Radioactive Isotope Seed Offers Aggressive Option For Treatment Of Prostate Cancer
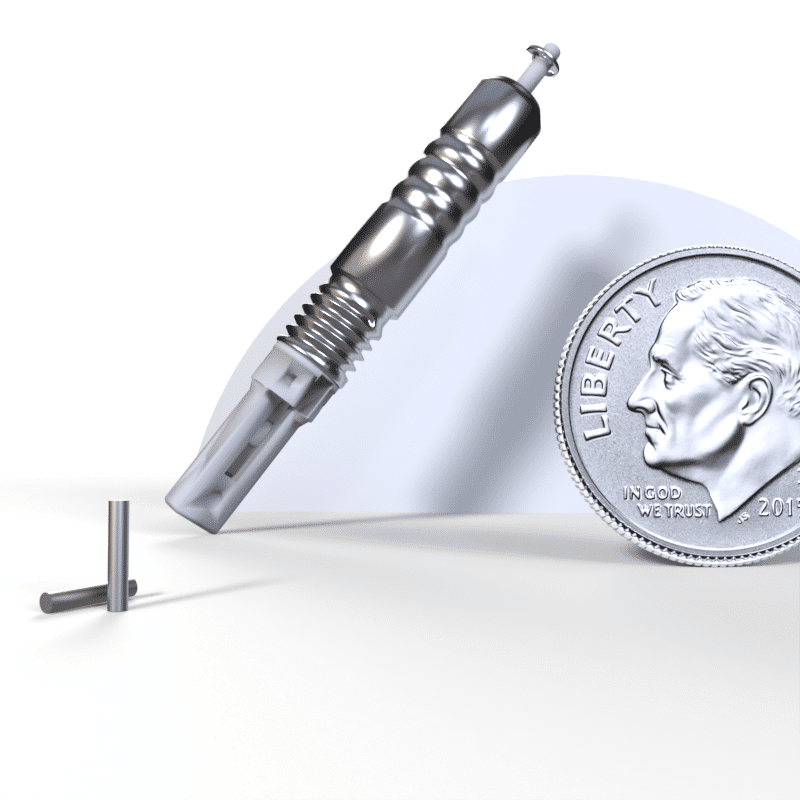
Richland, WA – Radioactive”seeds” have been used to cure thousands of cases of prostate cancersince first used some 40 years ago.
IsoRay Medical, Inc. is producing a powerful new kind of radioactive,cancer-destroying isotope seed made from Cesium-131 that is implanteddirectly into tumors.
Cesium-131 delivers its therapeutic radiation faster than otherisotope seeds now being used and at reduced risk to patients whencompared to surgery. Introduced in September 2004, the clinical use ofcesium-131 marks the biggest advancement in seed brachytherapy since the introduction ofpalladium-103 19 years ago.
The Food and Drug Administration approved Cesium-131 formarketing in March 2003. Its initial use has focused on prostatecancer, but it is approved for other malignant cancers, includinghead, neck, breast, brain, and liver cancers.
Patients at leading cancer treatment hospitals and clinics acrossthe United States are now receiving Cesium-131. The centers forMedicare and Medicaid Services have established a specificreimbursement code for Cesium-131, and most insurance companies alsocover the cost of the brachytherapy procedure.
Cesium-131 differs from other brachytherapy treatments in severalways:
The treatment of prostate cancer is an obvious first applicationfor IsoRay Medical’s Cesium-131 technology. Seed therapy is a provenand common treatment for this form of cancer, with 50,000 to 60,000procedures conducted each year.
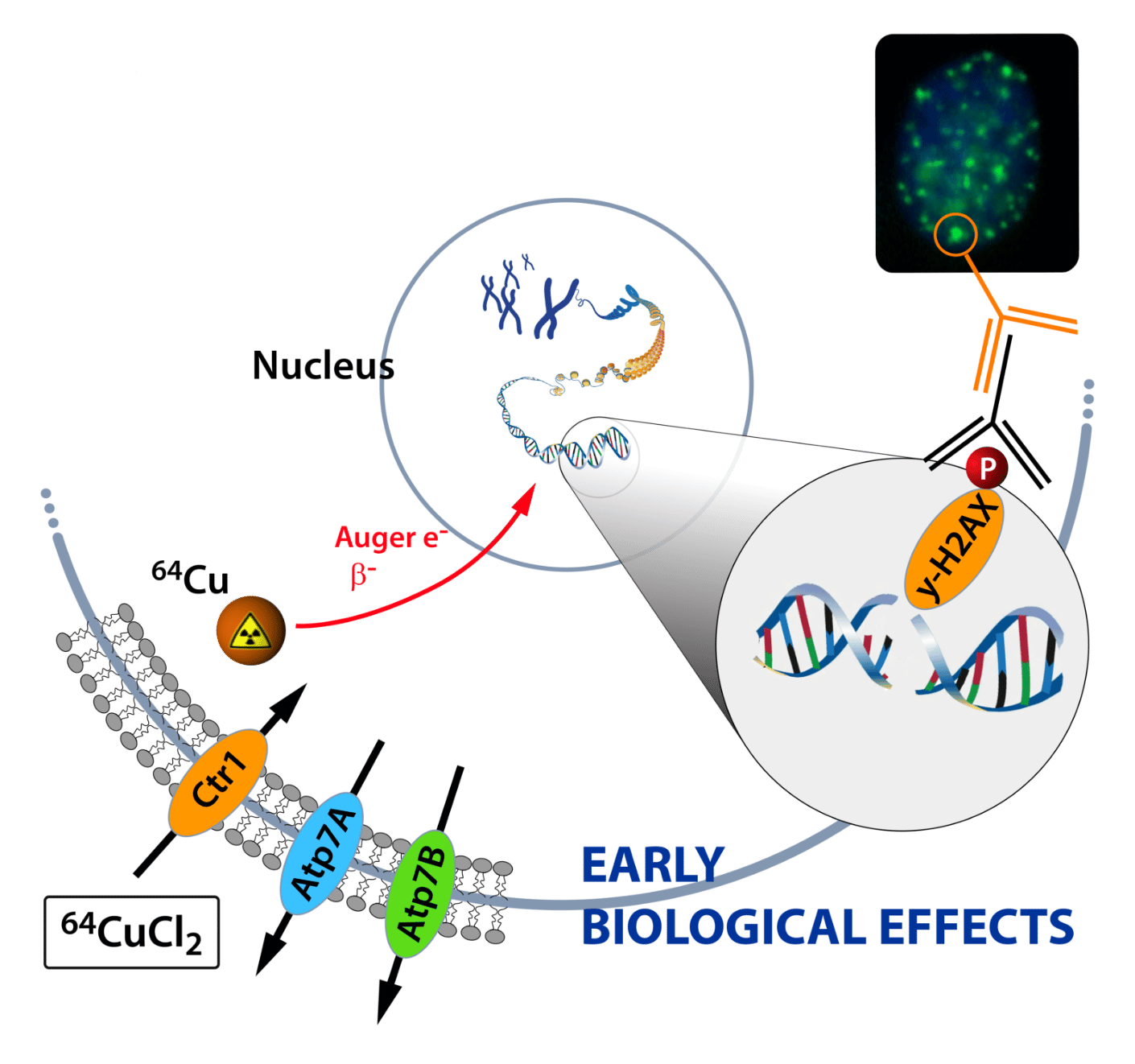
Prostate Cancer Isotope Treatment With 177lu
One of the most common treatments for cancer is external beam radiation therapy. It is possible to deliver radiation directly to the tumour using radioactive isotopes that are administered either orally or by injection.
177Lu-PSMA therapy allows the simultaneous treatment of the tumour and its metastases, regardless of location. Radioisotope therapy is repeated 4 or more times at 6-8-week intervals. Before 177Lu-PSMA therapy, several blood tests and examinations must be performed, which will be prescribed by your doctor. Before coming to the hospital on the day of your treatment, eat a normal breakfast and drink plenty of water .
You will be admitted to the hospital for at least one night. During this time, several images are taken of your body with a gamma camera to assess the distribution of 177Lu-PSMA in your body.
After the end of the therapy, you can leave the hospital and continue as normal. Over the next 2-3 days, it is important to drink plenty of fluids to protect the kidneys and allow the remaining radioactive substance to be cleared faster from the body. When you leave the hospital, the staff will give you written instructions on how to safely interact with others after radiation therapy.
For more information about the therapy, see patient information.
Radioisotopes In Prostate Cancer
Radioisotopes directed to the bone remodeling system have previously been utilized in diagnostic imaging of osseous metastases. The most used radioisotope in this regard has been technetium-99 methylene diphosphonate bone scintigraphy. Newer modalities such as sodium fluoride positron emission tomography and 18-fluorodeoxyglucose PET have also demonstrated promise. A natural extension of this application has been for therapeutic purposes, particularly in prostate cancer due to the predilection of bone-only metastases. A number of randomized trials have demonstrated the efficacy of radioisotopes although their application has been mostly in the palliative setting. Agents used in a therapeutic setting against metastatic prostate cancer include strontium-89, samarium-153, rhenium-186, and rhenium-188, and most recently, Ra-223. The physical characteristics of these agents are shown in Table 1.
Don’t Miss: How To Cure Prostatitis Without Antibiotics
Why Choose Us For Prostate Cancer Care
- Prostate cancer specialists: Because our team is subspecialized in prostate cancer, you get the most comprehensive, most personalized care plan available.
- Unparalleled in proton therapy: We’ve treated over 10,000 prostate cancer patients using proton therapy more than any other center in the world.
- Leaders in robotic surgery: Our surgeons perform more minimally-invasive robotic surgeries each year than those at any other teaching hospital in the West.
- State-of-the-art tech: As the largest urology group in the region, we offer you access to the most advanced technology available.
- Clinical trials: You have access to many clinical trials for prostate cancer, which may offer potential new treatments.
Permanent Versus Temporary Brachytherapy
In addition to permanent brachytherapy, temporary brachytherapy has also been used. In this technique, the implants deliver radiation to the prostate at a higher dose rate than is provided by a permanent implant. Currently, the isotope most commonly used for temporary brachytherapy is iridium -192, which provides a higher dose of radiation than the iodine -125 and palladium -103 permanent implants.
For high-dose-rate brachytherapy , a preplan is devised using TRUS to deliver 15 Gy/h to the prostate and smaller doses to the urethra and rectum. During the implantation, hollow needles are inserted transperineally and checked via TRUS to ensure reproduction of the preplan template. The needles are then connected to an automated remote-controlled loading machine. This device successively moves Ir-192 wires into the needles to the dwell positions for various durations. The total irradiation time is usually only 5-10 minutes.
HDRB is commonly delivered in 2 or more fractions of 810 Gy or more, with 6-24 hours between treatments. Patients require hospitalization while the implants remain in place but may go home once the implants are removed.
HDRB is usually used in combination with IMRT. The optimal patient population has not yet been determined. Most series reported are from single centers.
The American Brachytherapy Society has published consensus guidelines for high-dose-rate prostate brachytherapy, which note a growing experience with the use of this modality as monotherapy.
You May Like: What Age Can A Man Get Prostate Cancer
What Type Of Technology Does This Treatment Use
We use real time, 3-dimensional imaging to carefully place each seed at a predetermined location and depth. In this way, we cover the entire gland and the cancer site. The number of seeds implanted into your prostate will depend on your unique anatomy.
We place an ultrasound probe in your rectum to image the prostate. We also use continuous X-ray imaging. Together, these provide a magnified, 3D view of your prostate during the procedure. After the implantationand while you are still anesthetizedwe will check your urethra and bladder and retrieve any seeds found in your bladder.
Possible Side Effects Of Ebrt
Some of the side effects from EBRT are the same as those from surgery, while others are different.
Bowel problems: Radiation can irritate the rectum and cause a condition called radiation proctitis. This can lead to diarrhea, sometimes with blood in the stool, and rectal leakage. Most of these problems go away over time, but in rare cases normal bowel function does not return. To help lessen bowel problems, you may be told to follow a special diet during radiation therapy to help limit bowel movement during treatment. Sometimes a balloon-like device or gel is put between the rectum and the prostate before treatment to act like a spacer to lessen the amount of radiation that reaches the rectum.
Urinary problems: Radiation can irritate the bladder and lead to a condition called radiation cystitis. You might need to urinate more often, have a burning sensation while you urinate, and/or find blood in your urine. Urinary problems usually improve over time, but in some men they never go away.
Some men develop urinary incontinence after treatment, which means they cant control their urine or have leakage or dribbling. As described in the surgery section, there are different levels and types of incontinence. Overall, this side effect occurs less often with radiation therapy than after surgery. The risk is low at first, but it goes up each year for several years after treatment.
You May Like: What Are Treatment Options For Prostate Cancer
What Kind Of Treatment Follow
Patients usually return to see the radiation oncologist about two to eight weeks after the last radiation therapy session. The main purpose of this visit is to see if the side effects from treatmentâsuch as bowel or urinary symptomsâhave subsided. In most patients, these symptoms subside in a few weeks. The doctor will check up on you and make sure you make good progress in recovery. After that, you will have regular follow-ups every three to six months. Your doctor may use a digital rectal exam to assess your prostate. A blood test will measure your PSA level and assess your response to treatment. Higher PSA levels can indicate the presence of prostate cancer. During follow-up, your doctor can also monitor any late treatment side effects and help manage them.
You may ask the radiation oncologist, âHow am I doing? Is the cancer all gone? Am I cured?â However, they cannot answer these questions immediately. After radiation therapy, it may take months to see your full treatment response. The body gradually disposes of dead cancer cells. Some cancer cells, even if technically dead , may continue to function for a while before ultimately dying. The rate of PSA level drop for successful radiation therapy is much slower than that of surgery. PSA usually drops by half every three to four months after radiation, and typically to the lowest level in about 12 to 18 months.
Two Agents Approved For Psma
On May 26, FDA approved piflufolastat F 18 for use in a type of imaging procedure called PSMA PET in people with prostate cancer. The approval covers the use of piflufolastat F 18 in patients suspected of having metastatic prostate cancer or recurrent prostate cancer . Last year, the agency approved another imaging agent for PSMA PET, Ga 68 PSMA-11, for the same uses, but its use is largely limited to the two institutions where it is made.
In a statement, Lantheus, which manufactures piflufolastat F 18, said the imaging agent will be immediately available in parts of the mid-Atlantic and southern regions with broad availability across the U.S. anticipated by year end.
PSMA is often overproduced by prostate cancer cells but is generally not produced by most normal cells, making it an excellent target for both PET imaging and targeted systemic radiation therapy like 177Lu-PSMA-617, Dr. Morris said.
You May Like: Is Ejaculation Good For The Prostate Gland
How Does Radiotherapy Treat Advanced Prostate Cancer
Radiotherapy can be used in different ways to treat prostate cancer that has spread from the prostate to other parts of the body :
- as part of your first treatment for advanced prostate cancer
- to improve symptoms in areas where the cancer has spread
- to help some men with bone pain live longer and to treat bone pain.
All types of radiotherapy aim to destroy cancer cells.
If youre offered radiotherapy as part of your first treatment for advanced prostate cancer, youll have a type of radiotherapy called external beam radiotherapy.
If youre having radiotherapy to improve symptoms in areas where the cancer has spread, you may have external beam radiotherapy to the part of the body where the cancer is causing problems.
If your cancer is causing bone pain, you may be offered a type of internal radiotherapy called radium-223 to help you live longer and to treat the bone pain.
A clinical oncologist or radiographer will plan your radiotherapy with you. They will tell you if radiotherapy can help you and explain which type of radiotherapy you will have, how long the treatment could take and the possible side effects. This could depend on where your cancer has spread to, any symptoms youre having, and your general health and fitness. They can also tell you about any clinical trials that might be suitable.
A team of radiographers will give you the treatment. They will also give you support and information during your treatment.
Help Getting Through Cancer Treatment
People with cancer need support and information, no matter what stage of illness they may be in. Knowing all of your options and finding the resources you need will help you make informed decisions about your care.
Whether you are thinking about treatment, getting treatment, or not being treated at all, you can still get supportive care to help with pain or other symptoms. Communicating with your cancer care team is important so you understand your diagnosis, what treatment is recommended, and ways to maintain or improve your quality of life.
Different types of programs and support services may be helpful, and can be an important part of your care. These might include nursing or social work services, financial aid, nutritional advice, rehab, or spiritual help.
The American Cancer Society also has programs and services including rides to treatment, lodging, and more to help you get through treatment. Call our National Cancer Information Center at 1-800-227-2345 and speak with one of our trained specialists.
Don’t Miss: Does Prostate Affect Bowel Movements
If I Choose Surgery Will Radiation Treatment Still Be Required
Your surgery may be incomplete or show a more advanced cancer. If the surgeon has inadvertently cut through tumor, you have what is called a positive margin. Having a positive margin or disease that breaks through the capsule of the prostate gland or invades the seminal vesicles are reasons to meet with a radiation oncologist soon after you recover from surgery. Additional radiation therapy within three to six months may prevent the cancer from coming back. Discuss this option with your treatment team.
Using Radiation Radioimmunotherapy And Radioactive Isotopes Such As Lutetium 177 To Treat Prostate Cancer
Radiation is a mainstay in the treatment of prostate cancer. In men with localized prostate cancer , using radiation can help cure the cancer. In men with advanced disease, radiation can improve survival and help to manage pain.
Radiation can be delivered a variety of different ways. For example, there are external beams that can be used to deliver radiation from an external machine into the prostate, radioactive seeds that can be implanted, or ways to inject special radioactive isotopes directly into the bloodstream.
In the United States , there are older FDA-approved treatments utilizing radioactive isotopes for men with prostate cancer that has spread to the bones to decrease pain, called samarium-153 and strontium-89 . More recently, a bone-targeted alpha particle called radium-223 was approved because it leads to longer overall survival in men with symptomatic metastatic castration-resistant bone metastases. These bone-targeted radioisotopes have been useful because prostate cancer commonly spreads to bone. However, those drugs cannot treat other sites of tumors such as in the prostate, lymph nodes, or lung.
Learn more about how this treatment works in this video:
Read Also: How Do Know If You Have Prostate Cancer
Questions To Ask Your Doctor Radiographer Or Nurse
- Which type of radiotherapy is suitable for me and why?
- Will I have any other treatments while Im having radiotherapy?
- How long will the pain relief last? What other treatments are available to help with my pain?
- Will I get any side effects and if so, how can I manage them?
- Are there any safety guidelines I should follow during and after treatment?
- Who should I contact if I have any questions at any point during my treatment? How do I contact them?
- Will having this treatment mean I cant have other types of treatment later on for example, chemotherapy?
What Are Isotope Treatments Used For
In radionuclide or radioisotope therapy , a radioactive substance administered to the patient intravenously or orally is taken up by the targeted organ or tissue via normal metabolism and radiates locally there for a relatively short period. The radiation effect is utilised both for diagnostic and radiotherapy purposes.
The impact of radionuclide therapy is based on the local radiation impact of a radioactive substance taken up by cancer cells, destroying the tumor cells. The formation of a combination that is taken up by the tumor and destroys cancer cells is always an individually tailored process which requires expertise from a broad range of specialities.
Radionuclide therapies are an increasingly used form of treatment in various cancers. This is due to the fact that an increasing number of cancer tracers have been identified that allow the use of targeted radionuclide therapy. Lymphomas, for instance, can be treated with radiolabelled antibodies that are taken up by cancer tissue and destroy it by means of radiation and antibody formation.
Since the early 2000s, various radionuclide therapies have also been used to treat non-Hodgkins lymphoma, for example. The treatments are based on radiolabelled antibodies which combine the effect of the antibody itself and the cell-destroying effects of radiation.
Recommended Reading: What Age To Check Prostate Cancer
Targeting Psma: Not Just For Imaging
Like a number of other radiopharmaceuticals, 177Lu-PSMA-617 has two components: a drug that delivers the therapy to cancer cells and a radioactive particle. In the case of 177Lu-PSMA-617, the delivery vehicle is PSMA-617, a drug that latches onto a protein called PSMA that is often found at high levels on the surface of prostate cancer cells. The radioactive component is lutetium-177, which is being tested as a part of multiple radiopharmaceutical drugs.
As Dr. Morris explained, PSMA-617 is extremely adept at finding and locking on to the PSMA protein on cells. Once it binds to PSMA on a cancer cell, the whole molecule is internalized by the cell and the cell is exposed to a lethal dose of radiation from lutetium-177, he said.
The PSMA protein is also at the heart of a new type of imaging procedure called PSMA PET. This form of PET imaging is just starting to be used in men with prostate cancer to determine whether their cancer has spread, or metastasized, beyond the prostate. In the last several months, FDA has approved two such drugs, known as radiotracers, for PSMA PET imaging.
Who Can Have Radioisotope Therapy
Lutathera is for patients in general good health, with no liver or kidney dysfunction, who have pancreatic or small-bowel tumors that are recurring, inoperable or have not responded to treatment such as:
- Microwave ablation
- Oral chemotherapy
- Long-acting octreotide injections alone
If you are a candidate for surgery, we may offer Lutathera as a first treatment, depending on your condition.
Also Check: How Do They Check Your Prostate
Fact Sheet: Radiopharmaceutical Therapy And Prostate Cancer
Prostate cancer is the most commonly diagnosed cancer among men in the United States, other than skin cancer. According to the American Cancer Society, approximately 238,000 new cases of prostate cancer are diagnosed and more than 29,000 men die from the disease annually in the United States.
Imaging plays an important role in diagnosing and staging prostate canceras well as monitoring patients for recurrent disease . Radionuclide therapies have long been used to alleviate pain in patients with metastatic prostate canceror cancer that has spread to the boneand new therapeutic agents are under development as well.
What is radiopharmaceutical therapy, and how does it work?
Radiopharmaceutical therapy involves a radioactive drug called a radiopharmaceutical that targets cancer cells. Radiopharmaceuticals typically consist of a radioactive atom combined with a cell-targeting molecule that seeks and destroys cancer cells. Some radionuclides have the ability to target specific cells on their own.
When injected into the patients bloodstream, the radiopharmaceutical travels to and delivers radiation directly to or near disease sites. This treatment is a targeted therapy. It damages cancer cells while limiting radiation exposure to healthy tissue. This type of therapy offers promise as a vehicle for personalized treatment of cancer because it can be tailored to the molecular properties of a specific tumor.
About prostate cancer
- lutetium-177 PSMA-617
- radium-223 dichloride
