What Are The Benefits Of Salvage Prostate Cryoablation
One benefit of salvage cryoablation of the prostate is that it is a minimally invasive procedure. Many times it does not require a hospital stay. Everyone is different, but you will probably be able to resume normal activity within the first week following the procedure.
Other benefits include:
- Short recovery period.
- Minimal anesthesia.
Salvage cryoablation of the prostate offers another treatment option to men who have failed radiation treatment. In addition, it can be repeated if the first treatment did not completely kill the cancer.
What Is Involved With A Salvage Radiation Procedure
If prostate cancer recurs after a patient has had surgery, salvage radiation is often the next step in treatment. If the recurrence is localized radiation may be able to encompass the area and control the disease. Salvage radiation therapy invloves an external beam of radiation aimed at the prostate bed.
Rising PSA and a high Gleason score following surgery can indicate a recurrence of the disease. The rate of the increase at the time of recurrence can also be an important factor. for more information on options after a prostate cancer recurrence.
Video Transcript
Bryan Wong, MD: Salvage radiation occurs after men have already had prior surgery for the prostate cancer, but have subsequently suffered a recurrence of their disease.
So, the idea behind salvage radiation therapy is that when a patient who has had initial treatment with surgery, they may have suffered recurrence. However, that recurrence might be localized and radiation may be able to encompass the area of recurrence and control the disease.
Salvage radiation often involves external beam radiation to the prostate bed. It is not clear if adding the pelvic nodes as well would be important. Similarly, it is also not clear whether or not adding hormonal therapy to salvage radiation is of clear benefit. Other options for recurrence would also include hormonal therapy.
Single Dose Of Targeted Radiotherapy Is Safe And Effective For Prostate Cancer
- Date:
- European Society for Radiotherapy and Oncology
- Summary:
- A single high dose of radiation that can be delivered directly to the tumor within a few minutes is a safe and effective technique for treating men with low-risk prostate cancer.
A single high dose of radiation that can be delivered directly to the tumour within a few minutes is a safe and effective technique for treating men with low risk prostate cancer, according to a study presented at the ESTRO 38 conference.
Radiotherapy traditionally involves a series of lower dose treatments that take place over several days or week. The new treatment is called high dose-rate brachytherapy and it delivers radiation via a set of tiny tubes.
Researchers say this technique could offer an effective treatment that is convenient for patients and brings potential time and cost savings for hospitals.
The research was presented by Dr Hannah Tharmalingam, a Clinical Research Fellow at Mount Vernon Cancer Centre, Northwood, and The Christie NHS Foundation Trust, Manchester, UK.
The research included 441 men with prostate cancer who were treated at one of seven UK hospitals between 2013 and 2018. Their cancers were classified, depending on how likely they were to spread, as either low risk , medium risk or high risk . All were treated with a single high dose of radiation 166 men also received hormone therapy but none had any surgery or chemotherapy.
Story Source:
You May Like: What Herbs Are Good For Prostate Cancer
What Is The Follow
After three months, you will have a follow-up visit with your healthcare provider. At this time, youll have a PSA test, a blood test that checks for prostate-specific antigen, or PSA, a protein produced by the prostate gland. The PSA test is done to make sure that the treatment worked.
Your healthcare provider will monitor you and suggest a follow-up plan depending on the stage of the cancer and the potential for it to return.
A note from Cleveland Clinic
If youve been treated for prostate cancer and it has come back, your healthcare provider might suggest that you have a salvage cryoablation. Its important to have an honest discussion of the risks and benefits of the procedure and a good understanding of what to expect. Please make sure to ask questions about whatever concerns you. The goal is for you to be able to live longer and live well.
Last reviewed by a Cleveland Clinic medical professional on 08/27/2020.
References
Side Effects And Toxicities Associated With Radiotherapy After Prostatectomy
Radiation treatment is the only potentially curative treatment available for most patients with biochemical failure after RP. However, some would argue that quality of life is as important as survival. Despite the evidence in support of using RT in this setting, the decision to use it must take into account the side effects associated with treatment. There have been multiple reports of acute and late toxicities after post-operative radiation therapy in prostate cancer. Overall, RT appears to be well-tolerated in patients undergoing ART and SRT, and lessons drawn from patients undergoing ART are therefore broadly applicable to SRT.
Peterson et al. reported on late toxicities in 308 postprostatecomy patients who had undergone salvage therapy. In the study, radiation dose ranged from 54.0 to 72.4 Gy with a median dose of 64.8 Gy and was given in 1.8-2.0 Gy fractions. Median follow-up from the end of treatment was 60 months. Thirteen percent of patients reported late complications, but only an estimated 0.7% of patients would experience severe toxicities by 5 years. Among those reported in the study were grade 3 cystitis and grade 4 rectal complications. These results are consistent with those of other reports, including data from the three recently randomized trials on ART.
Don’t Miss: Does The Prostate Keep Growing
Radiation Dose Enough For Some Prostate Cancers
HealthDay Reporter
TUESDAY, April 30, 2019 Treating men with low-risk prostate cancer with just one high dose of radiation may be safe and effective, British researchers report.
Therapy for prostate cancer typically involves low-dose radiation given over several days or weeks. Conversely, high-dose radiation is given once through a set of tiny tubes inserted directly into the tumor.
For low-risk patients, a single dose of high-dose radiation is sufficient, but for medium- and high-risk patients, a single dose of 19 Gy isnt enough. They will likely need a bigger dose or going back to multiple doses, said lead researcher Hannah Tharmalingam. Shes a clinical research fellow at the Mount Vernon Cancer Centre in Northwood, England.
According to Tharmalingam, high-dose radiation could be more convenient for low-risk patients, and less time-consuming and costly for the medical system.
But one radiation oncologist fears that the side effects make it potentially dangerous.
For the study, Tharmalingam and her colleagues treated 441 prostate cancer patients between 2013 and 2018. The cancers were classified as low-, medium- or high-risk.
All of the men were treated with one high dose of 19 Gy of radiation, which is equivalent to the total amount of radiation given over several days with current treatments, Tharmalingam said.
In addition, 166 men were also given hormone therapy. None of the men, however, had surgery or chemotherapy.
Continued
Oncological Outcomes
Stereotactic Body Radiation Therapy
This technique uses advanced image guided techniques to deliver large doses of radiation to a precise area, such as the prostate. Because there are large doses of radiation in each dose, the entire course of treatment is given over just a few days.
SBRT is often known by the names of the machines that deliver the radiation, such as Gamma Knife, X-Knife, CyberKnife, and Clinac.
The main advantage of SBRT over IMRT is that the treatment takes less time . The side effects, though, are not better. In fact, some research has shown that some side effects might actually be worse with SBRT than with IMRT.
Don’t Miss: How To Check If My Prostate Is Enlarged
Treating Prostate Cancer That Doesnt Go Away Or Comes Back After Treatment
If your prostate-specific antigen blood level or another test shows that your prostate cancer has not been cured or has come back after the initial treatment, further treatment can often still be helpful. Follow-up treatment will depend on where the cancer is thought to be and what treatment you’ve already had. Imaging tests such as CT, MRI, or bone scans may be done to get a better idea about where the cancer is.
New Kids On The Block
Recently, the use of new molecular imaging has increasingly changed the management of patients after radical prostatectomy. Choline positron emission tomography-computed tomography was the first gamechanger. Different retrospective studies , , , ] showed that using choline PET-CT changed the management in 33% of prostate cancer patients with biochemical recurrence. Gallium Ga 68-labelled prostate-specific membrane antigen PET-CT is even more
Also Check: How Long After Prostate Biopsy Can You Ejaculate
What Happens To The Prostate After Radiation
The entire prostate gland is radiated when we treat the cancer. The prostate normally produces some of the fluid in the ejaculation. Radiation therapy has the side effect of damaging the glands in the prostate, so a lot less fluid is produced. The ejaculation may be dry or nearly dry. In addition, you will probably be sterile after radiation, but this is not 100% guaranteed and should not be relied upon as a form of birth control. You can still usually have erections because the nerves and blood vessels that go to the penis are not as damaged as the prostate gland.
The prostate gland will end up having a lot of scar tissue. It will shrink in size to about half its original weight within a couple years after finishing radiation. The urethra passes through the canter of the prostate gland like the hole of a doughnut. Sometimes this passage can widen, other times it can shrink after radiation. In summary, the prostate gland is heavily damaged from radiation and does not work normally afterwards.
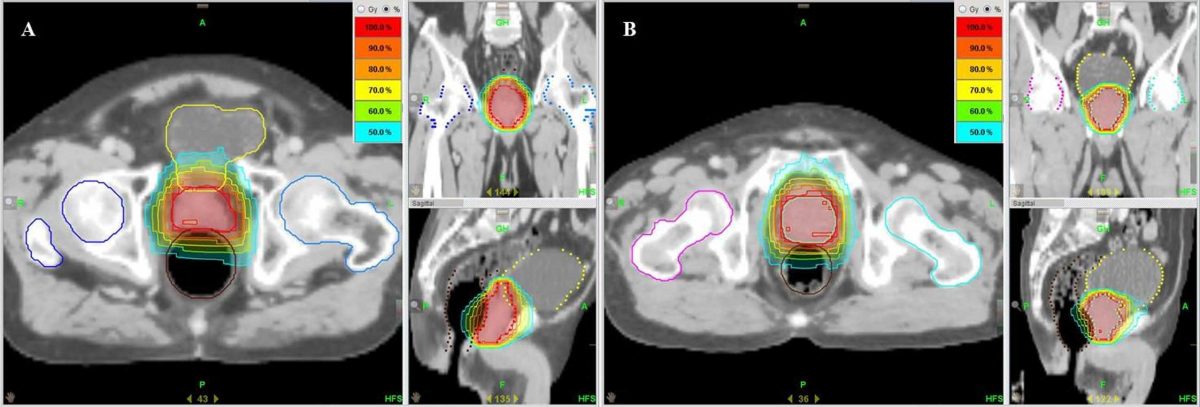
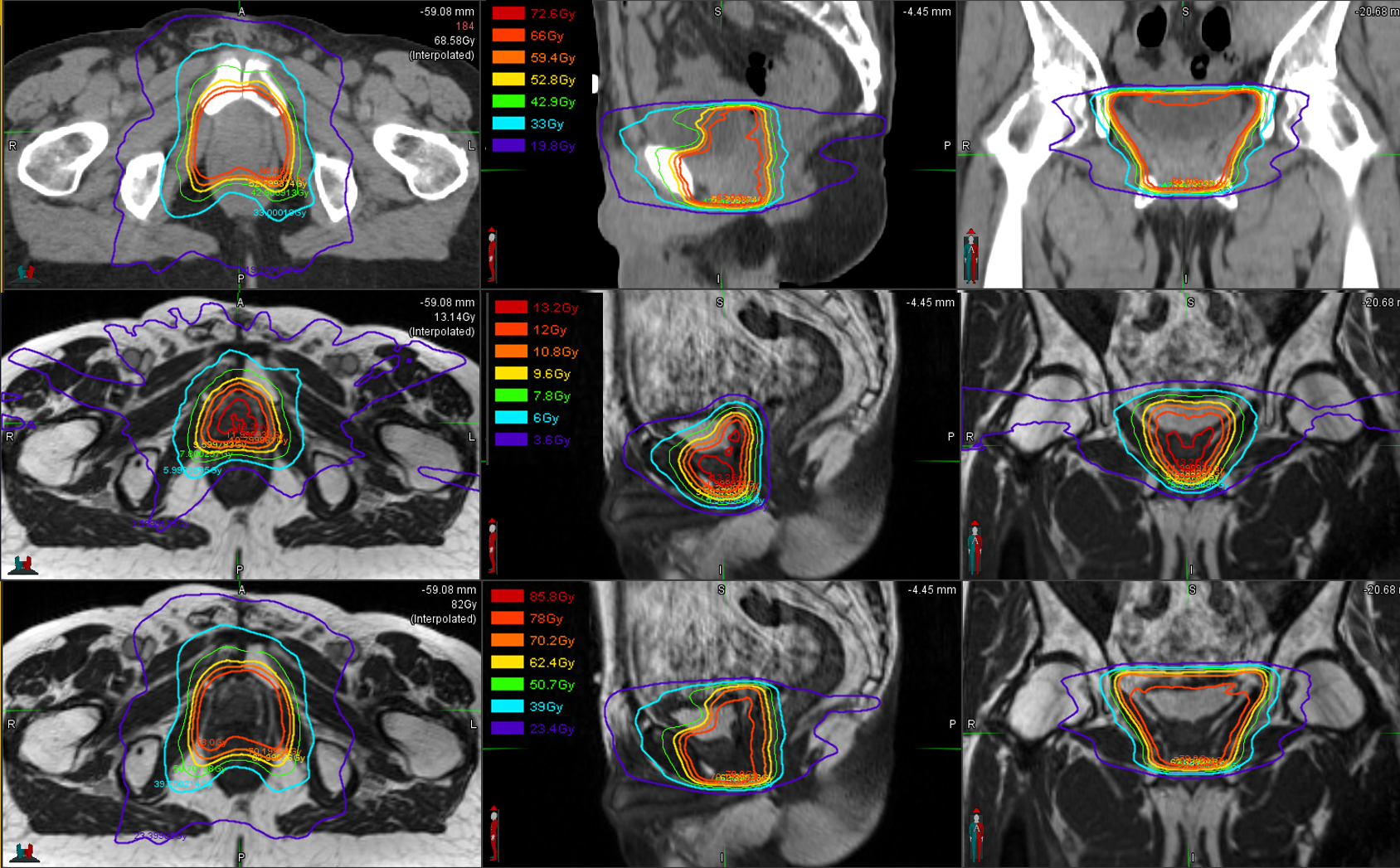
Intensity Modulated Radiation Therapy
IMRT, an advanced form of 3D-CRT therapy, is the most common type of external beam radiation therapy for prostate cancer. It uses a computer-driven machine that moves around the patient as it delivers radiation. Along with shaping the beams and aiming them at the prostate from several angles, the intensity of the beams can be adjusted to limit the doses of radiation reaching nearby normal tissues. This lets doctors deliver an even higher radiation dose to the cancer.
Some newer radiation machines have imaging scanners built into them. This advance, known as image guided radiation therapy , lets the doctor take pictures of the prostate just before giving the radiation to make minor adjustments in aiming. This appears to help deliver the radiation even more precisely and results in fewer side effects.
A variation of IMRT is called volumetric modulated arc therapy . It uses a machine that delivers radiation quickly as it rotates once around the body. This allows each treatment to be given over just a few minutes. Although this can be more convenient for the patient, it hasnt yet been shown to be more effective than regular IMRT.
You May Like: Can You Get Prostate Cancer From Not Masturbating
Salvage External Beam Radiotherapy For Prostate Cancer After Radical Prostatectomy
James B. Yu, MD, MHSOncology
This article defines the biochemical recurrence of prostate cancer, distinguish SRT from ART, outline the evidence for SRT, and makes recommendations with regard to radiotherapy volume and dose.
Prostate cancer is the second most common cause of cancer death in American men. What to do when prostate cancer recurs months or years after a patient undergoes radical prostatectomy is an area of active research. Patients who underwent radical prostatectomy without immediate adjuvant radiation therapy but subsequently have evidence of recurrent disease are candidates for Salvage Radiation Therapy . Though there are three prospective randomized trials illustrating the efficacy of post-operative ART for selected patients, similarly strong evidence is lacking for SRT. In this article, we define the biochemical recurrence of prostate cancer, distinguish SRT from ART, outline the evidence for SRT, and make recommendations with regard to radiotherapy volume and dose. We discuss the known side effects from SRT, weigh the cost and benefit of SRT, and discuss possible tools that may improve the cost/benefit ratio for SRT by helping to select patients whom SRT may be more likely to benefit.
What Is Salvage Prostate Cryoablation
Salvage cryoablation of the prostate is a procedure recommended for prostate cancer that has returned in men who have been treated previously.
Salvage literally means save. The doctor is trying to save the patient from the cancer. The procedure uses cryoablation, or extreme cold, to freeze the prostate, so that the cancer cells within it will freeze and die. It is also called cryosurgery or cryotherapy.
The procedure is typically done on an outpatient basis and is minimally invasive.
Recommended Reading: Why Does The Prostate Get Enlarged
What Are The Complications Of Salvage Prostate Cryoablation
You might experience these types of complications:
- Swelling of the scrotum.
- Urinary urgency and increased urinary frequency.
- Pelvic or rectal pain.
Rarely, the procedure may also risk injury to surrounding tissues such as the rectum or bladder because of the nearby location of these structures.
Another rare complication is the potential for the patient to develop a fistula, an abnormal opening that connects the urethra and the rectum. The fistula may cause the patient to have diarrhea from urine in the rectum. It may also cause infection from bacteria in the bladder.
Stereotactic Body Radiation Therapy Or Stereotactic Ablative Radiation Therapy
Guided by advanced imaging techniques, SBRT delivers large doses of radiation over a short period of time to a precise area. SBRT is commonly referred to by the names of the machines used to deliver the radiation. SBRT can offer some patients with localized prostate cancer the convenience of fewer treatments while maintaining treatment effectiveness and safety. SBRT may also be used to treat metastases for some patients to reduce tumor mass and potentially enhance survival.
You May Like: What Are The Chances Of Prostate Cancer Recurrence
Also Check: How To Screen For Prostate Cancer
Modern Imaging Modalities In Prostate Cancer: Pet/ct
The benefit to performing local treatment such as RT is critically dependent upon imaging methods and its accuracy to assess disease at local, nodal, and metastatic level . Traditionally, computed tomography and bone scintigraphy have been used for both staging and follow-up of patients with prostate cancer, yet they often lead to understaging. Indeed, CT was shown to have a 32% sensitivity only in detecting nodal metastases in a meta-analysis led by Hövels et al. , with both sensitivity and specificity dropping precipitously at low PSA levels, when indication for SRT is usually undertaken. Bone scintigraphy remains the standard for the detection of bone lesions, but pooled results from a meta-analysis revealed a sensitivity and specificity of 59 and 75%, respectively .
18F-Fluciclovine PET/CT is also indicated at BCR, after primary treatment with curative intent . It has the ability to detect amino acid transport, which is upregulated in numerous types of cancer cells . Fluciclovine PET/CT was found to be both more sensitive and more specific than choline PET/CT , and thus received approval by the Food and Drug Administration in the recurrent setting. In the phase III FALCON trial, the detection rate of Fluciclovine was 56% at a median PSA level at restaging of 0.79 ng/ml .
Randomized Phase Ii Trial Of Salvage Radiotherapy For Prostate Cancer In 4 Weeks V 2 Weeks
Clinical Trial Details
The purpose of this study is to compare urinary and bowel side effects of hypofractionated radiotherapy in 20 treatments to ultra- hypofractionated radiotherapy in 5 treatments for prostate cancer that has returned after prostatectomy.
Learn more about the trial details in this informational video:
Total numerical dose differs in each arm but is considered biologically equivalent to each other and protracted fractionated radiotherapy .The investigators are also interested in looking at progression-free survival and the quality of life . The standard treatment for men with detectable PSA after radical prostatectomy is salvage radiotherapy . Salvage radiotherapy delays the need for chronic, non-curative treatment, such as long-term androgen suppression, and is the only potentially curative treatment of some biochemical recurrences after prostatectomy. Standard treatment regimens range from 20-40 treatments.
Patients are recommended to undergo salvage radiotherapy delivered over many weeks, representing a high burden of therapy. Modern radiotherapy has been afforded many advantages including advanced image-guided radiotherapy allowing for larger dose delivery in fewer treatments and smaller margins with hypofractionated and ultra-hypofractionated radiotherapy. In patients that need salvage radiotherapy, the potential advantages of hypofractionated and ultrahypofractionated radiotherapy delivered over 20 or 5 treatments are:
Inclusion Criteria
Recommended Reading: Docetaxel Chemotherapy For Prostate Cancer
Exclusion Criteria In Phase 3 Trials Of Salvage Rt
Given the lack of universally-accepted criteria regarding the contraindications of SRT, in Table Table33 we provide a summary of the exclusion criteria used in the phase 3 RCTs that have evaluated SRT with and without ADT. That table also includes the exclusion criteria in currently ongoing studies comparing adjuvant RT to SRT. Based on those data, we have developed a decision algorithm to identify patients considered “unfit” for SRT .1). As with most therapeutic indications, it is important not only to define the patients who are likely to benefit from a given treatment, but also to identify those patients in whom treatment could reduce life expectancy and/or lead to complications without providing a clear clinical benefit. Patients considered unfit for SRT would therefore include those who meet several of the following criteria: > 75 years of age Significant comorbidities Poor baseline urinary function Low risk of developing BCR and Unfavourable DVH values. These patients should be offered alternative approaches, which may include surveillance or hormonal therapy depending on the patients individual characteristics, life expectancy, and the “aggressiveness” of the recurrent disease. Finally, in patients with PSA > 1 ng/mL and/or PSADT < 6 mo, SRT should not be performed until the recurrence has been localized on imaging tests or at least until distant metastasis has been ruled out.
