Selection Of Candidates For Nadt
High-risk patients with localized prostate carcinoma are likely to benefit most from effective neoadjuvant therapy. However, heterogeneous definitions of high-risk disease render trial-to-trial comparisons difficult.
The use of preoperative nomograms that incorporate clinical T classification, serum PSA level, and biopsy Gleason grade can enhance prediction of the risk of PSA recurrence and selection of a relatively homogeneous population. The percentage of cancer in biopsy cores and the number of positive biopsy cores, as well as the incorporation of biomarkers , may further improve predictive accuracy.
Although a relatively high threshold of PSA recurrence to determine eligibility is reasonable, it may negatively affect accrual. In addition, investigators may determine that radiotherapy, instead of prostatectomy, is the optimal treatment in such high-risk patients. Conversely, setting a lower threshold of recurrence may result in unnecessary treatment, a reduction in the event rate, and an increase in the number of patients required.
It may be reasonable to hypothesize that patients with a relatively high risk of recurrence may be optimal candidates for cytotoxic chemotherapy, whereas those with a lower risk of recurrence may be optimal candidates for more tolerable biologic agents and immunotherapy.
How Effective Is Hormone Therapy For Prostate Cancer
In the initial years of diagnosis, hormone therapy for prostate cancer can help patients with their symptoms and add years to their lives.
For men who need hormone therapy, such as men whose prostate-specific antigen levels are rising after surgery or radiation or men with advanced prostate cancer who dont yet have symptoms, its not always clear when the best time is to start hormone treatment:
- Some doctors think that hormone therapy works better if its started as soon as possible, even if the patient feels well and is not exhibiting any symptoms. Studies have shown that hormone treatment may slow down the disease and perhaps even help men live longer.
- Some doctors, however, don’t agree with this approach. Because of the side effects and the risk of the cancer becoming resistant to therapy sooner, some doctors feel that treatment should not be started until cancer symptoms appear.
Orchiectomy Surgical Removal Of The Testicles
Once a common treatment, orchiectomy is rarely used now, thanks to the development of advanced ADT drugs. The procedure removes the testicles the source of most testosterone production. The scrotal sac is left intact, and patients can have testicular prostheses implanted for cosmetic purposes. Orchiectomy is effective in drastically reducing levels of testosterone, but it has several downsides. Removal of the testicles is permanent and irreversible. Loss of the testicles makes it challenging to have intermittent hormone therapy, an advantageous treatment. And there is a psychological effect: Many patients feel distress related to the idea of lost masculinity if they undergo this procedure.
Recommended Reading: How To Stimulate Prostate Gland
Stereotactic Body Radiation Therapy
This technique uses advanced image guided techniques to deliver large doses of radiation to a precise area, such as the prostate. Because there are large doses of radiation in each dose, the entire course of treatment is given over just a few days.
SBRT is often known by the names of the machines that deliver the radiation, such as Gamma Knife®, X-Knife®, CyberKnife®, and Clinac®.
The main advantage of SBRT over IMRT is that the treatment takes less time . The side effects, though, are not better. In fact, some research has shown that some side effects might actually be worse with SBRT than with IMRT.
How To Tell If Hormone Therapy Is Working
If you are taking hormone therapy for prostate cancer, you will have regular PSA tests. If hormone therapy is working, your PSA levels will stay the same or may even go down. But, if your PSA levels go up, this may be a sign that the treatment is no longer working. If this happens, your doctor will discuss treatment options with you.
If you are taking hormone therapy for breast cancer, you will have regular check-ups. Checkups usually include an exam of the neck, underarm, chest, and breast areas. You will have regular mammograms, though you probably wont need a mammogram of a reconstructed breast. Your doctor may also order other imaging procedures or lab tests.
Don’t Miss: How Do People Get Prostate Cancer
Types Of Hormone Therapy
The table at the right provides an overview of three commonly used types of hormone therapy. These and others are discussed below. While hormone therapy is commonly used, side effects of the treatment are reported as well. They range from erectile dysfunction, hot flashes, weight gain and loss of bone density.
What Is Prostate Cancer
Prostate cancer is cancer that affects the prostate gland in men. Prostate cancer is the second-leading cause of cancer deaths for men in the US.
Growth in the prostate can be of two types
Prostate cancer starts in the prostate gland and may spread to the nearby areas: lymph nodes, organs, or bones in other parts of the body.
You May Like: Open Mri For Prostate Scan
Managing Side Effects Of Radiation Therapy
Advances in the precision of radiation therapy have lessened the risk of complications. And our doctors are constantly developing new ways to minimize side effects. For example, we are one of the few hospitals in the United States using an FDA-approved biodegradable gel inserted before treatment to protect the rectum.
Still, radiation can cause short- and long-term side effects, including incontinence , erectile dysfunction, bowel problems, fatigue, and symptoms in other parts of the body .
Any side effects you experience depend on which part of the body receives radiation. In the case of such techniques as image-guided radiation therapy and stereotactic radiosurgery, it also depends on which normal structures are in the path of the radiations beam. In addition, radiation therapy is sometimes delivered in combination with hormonal therapy, which can cause impotence. Our experts will work closely with you and your medical team to manage any treatment-related difficulties you may experience, such as bladder, bowel, or erectile dysfunction. However, because of the sophisticated targeting systems we use, severe long-term bladder and bowel problems are now rare.
During the course of radiation treatments, some men experience diarrhea or frequent and uncomfortable urination. Please tell your treatment team if you have any of these problems. We can recommend medications and other methods that can help alleviate these uncomfortable side effects.
Hormone Therapy: Immediate Versus Delayed
Medical Research Council Prostate Cancer Working Party Investigators Group. Immediate Versus Deferred Treatment for Advanced Prostatic Cancer. British Journal of Urology 1997 79:23546. PMID: 9052476.
Messing EM, Manola J, Sarosdy M, et al. Immediate Hormonal Therapy Compared with Observation after Radical Prostatectomy and Pelvic Lymphadenectomy in Men with Node-Positive Prostate Cancer. New England Journal of Medicine 1999 341:17818. PMID: 10588962.
Messing EM, Manola J, Yao J, et al. Immediate Versus Deferred Androgen Deprivation Treatment in Patients with Node-Positive Prostate Cancer after Radical Prostatectomy and Pelvic Lymphadenectomy. Lancet Oncology 2006 7:4729. PMID: 16750497.
Nair B, Wilt T, MacDonald R, Rutks I. Early Versus Deferred Androgen Suppression in the Treatment of Advanced Prostatic Cancer. Cochrane Database of Systematic Reviews 2002 CD003506. PMID: 11869665.
Read Also: How Much Will Clomid Raise Testosterone
You May Like: What Does Prostate Cancer Do
Combining Nadt And Chemotherapy
Pan et al conducted a retrospective review of 3 different therapies in patients with very-high-risk localized prostate cancer: neoadjuvant chemohormonal therapy , in 60 men neoadjuvant hormonal therapy , in 73 men and immediate RP without neoadjuvant therapy , in 44 men. The NCHT group had better biochemical progression-free survival time after surgery compared with the NHT and No-NT groups . After RP, 81% of patients in NCHT group, 73% of patients in NHT group, and 48% of patients in No-NT group achieved an undetectable PSA , despite patients in the NCHT having significantly poorer prognostic factors. Randomized controlled investigations are needed to validate these results, and further follow-up is required.
Multiple phase I/II trials have also been performed to investigate the use of neoadjuvant chemotherapy alone prior to RP, however no patients in these trials achieved a complete pathologic response . As there is currently no evidence demonstrating improved clinical outcomes with the use of neoadjuvant chemotherapy alone or neoadjuvant androgen deprivation therapy alone, future research will likely focus on combined neoadjuvant chemohormonal therapy.
Although no data have yet emerged that definitively support the routine use of neoadjuvant chemohormonal therapy, its safety has been evidenced by several phase I/II clinical trials. Most of the trials on neoadjuvant chemohormonal therapy have investigated docetaxel. These are summarized in Table 4 below.
Different Approaches To Starting Hormone Therapy
Experts debate how early treatment with hormone therapy should be started. Some argue that the benefits of hormone therapy for prostate cancer should be offered to men earlier in the course of the disease. Others assert that there’s little evidence that getting treatment early is better than getting it later.
“Unfortunately, there are still some doctors who are offering hormonal therapy earlier in the course of the disease than is commonly recommended,” Brooks says. Given that the side effects can be serious, Brooks argues that starting treatment with hormone therapy so early may not be a good idea.
However, Holden argues that early treatment may be helpful. “I think one of the reasons that the death rate from prostate cancer is going down is that we’re using hormone therapy early,” he tells WebMD. “We haven’t proved that early treatment improves overall survival yet, but I think we will.”
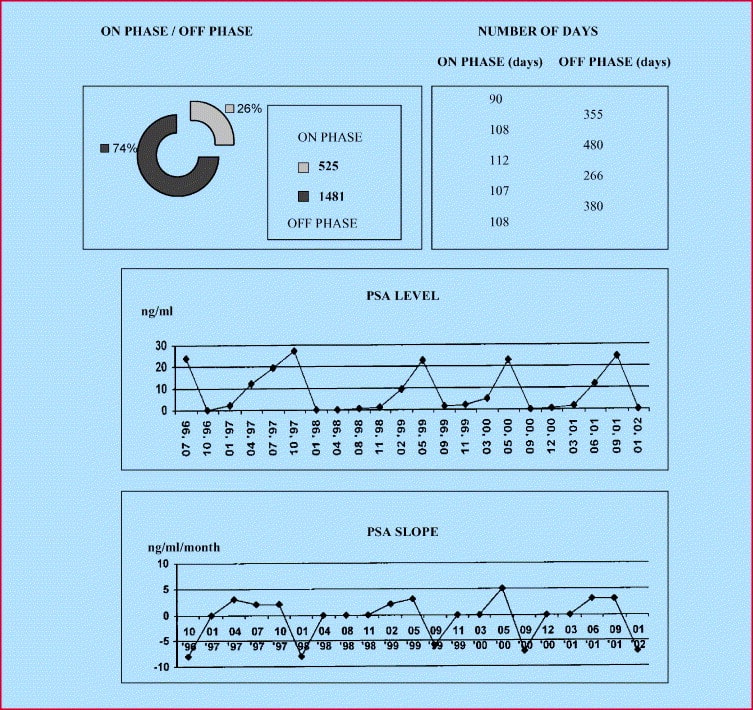
Researchers are also looking at “intermittent therapy,” starting and stopping hormone treatment for months at a time. The big advantage is that men could go off therapy temporarily and thus be free of the side effects. Early study results have been promising.
Recommended Reading: What Are The Different Stages Of Prostate Cancer
Diminution Of Muscular Strength
A mans muscular strength is reduced by 12% to 66% as the result of androgen deprivation. Moreover, muscle mass declines by 20% to 30% by age 70 . Because androgen deprivation reduces the amount of protein synthesis and the non-lipid body mass, obesity results. Thus, elderly patients should actively work against the loss of muscle by directed strength-training exercises .
Psa Responses In Crpc Patients Treated With Ar
Of the 38 patients with CRPC starting AR-targeting therapy, including 32 who had not received any prior treatments, 24 were treated with enzalutamide and 14 were treated with abiraterone. The demographic and clinical characteristics of the patients in the CRPC group are summarized in Table 1. The median follow-up duration was 26 months.
Also Check: Male Prostate Cancer Survival Rates
Figure : How Hormone Therapy Affects The Androgen Cascade
The male sex hormones are known as androgens. Probably the best known hormone in this family is testosterone. Most androgens are produced in the testicles.
Androgens fuel the growth of prostate cells, including prostate cancer cells. Hormone therapy also known as androgen-deprivation therapy seeks to cut off the fuel supply. But different therapies work in different ways.
A. The hypothalamus releases pulses of LHRH, which signals the pituitary gland to release the hormones FSH and LH.
B. LH travels through the bloodstream. When it reaches the testicles, it binds to specialized cells that secrete testosterone into the bloodstream.
C. In the prostate, the enzyme 5-alpha-reductase converts testosterone and other types of androgens into dihydrotestosterone , which stimulates the growth of prostate cells and fuels the growth of cancer, if it is present.
Centrally acting agents
LHRH agonists flood the pituitary gland with messages to crank out LH. This causes a temporary surge of testosterone until receptors in the pituitary are overloaded. Then testosterone levels drop sharply.
The GnRH antagonist jams receptors in the pituitary gland so that it cannot respond to the pulses of LHRH sent by the hypothalamus. This prevents the LH signal from being sent and no testosterone is made in the testicles.
DES inhibits secretion of LHRH from the hypothalamus.
Peripherally acting therapies
Orchiectomy removes the testicles, preventing testosterone production.
How Long Does External Radiation Treatment Take
In most cases the total dose of radiation needed to kill a tumor cant be given all at once. This is because a large dose given one time can cause more damage to nearby normal tissues. This can cause more side effects than giving the same dose over spread out over days or weeks into many treatments.
The total dose of external radiation therapy is usually divided into smaller doses called fractions. Most patients get radiation treatments daily, 5 days a week for 5 to 8 weeks. Weekend rest breaks allow time for normal cells to recover. The total dose of radiation and the number of treatments is based on:
- The size and location of the cancer
- The type of cancer
- The reason for the treatment
- Your general health
- Any other treatments youre getting
Other radiation schedules might be used in certain cases. For instance, radiation therapy might last only a few weeks when its used to relieve symptoms, because the overall dose of radiation needed is lower. In some cases, radiation might be given as 2 or more treatments each day. Or you might have several weeks off in the middle of treatments so your body can recover while the cancer shrinks. Your doctor will talk to you about the best plan in your case.
Read Also: How To Get Rid Of Prostate Infection Naturally
What Is Stereotactic Body Radiation Therapy And What Advantages Does It Offer
Stereotactic body radiation therapy, or SBRT, involves the use of sophisticated image guidance that pinpoints the exact three-dimensional location of a tumor so the radiation can be more precisely delivered to cancer cells. Traditionally, external beam radiation has been delivered in anywhere from 45-48 sessions over multiple weeks. But large, randomized studies have shown that shorter courses of radiation are just as safe and effective. Therefore, at MSK, we have shortened all our radiation courses.
There is increasing interest in giving this radiation in very short courses of treatment using intense radiation doses, called hypofractionated radiation therapy. Many of the people we care for have a type of radiation therapy called MSK PreciseTM. This is a hypofractionated form of SBRT that can be given in five sessions. MSK has been doing this for the past 20 years, and the results in the several hundred people whove been treated have been excellent so far. The treatment is very well tolerated and quite effective
Because of its superior precision, MSK Precise can have fewer side effects than more conventional radiation techniques, with extremely low rates of incontinence and rectal problems. The sexual side effects are low, similar to what is experienced with more extended external radiation techniques. And of course, its much more convenient for patients.
Intermittent Versus Continuous Hormone Therapy
Most prostate cancers treated with hormone therapy become resistant to this treatment over a period of months or years. Some doctors believe that constant androgen suppression might not be needed, so they advise intermittent treatment. This can allow for a break from side effects like decreased energy, sexual problems, and hot flashes.
In one form of intermittent hormone therapy, treatment is stopped once the PSA drops to a very low level. If the PSA level begins to rise, the drugs are started again. Another form of intermittent therapy uses hormone therapy for fixed periods of time for example, 6 months on followed by 6 months off.
At this time, it isnt clear how this approach compares to continuous hormone therapy. Some studies have found that continuous therapy might help men live longer, but other studies have not found such a difference.
Don’t Miss: Proton Beam Therapy For Prostate Cancer At Mayo Clinic
New Prostate Cancer Guideline Offers Shortened Radiation Time
Men being treated for early-stage prostate cancer with external beam radiation therapy can safely choose an option that reduces the number of treatment sessions, according to a panel of experts from the American Society for Radiation Oncology, American Society of Clinical Oncology, and American Urological Association. The new guideline for doctors who treat men with prostate cancer was published October 11, 2018 in Practical Radiation Oncology, Journal of Clinical Oncology, and The Journal of Urology.
Men diagnosed with prostate cancer while its still at an early stage often have several treatment options, including active surveillance , surgery, or radiation. All have about the same cure rates for the earliest stage prostate cancers, although each type of treatment has pros and cons.
External beam radiation therapy , is a type of radiation therapy used to treat prostate cancer. A machine focuses beams of radiation on the prostate gland to kill the cancer cells. Patients typically receive treatments 5 days a week for several weeks. The new guideline uses hypofractionated radiation, where external beam radiation is given in larger doses and fewer treatments. Men treated with this approach can typically expect to complete treatment in 4 to 5 weeks, compared with 8 to 9 weeks for conventional EBRT. Ultrahypofractionated therapy increases the radiation dose even more and can be completed in as few as 5 treatments.
Also Check: What Does Elevated Prostate Levels Mean
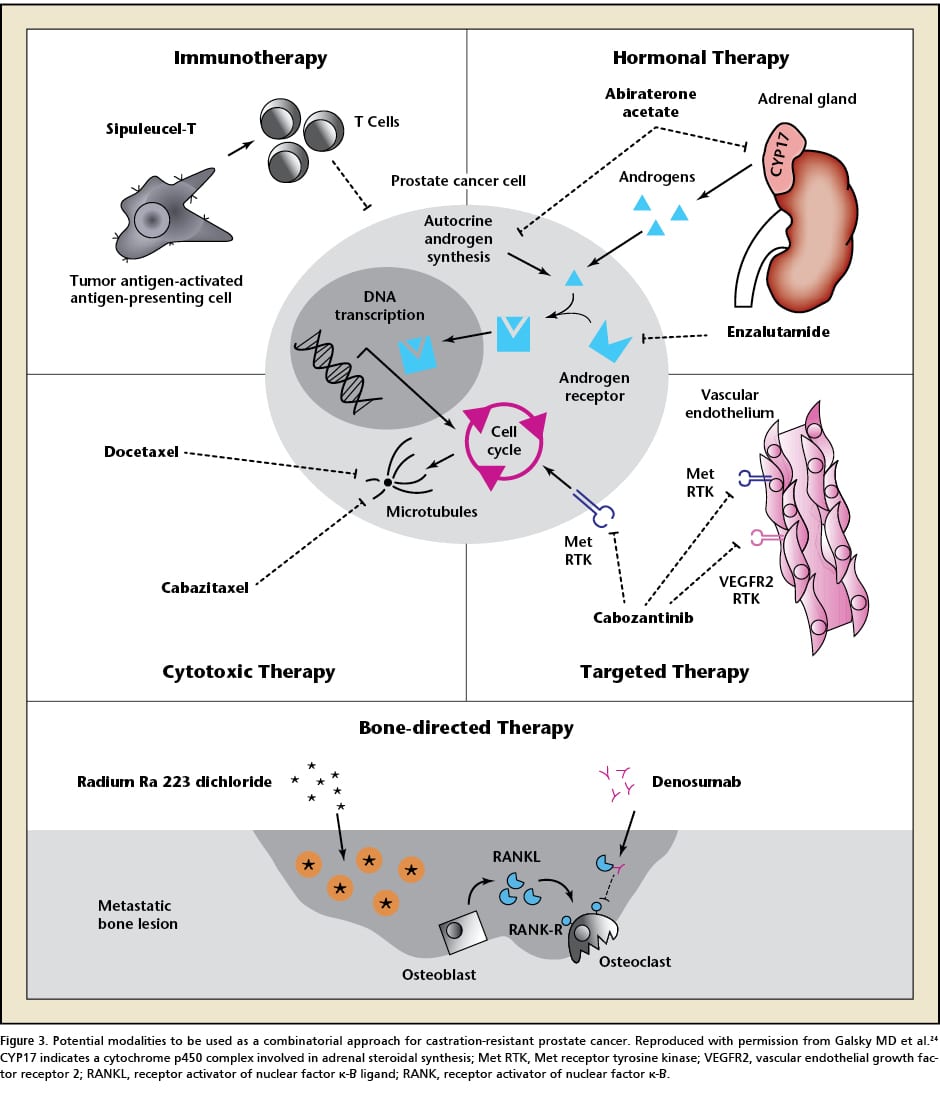
Current Treatment Strategies For Advanced Prostate Cancer
The current hormonal therapeutic armamentarium for advanced prostate cancer is informed by 2 broad approaches: inhibition of conversion of extragonadal precursor steroids to testosterone and DHT with abiraterone and direct blockade of the AR to prevent binding to its ligands, testosterone, and DHT with next-generation AR antagonists such as apalutamide, darolutamide, or enzalutamide .
Recommended Reading: When Should Men Get A Prostate Exam
What Happens After Radiation Therapy Treatment Ends
Once treatment ends, you will have follow-up appointments with the radiation oncologist. Itâs important to continue your follow-up care, which includes:
-
Checking on your recovery
-
Watching for treatment side effects, which may not happen right away
As your body heals, you will need fewer follow-up visits. Ask your doctor for a written record of your treatment. This is a helpful resource as you manage your long-term health care.
