Role Of Multiparametric Mri In Prostate Biopsy
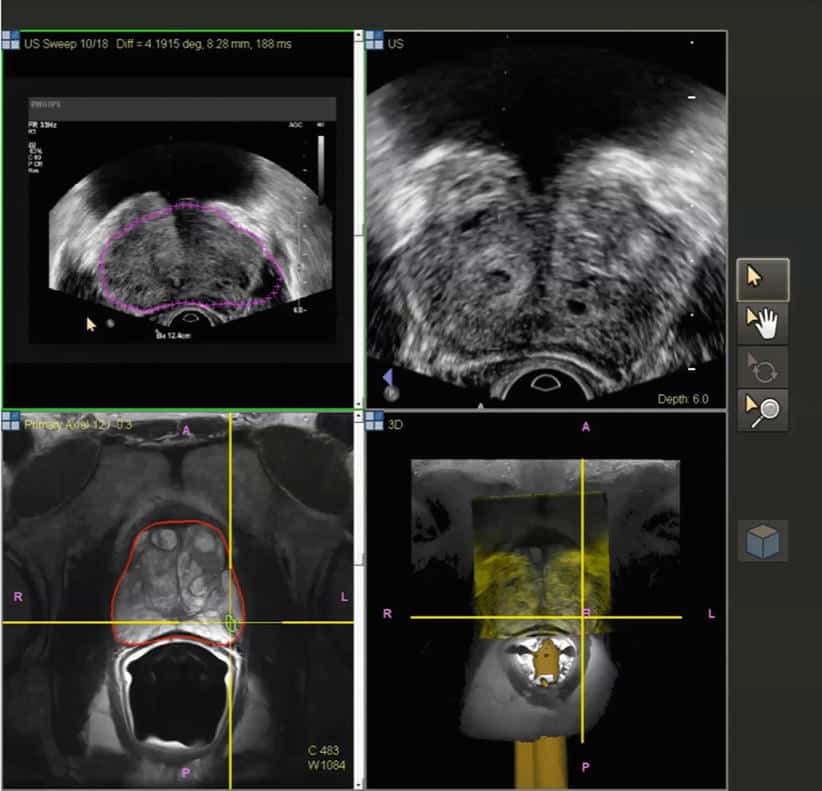
Recent advances in imaging techniques including multi-parametric MRI have enabled non-invasive assessment of the prostate for suspicious lesions. mpMRI is a MRI technique that involves conjunctive use of multiple MRI sequences to more accurately characterize lesions.10 mpMRI reporting has been standardized by the European Society of Urogenital Radiology through the development of the Prostate Imaging Reporting and Data System , which was updated to version 2 in 2015. Park et al. demonstrated in a retrospective study of patients who underwent both mpMRI and radical prostatectomy that PI-RADS2 score greater than 4 was 77% and 73.8% sensitive for detection of clinically significant cancer for each of the two readers with excellent inter-reader agreement.11 A recent meta-analysis by Woo et al. assessing the diagnostic performance of PI-RADS2 included 3857 patients and found a pooled sensitivity of 89% and specificity of 73% for cancer detection.12 Lesions with PI-RADS2 scores of 4 or 5 indicate a high or very high likelihood of clinically significant cancer, respectively, and should be biopsied.13
Currently, the AUA suggests that mpMRI-based screening should be considered purely investigational and awaiting results of PROMIS and PRECISION trials before making a statement on the change in adoption,20 but it will be intriguing to see how rapidly it will change clinical practice.
The Digital Rectal Exam
The prostate gland comprises three zones. Most cancers originate in the peripheral zone. Proctologists, urologists, and oncologists are trained to feel this area while performing a digital rectal exam .
Here, digital doesnt refer to technology. Instead, it refers to the fingers . In a DRE, your doctor inserts a well-lubricated gloved finger gently into the rectum to reach the prostate. Prostate enlargement and suspicious lesions may be felt during a DRE.
How A Prostate Mri Vs Biopsy Can Improve Detection
The good news is that early prostate cancer detection means clinically significant prostate cancer can be highly curable. However, such prostate cancers, if left untreated, have a slow, steady, and predictable behavior with the potential for local tumor progression and spread. Fortunately, detection rate improves with radiology technologies like an MRI, including the multiparametric MRI.
Unfortunately, men usually have to first get a prostate biopsy before their health insurance will cover a prostate MRI with IV contrast. This is backwards because a prostate biopsy has notable risks . Conversely, a prostate MRI is non-invasive and therefore less risky.
Don’t Miss: Can Prostatitis Cause Blood In Your Urine
Mpmri Shows If A Biopsy Is Needed
Its encouraging that noninvasive imaging after a suspicious PSA result can clarify whether a prostate biopsy is justified. Avoiding an unnecessary procedure spares a man from needless risk, and it has the added economic benefit of sparing society from spending needless healthcare dollars. Men whose mpMRI was negative for significant PCa but whose PSA remains high or continues to rise can have repeat scans without the risks involved in repeat biopsy. If the scan reveals significant PCa, a real-time mpMRI-guided targeted biopsy reduces the risks of conventional TRUS biopsy by using fewer needles while it offers the advantages of superior diagnostic accuracy.
Wouldnt it be great to know if you really needed a biopsy? Isnt it great to know that mpMRI tells you what you need to know?
NOTE: This content is solely for purposes of information and does not substitute for diagnostic or medical advice. Talk to your doctor if you are experiencing pelvic pain, or have any other health concerns or questions of a personal medical nature.
Ma X, Wang R, Long JB, Ross JS et al. The Cost Implications of Prostate Cancer Screening in the Medicare Population. Cancer. 2014 Jan 1 120: 10.1002/cncr.28373. Venderink W, van Luijtelaar A, van der Leest M, Barentsz JO et al. Multiparametric magnetic resonance imaging and follow-up to avoid prostate biopsy in 4259 men. BJU Int. 2019 Nov 124:775-784. doi: 10.1111/bju.14853. Epub 2019 Jul 23.
What Is A Trus Biopsy
This is the most common type of biopsy in the UK. The doctor or nurse uses a thin needle to take small samples of tissue from the prostate.
Youll lie on your side on an examination table, with your knees brought up towards your chest. The doctor or nurse will put an ultrasound probe into your back passage , using a gel to make it more comfortable. The ultrasound probe scans the prostate and an image appears on a screen. The doctor or nurse uses this image to guide where they take the cells from. If youve had an MRI scan, the doctor or nurse may use the images to decide which areas of the prostate to take biopsy samples from.
You will have an injection of local anaesthetic to numb the area around your prostate and reduce any discomfort. The doctor or nurse then puts a needle next to the probe in your back passage and inserts it through the wall of the back passage into the prostate. They usually take 10 to 12 small pieces of tissue from different areas of the prostate. But, if the doctor is using the images from your MRI scan to guide the needle, they may take fewer samples.
The biopsy takes 5 to 10 minutes. After your biopsy, your doctor may ask you to wait until you’ve urinated before you go home. This is because the biopsy can cause the prostate to swell, so they’ll want to make sure you can urinate properly before you leave.
Recommended Reading: How Many Stages Of Prostate Cancer Are There
Possible Harms From Treatment
The most common treatments for prostate cancer are surgery to remove the prostate and radiation therapy.
The most common harms from prostate cancer treatment are
- Urinary incontinence . About 1 out of every 5 men who have surgery to remove the prostate loses bladder control.
- Erectile dysfunction . About 2 out of every 3 men who have surgery to remove the prostate become impotent, and about half of men who receive radiation therapy become impotent.
- Bowel problems, including fecal incontinence and urgency . About 1 out of every 6 men who has radiation therapy has bowel problems.
> > > This Simple Morning Test Will Fix Your Prostate
Another type of prostate issue is chronic prostatitis, or chronic pelvic pain syndrome. This condition causes pain in the lower back and groin area, and may cause urinary retention. Symptoms include leaking and discomfort. In severe cases, a catheter may be required to relieve the symptoms. If the problem is unresponsive to other treatments, your doctor may suggest a surgical procedure. If these do not work, your symptoms could progress and become chronic.
An acute bacterial infection can cause a burning sensation. Inflammation of the prostate can affect the bladder and result in discomfort and other symptoms. This is the most common urinary tract problem in men under 50, and the third most common in men over 65. The symptoms of acute bacterial prostatitis are similar to those of CPPS. Patients may experience a fever or chills as a result of the infection.
Don’t Miss: When Should A Man Go For A Prostate Exam
A Picture Is Worth A Thousand Tests
I want to share a retrospective study out of the well-respected Radboud University Medical Center, Nijmegen, the Netherlands. Our Dutch colleagues specialize in clinical studies involving 3T multiparametric MRI for the detection, diagnosis and image-guided treatment of prostate tumors. This study is an important contribution in how to reduce the number of unnecessary biopsies.
In order to determine whether mpMRI results can help avoid an unnecessary biopsy, they analyzed the records of 4259 patients who had mpMRI between Jan. 2012 Dec. 2017. The patients either had a previous TRUS-guided biopsy that was negative for PCa, or had never had a biopsy. The PI-RADS classification system was used to score the probability of PCa . For purposes of their analysis, negative mpMRI was defined as an index lesion of PI-RADS score lesser than or equal to 2 , while clinically significant PCa was defined as Gleason score 3 + 4. Follow-up was completed through Oct. 2018.
According to their mpMRI findings, 2281 patients had a lesion scored as PI-RADS 2. In 320 of them, a follow-up mpMRI was performed at an average of nearly 5 years . The rate of freedom from clinically significant prostate cancer was 99.6% after 3 years. They concluded that more than half of the men were able to avoid a biopsy because their initial mpMRI did not show clinically significant PCa, and 3 years later 99.6% of them had not progressed any further.
Controversies And Misconceptions Surrounding Prostate Biopsies
The PSA test measures the levels of PSA proteins in the body, and when it was first developed, it was quickly implemented by many physicians as a screening test for prostate cancer. The thought was that since PSA proteins are only produced by the prostate, elevated levels could be an indication of prostate cancer. As a result, most men with an abnormal PSA test underwent a prostate biopsy.
The increase in biopsies resulted in the number of advanced, untreatable prostate cancers decreasing significantly because more prostate cancers were caught earlier, when the disease is easier to treat. But the problem with many patients being diagnosed sooner was that some patients were being aggressively treated when they should have been monitored instead.
Though many in the field of urology believe it was flawed, a controversial study attempted to assess the benefits of the PSA test as a screening tool for prostate cancer, and its results led to the recommendation that most men shouldn’t get the test because it didnt appear to improve mortality rates from prostate cancer. This, combined with growing awareness that many cases of prostate cancer were being treated unnecessarily or prematurely, led to a reduction in prostate biopsies. This controversy led to a reduction in prostate cancer screening and an increase in the number of diagnoses of advanced prostate cancer.
Also Check: How To Prevent Enlarged Prostate
Biochemical Recurrence Without Metastatic Disease After Exhaustion Of Local Treatment Options
Biochemical recurrence is defined as a rise in PSA to 0.2 ng/mL and a confirmatory value of 0.2 ng/mL or greater following radical prostatectomy, or a rise of 2ng/mL or more above the nadir PSA after radiation therapy. Not all men who have a rising PSA will develop metastases, and for that reason not all such men require treatment. The risk of metastases and death depend on the patients Gleason score, the length of time between the nadir PSA and the onset of the PSAs rise, and the PSA doubling time.
Patients who have PSA failure following radical prostatectomy and have no evidence of metastatic disease have the options of watchful waiting, radiation therapy, or hormone ablation as salvage therapy. Similarly, patients who have PSA failure following radiation therapy have the following options:
- Watchful waiting
- Hormone ablation
The pretreatment Gleason score, clinical stage, PSA level, and percentage of positive core biopsy results have been found to be reliable predictors of failure following local therapy. Unfortunately, no means of identifying recurrences limited to the pelvis is reliable. Although a Gleason grade of 7 or less is associated with a better prognosis than a grade of 8 or more, the survival likelihood associated with a rise in the PSA level is greater if the rise occurs more than 2 years after local treatment than if it occurs less than 2 years afterward.
How Does Laser Focal Therapy Compare To Other Focal Methods
In comparison to another popular focal treatment methods like high-intensity focused ultrasound , laser focal therapy is not limited to only small glands and has demonstrated much higher levels of accuracy with lower risk of side effects such as, erectile dysfunction.
High intensity focused ultrasound uses ultrasound instead of laser to heat the tissue. To obtain the ablation diameter of the laser used in our approach, HIFU would require > 20 overlapping ablations. What if the patient moves a little and the device misses a spot? When treating cancer, its important to get all of it. The vast majority of HIFU centers use ultrasound guidance , losing the precision of MRI and the important real-time information that MRI thermometry provides in protecting vital structures. Studies show significant urinary and sexual problems after HIFU because important tissues and nerves can be damaged during the procedure.
Laser focal therapy boasts many benefits for patients compared to other treatment methods for prostate cancer. No general anesthesia is required for the therapy, and patients are able to return to work as early as the day after the operation. Additionally, laser focal therapy carries lower risk of side effects compared to other treatment methods such as, impotence, and urinary incontinence. Laser focal therapy also does not rule out the exploration of further treatment options such as surgery or radiation therapy if needed later.
*Results may vary
Read Also: What Does An Enlarged Prostate Mean
Use In Men Who Might Have Prostate Cancer
The PSA blood test is used mainly to screen for prostate cancer in men without symptoms. Its also one of the first tests done in men who have symptoms that might be caused by prostate cancer.
PSA in the blood is measured in units called nanograms per milliliter . The chance of having prostate cancer goes up as the PSA level goes up, but there is no set cutoff point that can tell for sure if a man does or doesnt have prostate cancer. Many doctors use a PSA cutoff point of 4 ng/mL or higher when deciding if a man might need further testing, while others might recommend it starting at a lower level, such as 2.5 or 3.
- Most men without prostate cancer have PSA levels under 4 ng/mL of blood. Still, a level below 4 is not a guarantee that a man doesnt have cancer.
- Men with a PSA level between 4 and 10 have about a 1 in 4 chance of having prostate cancer.
- If the PSA is more than 10, the chance of having prostate cancer is over 50%.
If your PSA level is high, you might need further tests to look for prostate cancer.
To learn more about how the PSA test is used to look for cancer, including factors that can affect PSA levels, special types of PSA tests, and what the next steps might be if you have an abnormal PSA level, see Screening Tests for Prostate Cancer.
Physical Emotional And Social Effects Of Cancer
Cancer and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative care or supportive care. It is an important part of your care that is included along with treatments intended to slow, stop, or eliminate the cancer.
Palliative care focuses on improving how you feel during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of cancer, may receive this type of care. And it often works best when it is started right after a cancer diagnosis. People who receive palliative care along with treatment for the cancer often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. You may also receive palliative treatments similar to those meant to get rid of the cancer, such as chemotherapy, surgery, or radiation therapy.
Learn more about the importance of tracking side effects in another part of this guide. Learn more about palliative care in a separate section of this website.
Don’t Miss: Can A Biopsy Spread Prostate Cancer
Screening Tests For Prostate Cancer
The main screening test for prostate cancer is the prostate-specific antigen test. Its a blood test that measures how much PSA is in your blood. And you will probably have a digital rectal exam. A high PSA level may mean that you have an enlarged prostate, an infection or, less often, prostate cancer.
The prostate-specific antigen test can help find prostate cancer early. But experts recommend that you discuss the benefits and risks of the test with your doctor before you decide whether to have this test. It may not help you live any longer than if you had no screening. And it could lead to harmful treatments that you dont need.
Talk with your doctor about your health, your risk factors for prostate cancer, and the pros and cons of PSA testing.
Dr Niti Shares A Few Things About Psa
PSA is a Glyco protein secreted by prostate cells. It is not a cancer-specific marker. A total PSA more significant than ten ng per ML has a 67% likelihood of being diagnosed as cancer on biopsy. PSA between 4 and 10, there is a 20% likelihood of prostate biopsy being positive. But PSA is also increased due to infection, instrumentation like cystoscopy, TURP, or trauma. Certain drugs like finasteride or dutasteride can reduce the value of PSA. Also, ketoconazole or certain herbal medicines can reduce the value. It is mandatory to discuss the pros and cons with the patient before advising serum PSA.
- There is a concept of stage migration, and early PSA assessment can increase longevity due to early cancer diagnosis.
- PSAV is PSA velocity measured over three different values in 18 months.
- Unbound or free PSA as a ratio of total PSA is also an approved method.
- DRE, as a stand-alone test, has limited value.
Read Also: Best Cancer Center For Prostate Cancer
Prostate Biopsy In Clinical Practice
The decision to proceed with biopsy is complex, evolving, and should be made on an individualized basis. Traditionally, biopsy is performed for three general indications: abnormal digital rectal exam , increased prostatic-specific antigen , and clinical suspicion of prostate cancer.
Prior to the advent of PSA screening, prostate biopsy was performed solely for lesions palpable on DRE.2 Concerning findings on DRE include nodularity, asymmetry, or diffuse firmness. DRE has a poor positive predictive value for detecting cancer 3 and is not recommended as a sole screening tool. However, detection of suspicious gross abnormality on DRE may be an indication for biopsy regardless of PSA depending on contextual patient factors.4
PSA is an important biomarker that correlates with the risk of prostate cancer. Screening for prostate cancer using PSA has been shown to reduce prostate cancer mortality, but its utility is highly age dependent. The American Urological Association provides guidance on who should be screened using PSA. Their recommendations include avoiding screening altogether in men under the age of 40, average risk men age 4054, men age 70 or older and men with a life expectancy less than 1015years. They recommend that for men aged 5569, the decision to screen using PSA should be shared amongst the physician and patient and that a biennial interval may preserve the benefits of annual screening while reducing overdiagnosis.5
