European Association Of Urology
The EAU Guidelines on Prostate Cancer were updated in 2014 to discuss all aspects of prostate cancer screening, diagnosis, staging, and treatment . The EAU discussed the use of mpMRI in both a triage setting, as well as a trigger for repeat targeted biopsy. Based on current data, mpMRI is recommended only for diagnosis in the latter situation .
The recommendations for staging incident disease were divided by T-, N-, and M-stages at diagnosis, with multiple imaging methods considered for each stage category. The EAU recommended against using TRUS or CT to stage the primary lesion . Routine use of MRI among low-stage patients was similarly discouraged , although mpMRI was recommended for local staging in cases where the results might change management .
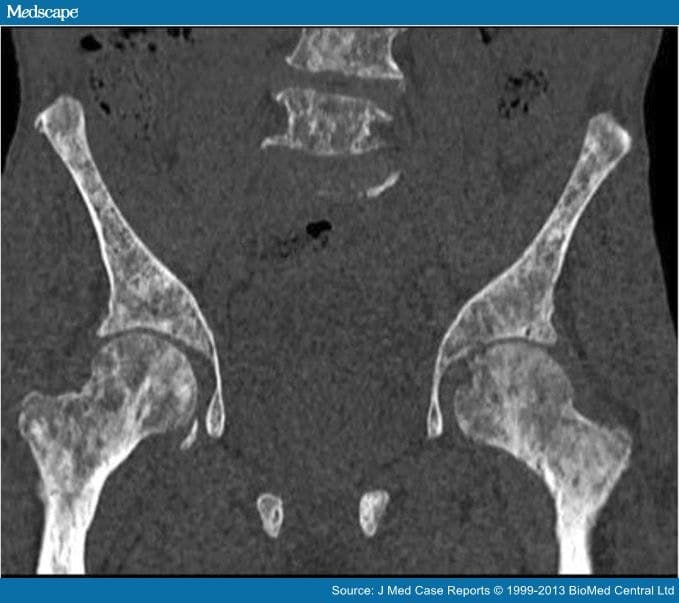
CT and MRI were the primary methods considered to stage nodal metastases in these guidelines. As these imaging methods use size to detect positive nodes, their sensitivity is low . Lymph node staging was recommended only for patients in whom curative treatment is planned and who have PSA levels of > 10 ng/mL, Gleason score 8, or clinical stage T3 .
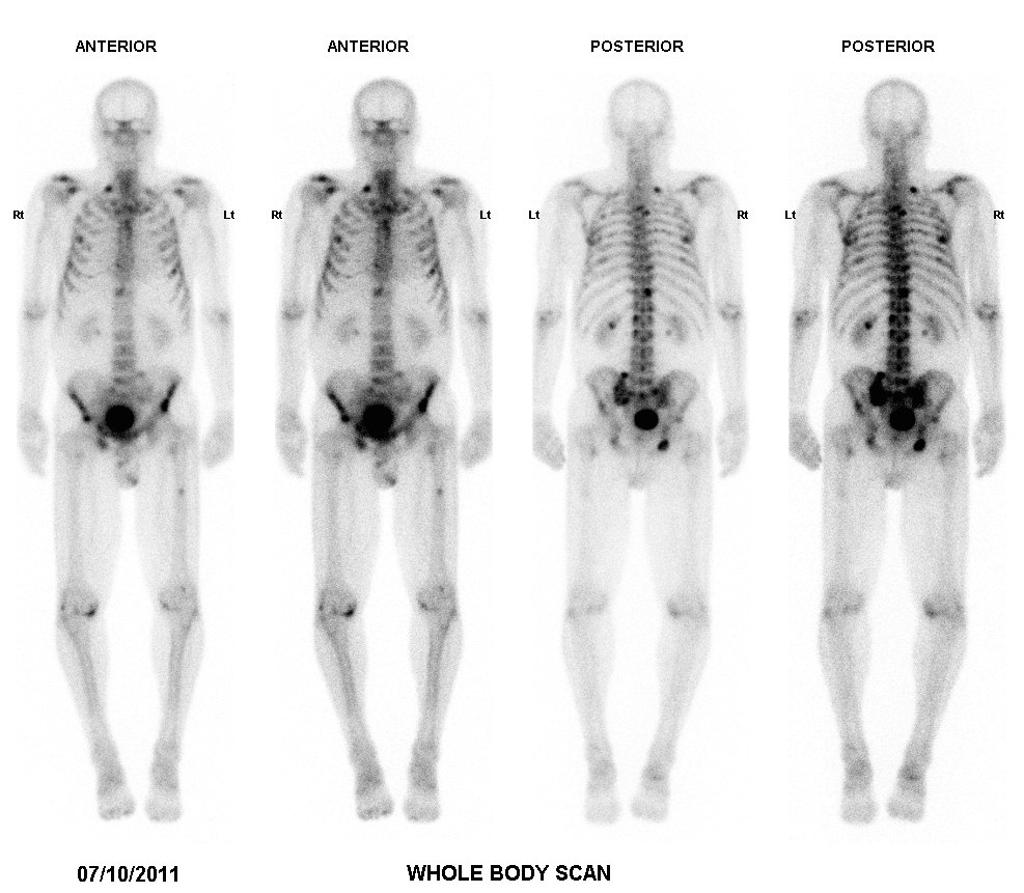
Bone scan is typically used to stage metastatic disease, but the performance of this imaging method is highly dependent on disease characteristics. The EAU guidelines recommended using bone scan to stage patients with PSA levels of > 10 ng/mL, Gleason score 8, or clinical stage T3, along with patients with symptoms consistent with bone metastasis .
How The List Was Created
15: The American Urological Association established a committee to review evidence from the associations guidelines and identify potential topics for nomination to the AUAs Choosing Wisely list. The committee reviewed a number of recommendations and through a consensus process identified the five tests or procedures that should be questioned. These recommendations were reviewed and approved by the AUA Board of Directors.
610: Following its previous successful participation in Choosing Wisely in 2013, the American Urological Association established a new committee in 2014 to develop a second list of recommendations. The group sought input from the AUA membership in addition to drafting potential suggestions after studying evidence from the associations evidence-based clinical practice guidelines and other clinical documents. The committee reviewed all recommendations and narrowed them to a list of fifteen possibilities. Again, the committee sought AUA member input by asking members to vote for their top five selections from the list of candidate recommendations. After the votes were tallied, the list of five recommendations was determined. These recommendations were reviewed and approved by the AUA Board of Directors in February 2015.
AUAs disclosure and conflict of interest policy can be found at www.auanet.org.
Risk Stratification And Staging
For patients with clinically localized prostate cancer, National Comprehensive Cancer Network guidelines define five risk categories: very low, low, intermediate, high, and very high. In contrast, the 2022 update of the American Urological Association/American Society for Radiation Oncology defines three risk categories: low, intermediate, and high the update combines the prior categories of very low risk and low-risk disease, as the recommended management for these patients is consistent. Both the NCCN and the AUA/ASTRO guidelines subdivide intermediate risk into favorable and unfavorable categories. ESMO guidlines also recommend classifying localized prostate cancer as low, intermediate, or high risk, as a guide to prognosis and therapy. See the Table below.
Also Check: When Should You Have Your First Prostate Exam
Getting My Scan Results
Your doctor or nurse will tell you how long it will take for the results of all the tests to come back. Its usually around two weeks.
Your doctor will use your scan results to work out the stage of your cancer in other words, how far it has spread. This is usually recorded using the TNM system.
- The T stage shows how far the cancer has spread in and around the prostate.
- The N stage shows whether the cancer has spread to the lymph nodes.
- The M stage shows whether the cancer has spread to other parts of the body.
American Board Of Internal Medicine Choosing Wisely
Choosing Wisely is an initiative launched by Consumer Reports and the ABIM Foundation in 2012 to start conversations between patients and their doctors regarding stewardship of healthcare resources and the proper delivery of care. Various professional societies participated in Choosing Wisely by creating lists of procedures or tests that could be eliminated, both improving care and saving money simultaneously.
The AUA Top Five list, released in 2013, focused on decreasing the inappropriate use of bone scan to stage incident prostate cancer as an area for improvement . The statement suggested that bone scans should not be used routinely in patients with PSA levels of < 20 ng/mL and Gleason score 6, as long as bony involvement is not suspected based on clinical examination. The American Society of Clinical Oncology also released their own Choosing Wisely document in 2012, which recommended against CT, PET, or bone scan evaluation of low-risk prostate cancer . According to their data, performing these imaging studies on low-risk patients may lead to misdiagnosis and over-treatment.
Don’t Miss: Percent Of Men With Prostate Cancer
Did Androgen Deprivation Therapy Cause Bone Loss For You
ADT long term ie 4 years has caused Osteopenia.
Interested in more discussions like this? Go to the Prostate Cancer group.
I had a Bone Scan before any treatment for my prostate cancer . It showedosteopenia. I am 75. Subsequent treatment over the next 8 mos included Radiation, Lupron, Zytiga. I assume the osteopenia is close to osteoporosis. No broken bones yet. Carpe Diem.
Welcome @tott123. Osteoporosis can be a complication of androgen deprivation therapy for prostate cancer. I’m glad that both you and @spryguy were being monitored and that the bone loss was discovered in the osteopenia phase before full blown osteoporosis.
What guidance did you get from your cancer team regarding lifestyle ways to avoid further bone loss, like diet, exercise, or treatments that help? Are you still taking ADT?
Welcome @tott123. Osteoporosis can be a complication of androgen deprivation therapy for prostate cancer. I’m glad that both you and @spryguy were being monitored and that the bone loss was discovered in the osteopenia phase before full blown osteoporosis.
What guidance did you get from your cancer team regarding lifestyle ways to avoid further bone loss, like diet, exercise, or treatments that help? Are you still taking ADT?
Biopsy During Surgery To Treat Prostate Cancer
If there is more than a very small chance that the cancer might have spread , the surgeon may remove lymph nodes in the pelvis during the same operation as the removal of the prostate, which is known as a radical prostatectomy .
The lymph nodes and the prostate are then sent to the lab to be looked at. The lab results are usually available several days after surgery.
Read Also: Can You Give Yourself A Prostate Massage
Genetic Testing For Some Men With Prostate Cancer
Some doctors now recommend that some men with prostate cancer be tested to look for certain inherited gene changes. This includes men in whom a family cancer syndrome is suspected, as well as men with prostate cancer that has certain high-risk features or that has spread to other parts of the body. Talk to your doctor about the possible pros, cons, and limitations of such testing.
Percentage Of Free Psa
The measurement of bound and free PSA can help to differentiate mildly elevated PSA levels caused by cancer from elevated levels resulting from benign prostatic hyperplasia. The lower the ratio of free-to-total PSA, the higher the likelihood of cancer. For example, among men with greater than 25% free PSA, only 8% are found to have cancer at prostate biopsy.
In contrast, more than half of men with less than 10% free PSA are found to have cancer at biopsy. While cutoffs may be used, the percentage of free PSA is usually employed as an additional factor in making an informed recommendation for or against biopsy. Generally, these percentages are useful in patients who have a PSA level in the range of 4-10 ng/mL.
This information is most useful in men with very large glands or in whom 1 biopsy result has already been negative. In healthy men with a PSA level of 4-10 ng/mL, many recommend biopsy without the additional free-PSA test or consider a trial of antibiotic therapy for 4-6 weeks before repeating the PSA test.
Read Also: Who Do You See For Prostate Problems
American College Of Radiology
The ACR Appropriateness Criteria for specific clinical conditions are reviewed every 2 years and were most recently updated for prostate cancer in 2013 . The multidisciplinary committee reviewed the evidence for each prostate cancer imaging method, including US, MRI, CT, bone scan, and PET. US was deemed to be unable to improve staging accuracy, although investigational techniques like contrast-enhanced and three-dimensional US may improve performance. Imaging with Indium Capromab and PET were not recommended for initial staging due to insufficient evidence at this time.
ACR recommended that for patients with low-risk disease , CT is usually not appropriate for staging. For intermediate-risk patients CT may be appropriate, while high-risk patients are good candidates. These recommendations were based on data suggesting CT for locoregional and nodal staging suffers from very poor accuracy , and yet it is widely overused. CT is not sensitive for detecting extraprostatic extension or seminal vesicle invasion.
The ACR only recommends bone scan in high-risk patients with the caveat that it may be appropriate in intermediate-risk patients as well. Studies have shown that patients with a low PSA level, Gleason score, and clinical stage have a very low probability of positive bone scan.
Bone Scans In Diagnosis Of Prostate Cancer
A bone scan uses tiny amounts of radioactive materials called tracers that are injected into the patient. These tracers accumulate in certain organs and tissues, such as bones, and give off a type of radiation called gamma radiation. The gamma rays can be seen by using a special camera, which produces images that can be interpreted by radiologists or by specialists in nuclear medicine.
A clever way to think about a bone scan is that it is the complete opposite of a X-ray examination. In an X-ray examination the radiation passes into or through your body from an external machine to create an image on film placed on the other side of your body. In a bone scan, the source of the radiation is inside your body and travels to the surface, where a camera detects it.
For patients who are newly diagnosed with prostate cancer, the value of a bone scan is limited. It would be unusal for the doctor to request a bone scan for any patient with a Gleason score of less than 7 and a PSA level of less than 20 ng/mL.
Patients with a Gleason score of 7 or higher may, however, be candidates for a bone scan, whatever their PSA level. A bone scan may be considered important in any patient with a Gleason score of 7 or higher who appears to be at high risk of bony metastatic disease. A bone scan is also indicated for any patient with prostate cancer who has symptoms suggesting bony metastases.
Content on this page last reviewed and updated April 26, 2008.
Recommended Reading: Can A Swollen Prostate Cause Erectile Dysfunction
Information And Decision Support For People With Prostate Cancer Their Partners And Carers
Information
1.1.1 For advice on communication and patient-centred care throughout the patient journey, follow the recommendations in the NICE guidelines on improving outcomes in urological cancers and improving supportive and palliative care for adults with cancer.
1.1.2 Offer people with prostate cancer information tailored to their own needs. This information should be given by a healthcare professional and may be supported by written and visual media.
1.1.3 Offer people with prostate cancer advice on how to get information and support from websites, local and national cancer information services, and from cancer support groups.
1.1.4 Choose or recommend information resources for people with prostate cancer that are clear, reliable and up to date. Ask for feedback from people with prostate cancer and their partners or carers to identify the highest quality information resources.
1.1.5 Find out the extent to which the person wishes to be involved in their decision making, and ensure that they have sufficient information to do so.
1.1.6 Use an up-to-date decision aid in all urological cancer multidisciplinary teams . Healthcare professionals trained in its use should offer it to people with localised prostate cancer when making treatment decisions.
1.1.7 Use nomograms together with people with prostate cancer to help:
-
with decision making
-
predict risk of treatment failure.
1.1.8 Explain the reliability, validity and limitations of any predictions made using nomograms.
Appropriate Use Criteria For Bone Scintigraphy In Prostate And Breast Cancer
The AUC for Bone Scintigraphy addresses several clinical scenarios for metastatic bone disease, across a variety of oncologic indications. To improve utilization and guide providers to use bone scan in a more appropriate way, the Society of Nuclear Medicine and Molecular Imaging , the European Association of Nuclear Medicine and the American Society of Clinical Oncology have collaboratively developed criteria for the appropriate use of this imaging technology to aid in the diagnosis of people with malignant diseases such as breast cancer and prostate cancer.
SNMMI assembled an autonomous Bone Scan Workgroup consisting of experts in the field of nuclear medicine including radiologists and oncologists to review the scientific literature and develop consensus recommendations for the clinical use of this technology. The Oregon Health Science University’s Evidence-based Practice Center conducted a systematic review of existing evidence based on the scope and parameters the Bone Scan Workgroup put together, which they used to make their recommendations for clinical use.
Don’t Miss: Metastatic Prostate Cancer Treatment Options
Prostate Health Index Testing
The Prostate Health Index test is a diagnostic blood test that combines free and total PSA and the pro-PSA isoform . The PHI test is intended to reduce the number of unnecessary prostate biopsies in PSA-tested men. In prospective multicenter studies, the PHI test has outperformed free and total PSA for detection of prostate cancer and has improved prediction of clinically significant prostate cancer in men with a PSA of 2 or 4 ng/mL to 10 ng/mL.
Ct Scanning Mri And Bone Scanning
Men with PSA levels above 10 ng/mL, high-grade histology , or physical findings that suggest stage T3 disease should probably undergo a staging computed tomography scan and bone scan. CT scanning is the one modality with evidence-based guidelines. The CT scan can be used to evaluate extension into the bladder and lymph nodes to help stage the patient’s cancer or to consider lymph node sampling prior to treatment.
According to the National Comprehensive Cancer Network , technetium-99m-methyl diphosphonate bone scan is indicated in the initial evaluation of patients at high risk for skeletal metastases, as indicated by any of the following :
- T1 disease, PSA 20
- Symptoms suggestive of osseous metastasis
The NCCN recommends pelvic CT or magnetic resonance imaging in patients with any of the following:
- T1-T2 disease and nomogram-indicated probability of lymph node involvement > 10%
Conventional endorectal MRI is helpful for localizing cancer within the prostate and seminal vesicles and for local staging. Dynamic, contrast-enhanced MRI and MR spectroscopic imaging are complementary in local staging, but their use is currently limited to a research setting.
- Detection of large and poorly differentiated tumors
- T staging: Detection of extracapsular extension, with high negative predictive values in low-risk men
- N staging: MpMRI is equivalent to CT scan
- M staging: MpMRI outperforms bone scan and targeted x-rays for M staging, with 98-100% sensitivity and specificity
Read Also: Can You Remove Entire Prostate
A Routine Bone Scan Is Unnecessary In Men With Low
Low-risk patients are unlikely to have disease identified by bone scan. Accordingly, bone scans are generally unnecessary in patients with newly diagnosed prostate cancer who have a PSA < 10.0 ng/mL and Grade Group 1 disease unless the patients history or clinical examination suggests bony involvement. Progression to the bone is much more common in advanced local disease or in high-grade disease that is characterized by fast and aggressive growth into surrounding areas such as bones or lymph nodes.
These items are provided solely for informational purposes and are not intended as a substitute for consultation with a medical professional. Patients with any specific questions about the items on this list or their individual situation should consult their physician.
American Society Of Clinical Oncology
ASCO recommendations for use of these regimens are as follows:
-
Docetaxel plus ADT should be offered to men with metastatic noncastrate prostate cancer with high-volume disease who are candidates for treatment with chemotherapy, but should not be offered to those with low-volume metastatic disease. The recommended regimen of docetaxel in this setting is six doses of 75 mg/m2, either alone or with prednisolone, administered at 3-week intervals.
-
Abiraterone plus ADT should be offered to men with high-risk de novo metastatic noncastrate prostate cancer, and may be offered to men with low-risk de novo metastatic noncastrate prostate cancer. The recommended regimen in this setting is abiraterone 1,000 mg with either prednisolone or prednisone 5 mg once daily until progressive disease is documented.
-
Enzalutamide plus ADT should be offered to men with metastatic noncastrate prostate cancer, including both those with de novo metastatic disease and those who have received prior therapies, such as radical prostatectomy or radiotherapy for localized disease. The recommended enzalutamide dosage in this setting is 160 mg/day.
-
Apalutamide plus ADT should be offered to men with metastatic noncastrate prostate cancer, including those with de novo metastatic disease or those who have received prior therapy, such as RP or RT for localized disease. The recommended apalutamide dosage in this setting is 240 mg/day.
Read Also: How Long Does Prostate Biopsy Take
