Prostate Cancer Risk Groups
Prostate cancer can be categorised into one of 5 risk groups in the Cambridge Prognostic Group .
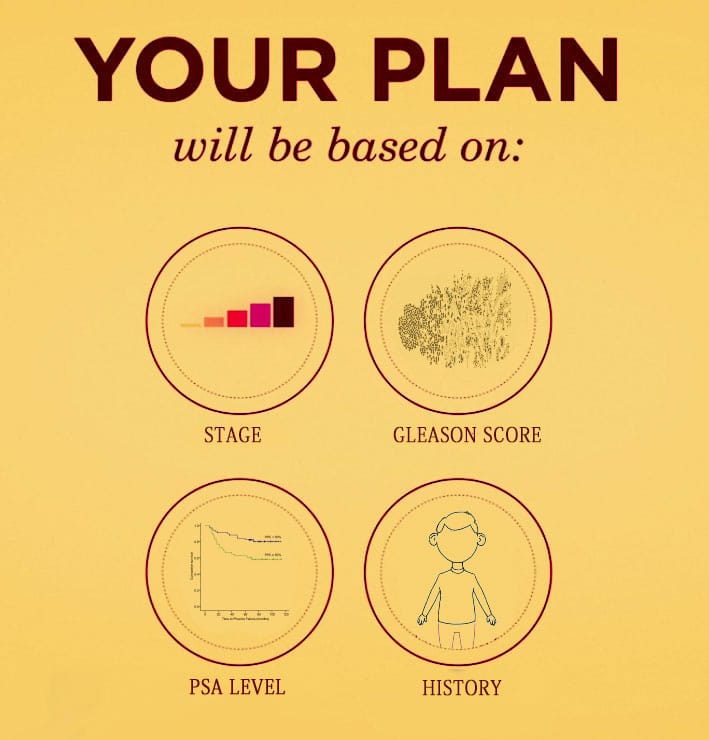
Doctors will look at the Grade Group , prostate specific antigen level and tumour stage to decide which CPG group the prostate cancer is.
The risk group of the cancer will help determine which types of treatments will be necessary.
If prostate cancer is diagnosed at an early stage, the chances of survival are generally good.
Prostate Surgery May Leave More Options Open
“It is related to the burden of disease,” Rapiti tells WebMD. “The more of the tumor you are able to take away and the less you leave, the less chance you have for metastases .”
And Bouchardy says that even if surgery doesn’t get every cancer cell, surgery patients with recurrent disease have more options than radiation patients with recurrent disease.
“Recurrence after surgery is easier to treat successfully — with irradiation or irradiation plus hormonal therapy — than after irradiation, when only hormonal therapy remains as an option,” she tells WebMD.
Ash Tewari, MD, is director of prostate cancer-urologic oncology outcomes at the Brady Urology Institute at Cornell University. Tewari has been studying long-term outcomes after prostate cancer treatment. He was not involved in the Swiss study.
“If you look not only at this study but at the studies we brought out in the last three or four years, in terms of survival for 10 or even 15 years, there is a distinct advantage in patients who underwent surgery for localized prostate cancer,” Tewari tells WebMD. “This has implications for patients comparing different treatment options.”
Surgery is not the best choice for every patient. The Swiss researchers found that elderly patients and those with very early-stage tumors did just as well after radiation therapy as surgery patients.
The Swiss study appears in the Oct. 8 issue of Archives of Internal Medicine.
Show Sources
Radiation Treatment For Prostate Cancer
Radiation treatment is the use of radiation beams to destroy cancer cells or slow their growth.
Radiation treatment is usually recommended for prostate cancer:
- if you are not well enough for surgery
- if you have had surgery for prostate cancer but there are signs that not all the cancer has been removed
- to relieve pain caused by cancer that has spread to the bones
- to shrink blocks in your lymphatic or urinary system
- when radiation treatment is your preferred treatment option
There are three types of radiation treatment for prostate cancer:
External beam radiotherapyThe most common radiation treatment for prostate cancer. The radiation beams are given from outside the body onto the area affected by cancer.
Low-dose-rate brachytherapy Low-dose-rate brachytherapy is an internal radiation treatment where radioactive seeds are permanently placed inside the prostate gland.
It is used when the cancer is low-risk and found only inside the prostate. It is only available in a few private centres in New Zealand.
After your radiation treatment, you will be radioactive and need to take special care at home. Your treatment team will explain what to do.
High-dose-rate brachytherapy High-dose-rate brachytherapy is an internal radiation treatment where radioactive sources are temporarily placed into the prostate with needles.
It is usually used in combination with external beam radiotherapy to treat higher-risk prostate cancer. It may also be used alone to treat low-risk prostate cancer.
Don’t Miss: How To Reduce Dht In Prostate
Most Prostate Surgeries Are Now Done Robotically
In the U.S., about 95% of prostate surgeries are performed robotically, with the surgeon sitting apart from the patient at a control console, watching progress on a high-definition monitor while controlling the robot remotely. The robot translates the surgeons hand movements into precise micro-movements, making it easy for them to manipulate a tiny camera and surgical instruments with greater range of motion than they could with their hands.
Robotic procedures are done with the patient under general anesthesia and take two hours or more to complete. The possibility of side effects is a concern with any type of prostatectomyeven with the aid of a robotthe main ones being an inability to control urine after surgery, and difficulty having or maintaining an erection. There are several different types of robotic surgeries, and each one comes with its own set of benefits.
Mri With A Tesla 30 Magnet Age Of Friend
Speak with the urologist about prescribing a Tesla 3.0 MRI . This test is very effective in indicating if there is any nodule involvement, if there is involvement in one or two lobes, will show size of prostate, any evidence of extracapular extension, will stage the disease. An MRI with the 3.0 Tesla magnet, is the gold standard. There are certain major hospitals that have MRI machines with a 3.0 Tesla magnet. In my laymans opinion it is advisable to have such a test before any surgery or another active treatment which is a localized one. If the cancer is outside the prostate these type treatments may not be a best decision for treatment since additionally treatment will still be required, and side effects of various treatments are cummulative.
The side effects of surgeries are basically greater than other active treatment types. Surgery is less successful among older men than younger so for example a doctor may perform an excellent surgery for a 50 year old, who will have no side effects and the exact same surgery for a 70 year old who will have side effects.
How old is your friend?
Also Check: What Is Low Risk Prostate Cancer
You May Like: What Does Prostate Cancer Do
Treatment Choices For Prostate Cancer That Has Spread
If your prostate cancer has spread to other parts of your body, it cannot be cured. But it can be controlled by lowering the level of testosterone in your body with hormone therapy. You can have hormone therapy as
- Tablets you take each day
- Injections each month or every 3 months or 6 months.
- Tablets for a few months, then a break, followed by more tablets, and so on
Another way of reducing testosterone levels is removing the testicles. This is called surgical castration or orchidectomy. It quickly lowers the testosterone levels and can control the cancer very well.
Orchidectomy or hormone therapy can control the cancer for a few years in many men. When the cancer starts to develop again, your doctors may suggest treatment with chemotherapy or steroids. These can control or shrink the cancer for some time. Chemotherapy can work well at controlling advanced prostate cancer in some men.
If your cancer has spread to your bones and is causing you pain, your specialist may suggest radiotherapy to the affected areas of bone. Radiotherapy for bone pain can work very well to strengthen the bone and relieve pain. The damaged bone begins to repair itself after radiotherapy treatment. Bisphosphonate treatment can also reduce bone pain and help to reduce the risk of bone fracture.
For more information on Thrombosis which may occur during / after chemo click here
Determining The Prostate Cancer Treatment Thats Right For You
Once prostate cancer has been detected, graded, and given a Gleason score, your doctor will most likely refer you to a cancer specialist called an oncologist. The cancer care team will review the data and other factors like your age, the stage of the cancer, the presence of symptoms, and your overall general health before making the best recommendation.
The stage of cancer helps your oncologist determine how far cancer has spread throughout the body if at all.
- Stage 1 prostate cancer exists in the prostate only.
- Stage 2 prostate cancer has advanced more than stage 1 but hasnt yet spread to any other body parts.
- Stage 3 prostate cancer may still only exist on the prostate but covers more prostate than stage 2 and is accompanied by an abnormal PSA level. Stage 3 prostate cancer has sometimes spread to some of the surrounding tissues.
- Stage 4 prostate cancer has spread to other parts of the body.
This is only a brief overview of the stages, as they can be further broken down for each patients unique situation. Learn more about the staging of prostate cancer.
If the cancer has moved outside of the prostate , youre more likely to need treatment right away. But for those patients who have cancer thats contained inside the prostate and is low grade, there are a few treatment options to consider starting with a watchful waiting approach.
You May Like: How Long Is Hormone Therapy For Prostate Cancer
Hormone Therapy For Disseminated Pca
Metastatic PCa is currently not curative, but most patients will have significant initial responses to therapy. Upfront ADT has been the standard of care for treatment naïve PCa, based on Huggins and Hodges seminal work in 1941. Patients with symptomatic disease or metastasis at high risk sites should be treated promptly symptoms from metastatic PCa can rapidly resolve within days to weeks if responsive to initial ADT, and thus it is important to consider this when evaluating PS and treatment decisions. The addition of a continuous anti-androgen to an LHRH analogue has been extensively studied, and meta-analyses have shown a small but significant benefit of combined androgen blockade.6,7 However, there is currently no recommendation for or against combined androgen blockade in this setting.8
Comparison Between Rp And Pb
One small Italian trial randomized 200 patients to receive RP or PB.4 With a median follow up of 5 years, PRFS was the same in both groups . At 6 months and 1 year follow-up, brachytherapy patients had more irritative urinary symptoms but better sexual function. After 5 years, RP patients had a higher incidence of urinary stricture and urinary incontinence . Sexual function recovery was greater with brachytherapy in the first year after treatment however, it was virtually identical after 5 years between the 2 arms. There was no difference in overall QOL measures between the 2 groups of patients.
Also Check: My Dad Has Prostate Cancer When Should I Get Checked
What Does It Mean To Have A Gleason Score Of 6 7 8 Or 9
Because grades 1 and 2 are not often used for biopsies, the lowest Gleason score of a cancer found on a prostate biopsy is 6. These cancers may be called well differentiated or low-grade and are likely to be less aggressive that is, they tend to grow and spread slowly.
Cancers with Gleason scores of 8 to 10 may be called poorly differentiated or high-grade. These cancers are likely to grow and spread more quickly, although a cancer with a Gleason score of 9-10 is twice as likely to grow and spread quickly as a cancer with a Gleason score of 8.
Cancers with a Gleason score of 7 can either be Gleason score 3+4=7 or Gleason score 4+3=7:
- Gleason score 3+4=7 tumors still have a good prognosis , although not as good as a Gleason score 6 tumor.
- A Gleason score 4+3=7 tumor is more likely to grow and spread than a 3+4=7 tumor, yet not as likely as a Gleason score 8 tumor.
Also Check: What Does Prostate Cancer Feel Like
What Is Prostate Cancer
Prostate cancer occurs in the prostate gland, a part of mens reproductive system. It can be slow-growing or aggressive and may spread to other body parts, such as the bones or lymph nodes. It is important to get regular screenings for prostate cancer, as early detection and treatment can help improve the chances of a successful outcome.
Prostate cancer affects older men more and can lead to serious health problems if not diagnosed and treated early. A study published in the JAMA Network journal states that the trends for metastatic prostate cancer increase in older adults.
The study considered the number of prostate cancer cases in two age groups, 45-74 and 75 and above. Data shows that 56.5% of patients were reported in adults aged between 45 and 74, and 43.5% of cases were reported in adults aged over 75 years.
Don’t Miss: Prognosis Of Prostate Cancer By Stage
Side Effects Of Radiation For Prostate Cancer
The primary potential side effects of radiation treatment for prostate cancer include bowel problems, urinary problems and sexual function issues.
According to patient-reported outcomes measuring quality of life from men who participated in the 10-year, randomized Prostate Testing for Cancer and Treatment trial, men who were treated with radiation reported little increase in urinary leakage after radiation therapy. They also reported less sexual dysfunction when compared to men who were treated with surgery. However, men treated with radiation reported a higher incidence of bowel problems, such as loose and bloody stools. These side effects are often short-term for most patients, but some experience long-term side effects.
Ultimate Outcomes Are Similar Regardless Of The Surgical Approach
In general, while each approach has its advantages, all have been shown to have similar outcomes, adds Dr. Sprenkle. There are no significant differences in outcomes for patients between the open surgery and robotic ones. There is less blood loss on average with robotic surgery, and in the hands of a good surgeon, continence and sexual preservation is the same, he says, adding that while it varies from patient to patient, average recovery time is six weeks. And cancer control is the same. Put another way: Its better to focus on finding the right surgeon rather than the approach or type of surgery.
As far as what that means for patients deciding on which surgery they should get, Dr. Sprenkle says that its important to take time to think about all of your options.
And ask a lot of questions, he says.
You May Like: Treatment Options Of Prostate Cancer
Box : Criteria For The Diagnosis Of Prostatic Adenocarcinoma9
-
Architectural: infiltrative small glands or cribriform glands too large or irregular to represent highgrade prostatic intraepithelial neoplasia
-
Nuclear atypia: nuclear and nucleolar enlargement
Nuclear hyperchromasia
Before searching for these criteria, it is important to scan sections of the needle core tissue, at both lowpower and highpower magnification, in order to appreciate the architecture and cytological features of benign glands in the tissue. The arrangement of the benign glands and the nuclear appearances of the lining cells serve as important points of reference for comparison when evaluating atypical glands because there can be substantial variability between individual cases in histological characteristics because of differences in fixation, section thickness and H& E staining.
Figure 6Comedocarcinoma, highgrade Gleason pattern 5, with comedonecrosis.
Figure 8Penetration of smallgland prostatic adenocarcinoma into the seminal vesicle or ejaculatory duct wall. It is difficult to tell, on needle biopsy, whether this is definitely a seminal vesicle or an ejaculatory duct. Seminal vesicle or ejaculatory duct glands are crowded larger glands at lower right.
Figure 9Minimal adenocarcinoma. Compared with staining by haematoxylin and eosin , the 34E12 and p63 immunohistochemical stains highlight the invasion of the malignant glands, which lack basal cells .
Ng Tohu Matua: Te Maimoatanga Matepukupuku Repe Ure
- M te mhio ki te whanga o t matepukupuku repe ure, e whina i t rp maimoa ki te whakamahere i maimoatanga.
- Ka whakaritea he whakamtau toto prostate specific antigen ki te ine i te taumata PSA kei roto i t toto. Mehemea
- kua piki t PSA, he tohu tnei kua piki ake te mrea o t whai i te matepukupuku repe ure, e ai ki te tangata whai taumata PSA pai.
- Ara an tahi atu take, atu i te matepukupuku, piki ai te PSA, n reira, kore e taea te whakamahi i te whakamtautau PSA anake ki te whakatau i te matepukupuku repe ure.
- Ko te whakamtautau -mati tou, ko te porooro, ko te unuhanga tahi atu whakamtautau.Mehemea kei roto te matepukupuku i to tauira unuhanga, ka tauinetia m te whakamahi i te tauine ISUP .
- He huarahi te mahi tauine ki te krero i te momo hua u ptau matepukupuku, te tere o t rtou tipu, me te hua o tna kaha ki te hrapa ki whi k o te tinana.Tr pea ka whakahaerehia tahi atu titiro whakatau pr ki te CT, ki te MRI rnei, , i tahi w, he titiro whakatau -kiwi.Ka whakamahia ng putanga o ng whakamtautau me ng titiro whakatau ki te krawarawa i te whanga taumata o t matepukupuku tna rahi, me tna kaha rauroha.
You May Like: How Do You Do A Prostate Exam
How We Approach Prostate Cancer Treatment At Ctca
When you come to CTCA for a diagnostic consultation or second opinion, your case is reviewed by a multidisciplinary team of genitourinary cancer experts before you arrive for your first appointment. This care team may include a medical oncologist, a urologist or urologic oncologist and a radiation oncologist.
If we determine you need additional diagnostic evaluations, such as imaging or genomic testing, we schedule those procedures for you before your arrival.
Well also schedule appointments for you with our integrative care providers, who work to prevent and manage side effects of cancer and its treatment.
Together, we develop a treatment plan thats based on your unique needsusually within two to three days. Our goal is to give you and your caregivers a clear understanding of your options to empower you to make an informed decision about your care.
At CTCA, we strive to treat our patients as we would want our own loved ones to be treated: with compassion, dignity and respect. Its the basis of our foundation, and we call it the Mother Standard® of care.
Are There Side Effects Of The Combination Approach To Prostate Cancer Radiation Therapy
When it comes to early stages of disease, patients very frequently do well with either brachytherapy or external beam radiation. Success rates of around 90% or higher can be achieved with either approach. When the disease is somewhat more advanced based on the PSA level, Gleason score, extent of visible disease on magnetic resonance imaging we have learned over the years that higher doses of radiation are critical to achieving better results. Some evidence, including a large trial, suggests that for patients with intermediate- or high-risk prostate cancer, a combined approach using brachytherapy along with external beam radiation may be best compared to standard dose external beam radiation therapy alone.
Don’t Miss: Testosterone And Prostate Cancer 2020
