Questions To Ask Your Doctor Radiographer Or Nurse
- Will I have a planning session at a different time to the treatment, or immediately before?
- Will I have external beam radiotherapy or hormone therapy as well?
- What side effects might I get?
- How will we know if the treatment has worked?
- What should my PSA level be after treatment and how often will you test it?
- If my PSA continues to rise, what other treatments are available?
What Are Prostate Seed Implants
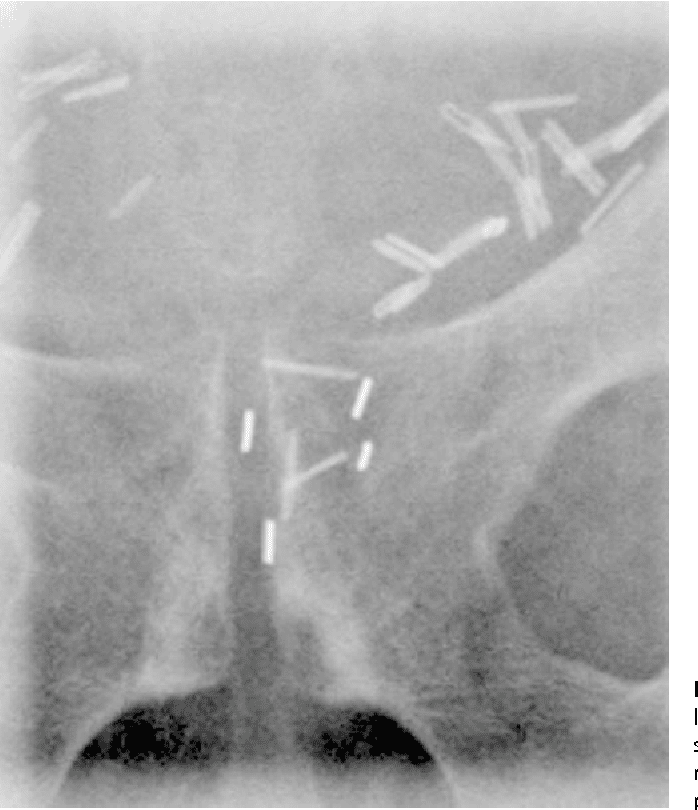
Seed size comparison. Image courtesy of the Nuclear Regulatory Commission .
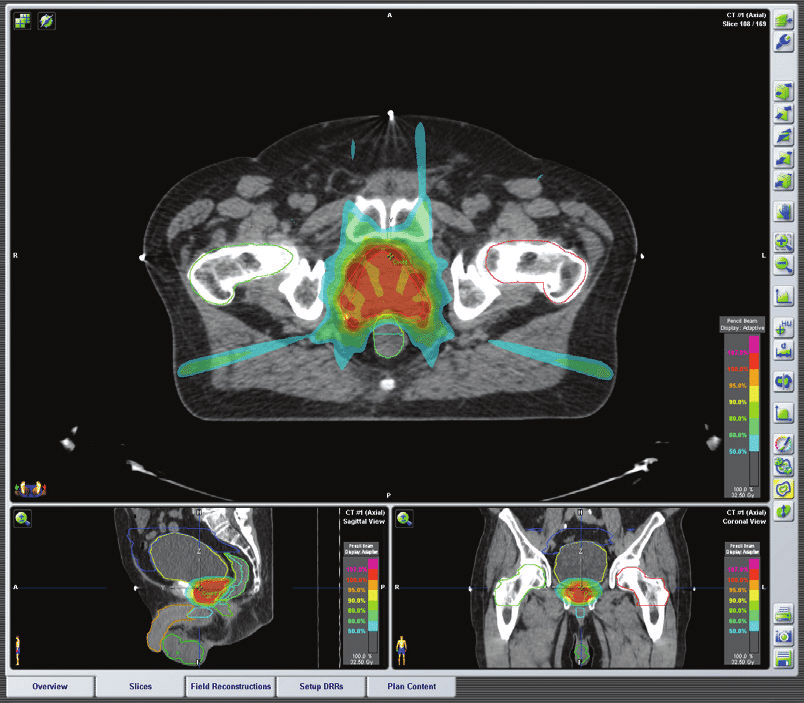
Brachytherapy can be used to treat prostate cancer in the form of prostate seed implants. During this procedure, your doctor will place 80 120 small radioactive seeds into your prostate. This procedure may be performed on an inpatient or outpatient basis depending on the individual.
Over the next few months, the seeds release radiation into the prostate gland and shrink the tumor. The radiation from the seeds wears off over time, leaving the seeds inert. The seeds will not be removed following the procedure.
Brachytherapy may be used on its own or with another type of treatment.
Permanent Versus Temporary Brachytherapy
In addition to permanent brachytherapy, temporary brachytherapy has also been used. In this technique, the implants deliver radiation to the prostate at a higher dose rate than is provided by a permanent implant. Currently, the isotope most commonly used for temporary brachytherapy is iridium -192, which provides a higher dose of radiation than the iodine -125 and palladium -103 permanent implants.
For high-dose-rate brachytherapy , a preplan is devised using TRUS to deliver 15 Gy/h to the prostate and smaller doses to the urethra and rectum. During the implantation, hollow needles are inserted transperineally and checked via TRUS to ensure reproduction of the preplan template. The needles are then connected to an automated remote-controlled loading machine. This device successively moves Ir-192 wires into the needles to the dwell positions for various durations. The total irradiation time is usually only 5-10 minutes.
HDRB is commonly delivered in 2 or more fractions of 810 Gy or more, with 6-24 hours between treatments. Patients require hospitalization while the implants remain in place but may go home once the implants are removed.
HDRB is usually used in combination with IMRT. The optimal patient population has not yet been determined. Most series reported are from single centers.
The American Brachytherapy Society has published consensus guidelines for high-dose-rate prostate brachytherapy, which note a growing experience with the use of this modality as monotherapy.
Recommended Reading: How Do Men Get Prostate Cancer
What Happens During The Radioactive Seed Implant Procedure
The entire procedure takes about 90 minutes. Most patients go home the same day.
A radiation oncologist and urologist perform the procedure. Both doctors are actively involved in all aspects of the implantation, from the planning to the post-operative care. During the procedure, the urologist provides ultrasound guidance and the radiation oncologist places the radioactive seeds. The prostate ultrasound and treatment planning are both done at the same time as implantation of the radioactive seeds.
The procedure
After The Implant Surgery

Most patients are discharged three to four hours after the implant procedure. Occasionally, a patient may need to be observed in the hospital until the next day. Your urologist will determine when you will be discharged from the hospital.
You will be given specific instructions about your implant. Keep these instructions so you can share them with your family members or with any doctors you see after your implant. The instructions will answer any questions you may have about radiation exposure to your family and friends after the implant. They are the same precautions that the radiation oncologist discussed with you.
There is little discomfort after the implant. Some patients do experience mild soreness when they sit. This soreness may last for one or two days after the implant. Sometimes, a patient will notice small spots of blood on his underwear after the procedure. This comes from the spot where the needles were inserted and should stop within 24 hours. Applying mild pressure with a clean cloth will stop the spotting. You may notice a small amount of blood in your urine. This is normal and should stop within one to two days after the implant. If the blood in your urine lasts more then two days, or if you see clots, call your urologist.
You should avoid heavy lifting or hard, physical activity for the first two days that you are home. After that time, you may return to your normal activity level.
You May Like: How To Get Rid Of Prostate Cancer
For Prostate Seed Implantation Trust Experience And Skill
The outcome of implantation is highly operator-dependent. As such, it is important for the radiation oncologist to be experienced and proficient with this procedure. The physicians of Princeton Radiation Oncology are among the most experienced and have been instrumental in pioneering this treatment option.
Will I Be Radioactive During Or After Internal Radiation Treatment
With internal radiation therapy, your body may give off a small amount of radiation for a short time.
If you have a temporary implant, youll be asked to stay in the hospital and might have to limit visitors during treatment. You also may be asked to stay a certain distance away from them. Pregnant women and children might not be allowed to visit you. Depending on the type of implant, once it is removed, your body will likely no longer give off radiation.
Over a few weeks to months, permanent implants will slowly stop giving off radiation. The radiation usually doesnt travel much farther than the area being treated, so the chances that others could be exposed to radiation is very small. Still, your health care team might ask you to take certain precautions such as staying away from small children and pregnant women, especially right after you get the implants.
Read Also: Prostate Cancer Types And Treatment
Read Also: How Accurate Is Mri In Diagnosing Prostate Cancer
What Happens Before The Procedure
A transrectal ultrasound is done to provide the radiation oncologist with specific details about your case. Newer techniques using a CAT scan or MRI may be used to guide the proper placement of the implants. This information is used to custom-design the treatment plan for you. Another option is for the ultrasound and treatment plan to be done at the same time as the radioactive seeds are implanted.
How Long Has This Procedure Been Around
Using internal radioactive sources to treat cancer is not a new concept it emerged over 100 years ago. However, radioactive seed localization specifically is a relatively new technique the first procedure in the Ottawa Hospital Radioactive Seed Localization Program was on April 21, 2015. Our hospital was the third centre in Canada to have this program, and we are a leader in the procedure, with other healthcare centres looking to us for guidance.
Also Check: How Is A Prostate Exam Conducted
What Are The Advantages And Disadvantages
What may be important to one man might be less important to someone else. Your doctor, nurse or radiographer can help you choose the right treatment for you. Theres usually no rush to make a decision, so give yourself time to think about things.
Advantages
- Recovery is quick, so most men can return to their normal activities one or two days after treatment.
- It delivers radiation directly into the prostate, so there may be less damage to surrounding healthy tissue, and a lower risk of some side effects.
- You will only be in hospital for one or two days.
- If your cancer comes back, you may be able to have further treatment.
Disadvantages
- It can cause side effects such as urinary and erection problems.
- You will usually need a general or spinal anaesthetic, which can have side effects.
- It may be some time before you know whether the treatment has been successful.
- You will need to avoid sitting close to pregnant women or children during the first two months after treatment.
If you are having external beam radiotherapy or hormone therapy as well as permanent seed brachytherapy, think about the advantages and disadvantages of those treatments as well.
Preparing For The Implant
Two or three weeks before your implant surgery, your urologists staff will call you to schedule you for routine blood work and a chest x-ray. It is important to have these done promptly, since your seeds have been ordered.
Be sure to tell your doctor if you take aspirin, aspirin products, or blood thinners, such as coumadin®. Your doctor will instruct you on when to stop taking these medications before your surgery.
Your urologists staff will give you instructions regarding what you may eat and/or drink the day before your implant surgery. You will also be given instructions on the use of a laxative and/or enema. A nurse from the Same Day Surgery Department will call you the afternoon before the day of your surgery. The nurse will go over your instructions and will tell you where to park and when and where to report. Please plan to have a friend or family member come to the hospital with you on the day of your surgery, because you will not be able to drive home.
Also Check: Does Ejaculation Help Prostate Inflammation
When You Might Have Permanent Seed Brachytherapy
Permanent seed brachytherapy is a treatment for early stage prostate cancer. This means the cancer hasn’t spread outside of the prostate.
If your prostate gland is too big you might need hormone therapy for 3 months before the radiotherapy treatment. The hormone therapy shrinks the prostate and makes it easier to put the seeds into the right place.
Brachytherapy Prostate Seed Implant
Patients who want to pursue brachytherapy as first line monotherapy, meaning alone and without other treatments, should exhibit these characteristics:
- No history of benign prostatic hyperplasia
- Prostate gland volume below 60 grams or 60 cc
Not meeting all of these criteria, however, does not eliminate brachytherapy as a prostate cancer treatment option. Read on to see who else is opting for brachytherapy and why. Then speak with your doctor to see if brachytherapy is right for you.
Brachytherapy as Initial Monotherapy for Prostate Cancer Prostate cancer should be confined to the prostate for those considering interstitial radiation therapy. This treatment is most effective when the disease is confined within the cloud of radiation created by the radioactive pellets. In most patients, the cloud of radiation will extend about 5 mm outside the organ.
Patients who want to pursue brachytherapy as their primary treatment should have Gleason scores of 6 or less and PSA scores of 10 or less. They should also have prostate volumes which are below 60 grams or 66 cc. Those with benign prostatic hyperplasia are not candidates for prostate brachytherapy. The urinary side effects associated with brachytherapy are exacerbated if the patient already has BPH.
Read Also: What Are The Side Effects Of Radiation For Prostate Cancer
Side Effects Are Part Of All Types Of Prostate Radiotherapy
A common misconception among prospective patients is that prostate implantation has fewer side effects than external beam radiation therapy. Nearly all patients suffer from some urethritis . Urinary retention requiring a temporary catheter occurs in 5% of patients.
To learn more about prostate seed implantation to treat prostate cancer, or to schedule a consultation, call . You can also reach us using our easy online form.
Also Check: Can Psa Test Detect Prostate Cancer
What Type Of Technology Does This Treatment Use
We use real time, 3-dimensional imaging to carefully place each seed at a predetermined location and depth. In this way, we cover the entire gland and the cancer site. The number of seeds implanted into your prostate will depend on your unique anatomy.
We place an ultrasound probe in your rectum to image the prostate. We also use continuous X-ray imaging. Together, these provide a magnified, 3D view of your prostate during the procedure. After the implantationand while you are still anesthetizedwe will check your urethra and bladder and retrieve any seeds found in your bladder.
Read Also: Can Prostate Problems Cause Burning Urination
Are There Side Effects Of The Combination Approach To Prostate Cancer Radiation Therapy
When it comes to early stages of disease, patients very frequently do well with either brachytherapy or external beam radiation. Success rates of around 90% or higher can be achieved with either approach. When the disease is somewhat more advanced based on the PSA level, Gleason score, extent of visible disease on magnetic resonance imaging we have learned over the years that higher doses of radiation are critical to achieving better results. Some evidence, including a large trial, suggests that for patients with intermediate- or high-risk prostate cancer, a combined approach using brachytherapy along with external beam radiation may be best compared to standard dose external beam radiation therapy alone.
Also Check: Super Beta Prostate Supplement Side Effects
What Is Our Seed Implant Technique Why Is It So Important
To have optimal results from your prostate seed implant, it is essential that all areas of the prostate are covered with seeds, and that no sensitive areas outside the prostate are implanted. With our teams technique and experience, there is minimal risk of placement of needles or seeds too close to the bladder, rectum, urethra or nerves. Any motion of the prostate or change in its size or shape during the procedure can be immediately taken into account, ensuring perfect seed placement. Because seeds are precisely placed in the prostate, the risk of seeds migrating outside the prostate is less than 0.4%.
You May Like: How Many Stages Of Cancer Are There In Prostate Cancer
What Are The Side Effects Of Hormone Therapy For Prostate Cancer
Because androgens affect many other organs besides the prostate, ADT can have a wide range of side effects , including:
- loss of interest in sex
Studer UE, Whelan P, Albrecht W, et al. Immediate or deferred androgen deprivation for patients with prostate cancer not suitable for local treatment with curative intent: European Organisation for Research and Treatment of Cancer Trial 30891. Journal of Clinical Oncology 2006 24:18681876.
Zelefsky MJ, Eastham JA, Sartor AO. Castration-Resistant Prostate Cancer. In: Vincent T. DeVita J, Lawrence TS, Rosenberg SA, eds. DeVita, Hellman, and Rosenbergâs Cancer: Principles & Practice of Oncology, 9e. Philadelphia, PA: Lippincott Williams & Wilkins 2011.
Smith MR, Saad F, Chowdhury S, et al. Apalutamide and overall survival in prostate cancer. European Urology 2021 79:150158.
How Many Hospital Appointments You Might Have
You might have the treatment during 1 or 2 stages. This depends on what is available at your hospital.
1 stage procedure
If you have the 1 stage procedure you have your brachytherapy planning and treatment on the same day. And you might stay in hospital for a night afterwards.
You’ll also have an ultrasound scan a few weeks before treatment to check you’re suitable for treatment and to work out how many seeds you need.
2 stage procedure
Some hospitals do your planning 2 to 4 weeks before your brachytherapy. At the planning session you have an ultrasound to check how many seeds you need in your prostate.
Then at your second visit your doctor puts in the radioactive seeds. This is called a 2 stage procedure.
You May Like: How To Check For Prostate Cancer At Home
Case For Combined Treatment
For treatment to be effective in patients who have more aggressive or advanced stages of prostate cancer, it must be directed at both the prostate and the surrounding areas where cancer cells may have spread. To accomplish this, a seed implant is typically combined with a few weeks of IGRT and/or a temporary hormone blocking medicine.
The seed implant delivers a high dose of radiation to the prostate, where most or all of the cancer cells reside. The IGRT not only treats the cancer in the prostate, it also attacks cancer cells that may have spread outside the prostate.
Permanent Seed Brachytherapy For Prostate Cancer
Permanent seed brachytherapy is when your doctor puts very small radioactive metal seeds into your prostate gland. The seeds slowly release a low level of radiation into the area of the prostate over a few months. It is a type of internal radiotherapy.
With brachytherapy, your doctor puts the radioactive source or seeds as close to the cancer as possible. So that the cancer gets a high dose but nearby tissues and further away the levels of radiation are low.
Recommended Reading: What Contributes To The Successful Treatment Of Prostate Cancer
Radioactive Seed Implant: After Your Treatment For Prostate Cancer
This handout explains radioactive seed implant treatment for prostate cancer. Included is what to expect during and after the implant procedure, radiation safety precautions, side effects, and follow-up visits at the Urology Clinic and Radiation Oncology.
The health education materials accessed through this site are not a substitute for professional medical advice, diagnosis, or treatment.Always seek the advice of your doctor or other healthcare provider with any questions you may have about a medical condition.
If you think you have a medical emergency, call your doctor or 911 right away.
Results With Prostate Brachytherapy: 12
At Northwest Hospital, 229 patients with stage T1/T3, low-to-high Gleason grade prostate cancer underwent prostate implants with I-125 or Pd-103 between January 1, 1987 and September 1, 1989. Patients, whose median age was 70 years , were divided into two groups based exclusively on clinical stage and Gleason grade. Pretreatment PSA measurement was obtained in all patients but did not impact upon the treatment group assignment.
Group 1 consisted of 147 lower stage/grade patients treated with an implant alone and Group 2 comprised 82 patients deemed to have higher risk of extra-prostatic extension of the malignancy. Group 2 patients, in addition to receiving a seed implant, were also treated with 45 Gy external beam radiation to the pelvis . None of the patients underwent operative staging, and none received concurrent androgen manipulation.
Fourteen patients were lost to follow-up: Seven by death from non-cancer causes within 18 months post-implant, and seven because of incomplete PSA follow-up, leaving 215 patients for complete evaluation. The median duration of post-treatment follow-up was 110 months.
The observed disease-free survivals of the two groups combined at 12 years was 70% 66% in the monotherapy group and 79% in the combination therapy group. Figures , , and show the disease-free survival results graphically.
Don’t Miss: How Do Prostate Problems Start
