate Biopsy
A new research study at UCLA aims to re-define prostate cancer significance through clinical validation of a tool which allows 3D visualization and tracking of the prostate. By fusing multi-parametric MRI with real-time ultrasound, suspicious areas seen on the MRI can be tracked and targeted during prostate biopsy. This research aims to improve currently available methods of cancer diagnosis.
Video: Targeted Prostate Biopsy using MR-Ultrasound Fusion
Prostate Biopsy: Targeted Prostate Biopsy MR-Ultrasound Fusion at UCLA
Read Also: Rezum Steam Treatment For Prostate
Characteristics Of Enrolled Studies
Out of the 26 enrolled studies, 25 used paired designs and 1 was a RCT. MRI-TB was used in all MRI navigation methods. Six studies included biopsy naïve patients, whereas six studies enrolled participants with prior negative biopsy results. The other studies used mixed biopsy, however, one study did not specify the biopsy type. 23 of the included studies provided clinically significant PCas definition and reported its detection rate. Some articles defined clinically significant PCa based on Gleason score 7 or > 2 positive cores. Some studies used Gleason score with other criteria based on core information . The sample size in each article ranged between 33 and 1042. Patient age ranged from 59 to 70 years. 1.5-T or 3.0-T scanner was used for mp-MRI examination in all included studies. Each patient presented with at least one disputable lesion as shown by MRI results, and each lesion was obtained from at least one targeted core. Systematic biopsies from the same session were carried out using a median of 10 – 13 cores through the transrectal route. Main features of included studies and PCa cases are presented in Table 1. The quality assessment of these enrolled studies is shown in Tables 2, 3 and Figure 2.
Table 1 Clinical characteristics of include studies.
Table 2 Quality assessment according to QUADAS-2 of the included studies.
Table 3 Quality assessment according to Cochrane Collaboration Risk of Bias Tool.
Ucsf Investigators Improve Mr
The accuracy of biopsy sampling, which can miss clinically significant tumors, limits our ability to detect prostate cancer extent and aggressiveness. MRI-guided ultrasound fusion biopsies can improve accuracy, but often the standard-of-care MR images can miss some tumors and are not reliable for determining aggressiveness. Investigators from the Hyperpolarized MRI Technology Resource Center at UCSF set out to study whether hyperpolarized pyruvate MRI can a) detect cancer based on its metabolic reprogramming and b) whether it can assess tumor aggressiveness.
The full team of investigators include Hsin-Yu Chen, PhD, Lucas Carvajal, MS, and Daniel Gebrezgiabhier, from the UCSF HMTRC Dr. Robert Bok, Jeremy Gordon, PhD, John Kurhanewicz, PhD, Peder Larson, PhD, Dr. Michael Ohliger, Daniel Vigneron, PhD, Dr. Z. Jane Wang, UCSF Radiology & Biomedical Imaging and HMTRC faculty Rahul Aggarwal, MD, from UCSF Hematology/Oncology Matthew R. Cooperberg, MD, MPH, Hao Nguyen, MD, PhD, and Katsuto Shinohara, MD, from UCSF Urology and Antonio Westphalen, MD, PhD, from the University of Washington, Department of Radiology.
The goal of the HMTRC is to collaboratively develop new technology to advance this field in order to better identify and understand human disease and ultimately to translate and disseminate these techniques for improved healthcare. Visit our website to learn more about HP MRI resources and Technology Research & Development Projects.
Read Also: What Is Prostate Massage Therapy
What Is A Biopsy And How Effective Is It
A needle biopsy is the only way to diagnose prostate cancer when it is suspected. But there are problems with the method most commonly used, called transrectal ultrasound guided biopsy. These problems often lead to inaccurate diagnosis.
For the last two decades, TRUS biopsy has been used to diagnose prostate malignancy. It is actually a blind and random procedure. Specific prostate tumors, especially very small ones, cannot be identified because ultrasound cannot visually detect specific cancer sites. Therefore, it is blind to tumors. In addition, TRUS biopsies tend to target the peripheral aspects of the gland and are likely to miss 30-40% of prostate cancer located in the anterior, midline transition zone, or apex. This is called sampling error. To attempt to overcome it, TRUS biopsies typically average 12-14 needles saturation biopsies use as many as 24 needles. The more needles used, the greater the risk of discomfort, infection, and urinary or sexual side effects while tumors continued to be missed. No other type of tumor cancer is biopsied this way!
