Heres What The Results Showed
After a median follow-up of just over 10 years, 9.7% of men who were treated with radiation and leuporelin for 18 months had died from prostate cancer, compared to 13.3% of the men treated with radiation and leuporelin for six months. Adding zoledronic acid made no difference in either case.
The authors concluded that hormonal therapy is more effective at preventing prostate cancer death when its given for 18 months rather than six. And similar benefits were noted for other endpoints as well. For instance, prostate tumors were less likely to metastasize, or spread, among men in the longer duration treatment group, and it took longer for their cancers to become resistant to hormone therapy if it was reinitiated later.
In earlier clinical research, scientists discovered that hormonal therapy given for three years protects against prostate cancer death more effectively than a six-month treatment regimen. But three years of hormone therapy isnt easily tolerated, and evidence so far shows that 10-year survival rates after either 18 months or three years of hormonal therapy are similar, the authors of the new study claim.
About the Author
Charlie Schmidt, Editor, Harvard Medical School Annual Report on Prostate Diseases
Beyond Reliance On Androgen Receptors
Doctors treating patients with prostate cancer have long observed that tumors eventually develop resistance to hormone therapy, which disrupts the ability of androgens to help prostate cancer cells survive and grow.
This resistance occurs, it was thought, because prostate cancer cells developed mechanisms to turn these androgen receptor signaling pathways back on, explained Kathleen Kelly, Ph.D., chief of the Laboratory of Genitourinary Cancer Pathogenesis in NCIs Center for Cancer Research, who was not involved in the study.
But since the introduction of the current generation of androgen-suppression therapies, doctors have been reporting that men appear to be developing metastatic tumors that do not rely on androgen receptor signaling, Dr. Kelly added.
To identify molecular pathways that allow prostate cancer cells to survive and grow without androgen receptor activity, Dr. Nelson and his colleagues began their research by using a variety of laboratory techniques to slowly deprive prostate cancer cells of the ability to use androgen receptor signaling.
They expected a type of androgen-independent prostate cancer cell, called neuroendocrine prostate cancer, to develop, explained Dr. Nelson. The development of neuroendocrine prostate tumors has previously been observed in men undergoing long-term hormone therapy.
I think these will be a reference for everybody in the field in terms of thinking about how prostate cancer is changing, commented Dr. Kelly.
Heterogeneity Of Castration Resistance Prostate Cancer
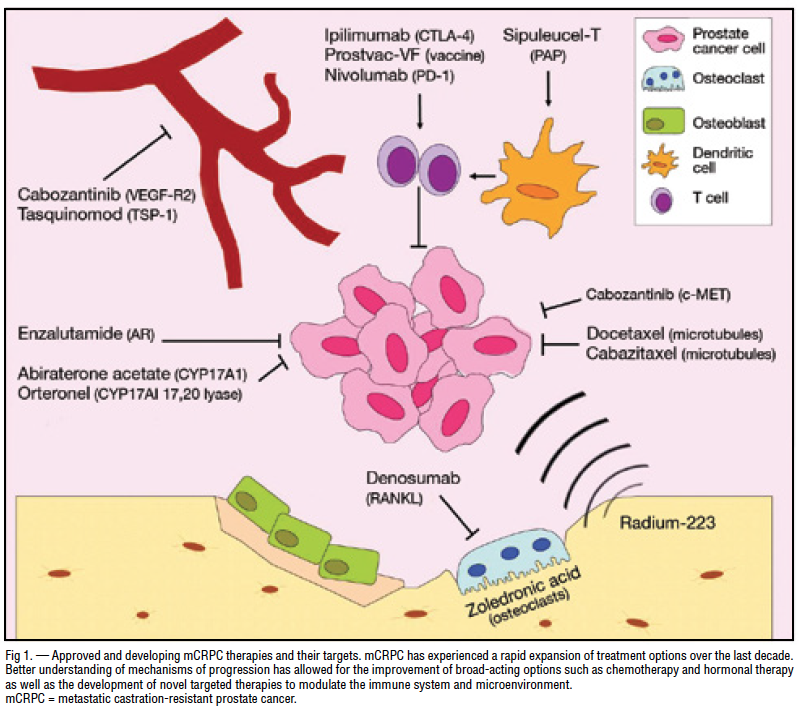
Even though the AR plays a major role in the progression to CRPC, alternative pathways can have a role in stimulating prostate cancer cells, confirming the cellular heterogeneity in prostate cancer .
Prostate cancer cells can develop alternative AR independent molecular pathways for survival that bypass AR activation, including cancer stem cells, receptor tyrosine kinases and neuroendocrine differentiation . A potential mechanism for survival in the castrate environment is the presence of prostate cancer stem cells that continually supply the cancer cell population, despite therapy. These cells are not affected by ADT and can differentiate into androgen dependent and independent cells, leading to a heterogeneous phenotype of AR .
Activation of the PI3 kinase signaling pathway is critical for the survival of prostate cancer cells. PTEN is a tumor suppressor and has lipid phosphatase activity that metabolizes PIP3 . The PTEN function is expressed primarily through negative regulation of the PI3K/Akt pathway. PTEN is inactivated in several types of cancers, including prostate cancer. Loss of PTEN function in prostate cancer can occur through several mechanisms, including deletion, mutation and methylation. These events can cause tumor cell survival through selective pressure caused by ADT .
Don’t Miss: How Fast Does Prostate Cancer Spread
Hormonal Therapy And Chemotherapy In Metastatic Disease
It has been recently demonstrated that the use of chemotherapy can improve outcomes in patients with metastatic hormone naive prostate cancer. It appears that some patients initiating hormonal therapy may actually be better candidates for cytotoxic therapy at this stage of disease than when their disease becomes castration resistant .
It has been controversial as to whether or not early chemotherapy in hormone naive patients would be beneficial. There have been arguments for and against this approach. In favor is the idea that attacking de novo testosterone independent clones early should allow ADT to keep prostate cancer in remission longer. In addition, there is the possibility that some patients at the time of progression may be too frail to receive chemotherapy.
Alternatively, ADT may take cells out of cycle and make them less responsive to cytotoxics. The fact that some patients respond for long periods to ADT and never need chemotherapy is the other argument against early chemotherapy.
Since the early 80s several studies tried to clarify these differing viewpoints, investigating the addition of chemotherapy with hormonal therapy in patients with metastatic prostate cancer .
None of the trials reported positive results, concluding that androgen suppression remains the preferred first line treatment in metastatic prostate cancer and that there was no cytotoxic regimen with consistent activity against hormone-sensitive prostate cancer.
Management Of Advanced And Metastatic Disease
AUA/ASTRO/SUO guidelines on advanced prostate cancer separate management considerations into the following four disease states, which encompass the entire continuum of advanced prostate cancer :
These disease states are defined by the following:
- Primary tumor status
- Presence or absence of distant disease on imaging
- Testosterone levels
- Prior chemotherapy exposure
Read Also: Can You Have Prostate Problems In Your 20s
Physical Emotional And Social Effects Of Cancer
Cancer and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative care or supportive care. It is an important part of your care that is included along with treatments intended to slow, stop, or eliminate the cancer.
Palliative care focuses on improving how you feel during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of cancer, may receive this type of care. And it often works best when it is started right after a cancer diagnosis. People who receive palliative care along with treatment for the cancer often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. You may also receive palliative treatments similar to those meant to get rid of the cancer, such as chemotherapy, surgery, or radiation therapy.
Learn more about the importance of tracking side effects in another part of this guide. Learn more about palliative care in a separate section of this website.
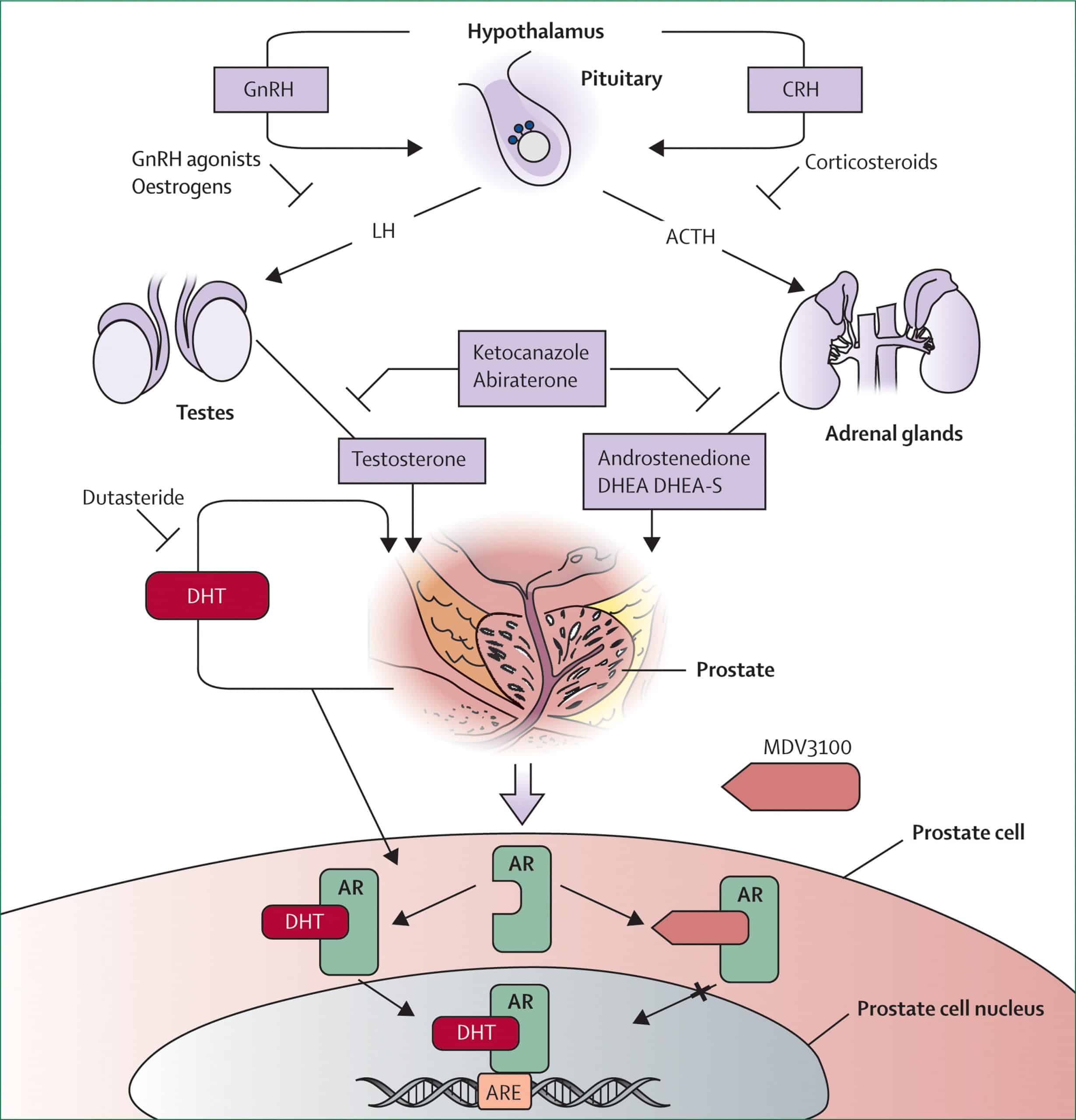
Treatment To Lower Androgen Levels From Other Parts Of The Body
LHRH agonists and antagonists can stop the testicles from making androgens, but cells in other parts of the body, such as the adrenal glands, and prostate cancer cells themselves, can still make male hormones, which can fuel cancer growth. Some drugs can block the formation of androgens made by these cells.
Abiraterone blocks an enzyme called CYP17, which helps stop these cells from making androgens.
Abiraterone can be used in men with advanced prostate cancer that is either:
- Castration-resistant
This drug is taken as pills every day. It doesnt stop the testicles from making testosterone, so men who havent had an orchiectomy need to continue treatment with an LHRH agonist or antagonist. Because abiraterone also lowers the level of some other hormones in the body, prednisone needs to be taken during treatment as well to avoid certain side effects.
Ketoconazole , first used for treating fungal infections, also blocks production of androgens made in the adrenal glands, much like abiraterone. It’s most often used to treat men just diagnosed with advanced prostate cancer who have a lot of cancer in the body, as it offers a quick way to lower testosterone levels. It can also be tried if other forms of hormone therapy are no longer working.
Ketoconazole also can block the production of cortisol, an important steroid hormone in the body, so men treated with this drug often need to take a corticosteroid .
Recommended Reading: Can Prostate Cancer Return After Radical Prostatectomy
Rationale For Treating Nmcrpc
Progression of nmCRPC to metastatic disease is likely to involve lymph nodes and/or bone approximately one-third of patients will develop osseous metastasis within 2 years, most commonly involving sites in the pelvis, spine, or ribs . Among patients with nmCRPC, a higher PSA concentration at diagnosis, shorter PSADT, higher Gleason score, a history of primary intervention, and a shorter interval from ADT initiation to the diagnosis of CRPC, have been associated with shorter time to metastasis . It is generally accepted that poor prognosis of patients with nmCRPC is most closely suggested by shorter PSADT . Following the development of metastases, the prognosis for OS diminishes .
Patients with bone metastases are at significant risk of developing symptomatic skeletal events history of an SSE is considered a negative predictor of survival . The association of SSEs with mortality might be explained by the presence of advanced disease, declining performance status, loss of independence, and pathological fractures . While SSEs cause pain and adversely impact quality of life, their management is associated with significant healthcare resource utilization, which has been found to be consistent in global, multinational studies .
Use Of Hormone Therapy In Treating Prostate Cancer
Hormone therapy is used in several ways, and androgen deprivation in prostate cancer may be given using either medication or surgery. This prostate cancer treatment may be used to:
- Cause the testicles to produce less androgen
- Block androgens from doing their job throughout the body
- Block the body from producing androgens
Hormone therapy is often used for different stages of prostate cancer, including in men with low, intermediate and high risk of cancer growth and spread. This treatment is generally used:
- In cancers that have spread too extensively to be treated with radiation therapy or surgery
- In patients with pre-existing health conditions that prevent them from undergoing surgery or radiation therapy
- In cancers that recur after initial treatment or that werent completely removed by surgery or radiation therapy
- To help reduce a tumors size to make it easier to remove surgically
- For patients with a high risk of cancer recurrence
Don’t Miss: Can You Feel Prostate From Outside
Hormone Therapy Can Cause Side Effects
Because hormone therapy blocks your bodys ability to produce hormones or interferes with how hormones behave, it can cause unwanted side effects. The side effects you have will depend on the type of hormone therapy you receive and how your body responds to it. People respond differently to the same treatment, so not everyone gets the same side effects. Some side effects also differ if you are a man or a woman.
Some common side effects for men who receive hormone therapy for prostate cancer include:
Chemotherapy Treatment In Crpc
Systemic chemotherapy is one of the options for the treatment of metastatic CRPC. Taxanes represent the class of chemotherapeutic agents that have shown a benefit in terms of overall survival. In particular, docetaxel and recently cabazitaxel have become the currently standard first and second-line chemotherapy agents for the treatment of metastatic prostate cancer patients after ADT failure .
SWOG 99-16 and TAX327 trials are the most important randomized studies showing the benefit of chemotherapy with docetaxel in metastatic prostate cancer.
In the TAX327 trial, 1,006 patients were randomized to receive docetaxel plus prednisone or mitoxantrone 12 mg/m2 every 3 weeks plus prednisone. This trial demonstrated a significant improvement in overall survival in the patient group treated with every 3 weeks docetaxel compared to mitoxantrone, leading also to an advantage in other secondary endpoints such as pain and quality of life .
Despite the efficacy of taxanes in CRPC, the real benefit can vary according to the clinical setting and host factors. Clinical resistance often occurs and can be explained by various mechanisms. Some of these are the presence of p-glycoprotein or other drug transporters that impair the uptake of the drug, the presence of tubulin mutations or the overexpression of the III tubulin isotype that impairs the binding to -tubulin and the presence of AR mutations or splice variants that do not require microtubule-based transport .
You May Like: Cancer Of The Prostate Gland
New Treatments For Nmcrpc
Guidelines for treatment of CRPC that has not yet spread emphasize careful monitoring for possible development of metastases via imaging and measuring blood levels of a protein called prostate specific antigen , a marker of prostate cancer progression. PSA doubling time , the amount of time it takes for PSA levels to double, is a good predictor of cancer progression. If PSADT is longer than 10 months, patients can continue to be observed and continue treatment with ADT. If PSADT is less than 10 months, patients should receive, in addition to the ongoing ADT, a drug that curbs androgen signaling, such as apalutamide, darolutamide, or enzalutamide to try and stave off development of metastases.
Of those three drugs, apalutamide is a newer option. In the pivotal SPARTAN trial, the median metastasis-free survival time for nmCRPC patients who took apalutamide alongside standard ADT was 40.5 months, compared to 16.2 months for patients who received a placebo alongside ADT.
In short, there has been significant evolution in the development of new drugs to treat CRPC, especially mCRPC, and patients are encouraged to explore treatment options available in clinical trials. For more information on any of the treatments discussed in this article, and how to access them, I invite you to get support from Cancer Commons.
Early Evidence Regarding Combinations Of Parp Inhibitors With Standard Mcrpc Therapies
There is conflicting evidence supporting the use of PARP inhibitors in mCRPC patients without mutations in DNA repair genes. The potential utility of PARP inhibitors in this setting will likely only be in combination with another effective agent. Preclinical studies have shown that inhibiting the androgen pathway can induce cell sensitivity to PARP inhibition, suggesting a synergy between androgen pathway blockade and PARP inhibitorsforming the hypothesis of multiple clinical trials . Ongoing phase 2/3 controlled clinical trials investigating PARP inhibitors in mCRPC with or without the concurrent administration of another agent have been summarized .
Table 1 Ongoing phase 2/3 controlled trials investigating PARP inhibitors in mCRPC
Don’t Miss: What Is Bipolar Transurethral Resection Of The Prostate
How Are Treatments Administered
GnRH agonists are either injected or placed as small implants under the skin. Anti-androgens are taken as a pill once per day. Degarelix is given as an injection. A chemotherapy drug called docetaxel is sometimes used in combination with these hormone therapies.
Zytiga is taken by mouth once per day in combination with a steroid called prednisone.
Surgery to remove the testicles can be done as an outpatient procedure. You should be able to go home a few hours after an orchiectomy.
How Does Hormone Therapy Work Against Prostate Cancer
Early in their development, prostate cancers need androgens to grow. Hormone therapies, which are treatments that decrease androgen levels or block androgen action, can inhibit the growth of such prostate cancers, which are therefore called castration sensitive, androgen dependent, or androgen sensitive.
Most prostate cancers eventually stop responding to hormone therapy and become castration resistant. That is, they continue to grow even when androgen levels in the body are extremely low or undetectable. In the past, these tumors were also called hormone resistant, androgen independent, or hormone refractory however, these terms are rarely used now because the tumors are not truly independent of androgens for their growth. In fact, some newer hormone therapies have become available that can be used to treat tumors that have become castration resistant.
You May Like: Problems Caused By Enlarged Prostate
Drug Sequencing For Androgen
The availability of the above new agents presents a challenge for physicians and patients, who must decide on the best sequence and timing for each of them. So far, no studies have been done to determine the best approach. Studies in progress are likely to result in some change to the sequencing of these drugs.
As of October 2012, and excluding cost considerations, men with asymptomatic or minimally symptomatic progressive disease can start with immunotherapy using sipuleucel-T. Since no objective responses are expected, patients can then be given abiraterone acetate.
On September 11, 2014 the FDA expanded the approved use of enzalutamide for the treatment of men with late-stage , castrate-resistant prostate cancer prior to receiving chemotherapy. The expanded indication was based on a study in which patients who received enzalutamide reduced the risk of radiographic progression or death by 83% versus placebo, while significantly reducing the risk of death by 29%.
Without formal studies to guide recommendations, either drug may be used next, although enzalutamide does not require prednisone, and for that reason it may be most suitable. Hopefully, studies will be done to determine whether men are better off receiving either enzalutamide or abiraterone first or second. Men showing progression on those drugs should then be offered docetaxel followed by cabazitaxel.
For full discussion, see Metastatic and Advanced Prostate Cancer.
The Importance Of Starting Treatment Promptly
Numerous cancer studies show that effective anticancer therapies work better against smaller tumors than larger ones. Why is this? First, as the number of cancer cells increase the odds increase that the cancer will mutate into more malignant, treatment-resistant forms. The other issue relates to the immune system. The immune system is constantly battling to inhibit cancer growth, but cancer cells have ways to suppress the normal activity of the immune system. When tumors grow larger, the cancers capacity to have an inhibitory effect on the immune system increases.
Don’t Miss: Does The Prostate Affect Erectile Function
