Neuroendocrine Secretory Profiles Are Abnormal In Most Mcrpc Patients
In the total study population, pretreatment serum levels of progastrin-releasing peptide, NSE, and CgA were abnormal in 80%, 88%, and 74% of patients, respectively. In the subgroup of patients without potential influencing factors, pretreatment serum levels of progastrin-releasing peptide, NSE, and CgA were abnormal in 76%, 90%, and 59% of patients, respectively, and demonstrated marked interindividual variability . Neuroendocrine markers were not associated with Gleason scores or previous therapies besides second-line chemotherapy with cabazitaxel . Last, neuroendocrine marker levels did not significantly differ between patients with and patients without lymph node metastases on 68Ga-PSMA-ligand PET/CT before RLT , between patients with and patients without bone metastases , or between patients with and patients without hepatic metastases .
Molecular Components Driving Ned In Prostate Cancer
In the last years, the molecular components involved in the NE differentiation of prostate cancer have been highly studied. Several molecular signatures have been implicated in prostate cancer with NED .
Table 2
Some studies show that Rb loss underlies the development of NED in prostate cancer . Rb is encoded by the human retinoblastoma gene RB1 that was initially cloned from children with a rare form of eye cancer of the same name. RB is a negative regulator of the cell cycle and has been found to be inactivated in a wide range of human cancers . By immunohistochemistry assay, studies showed that loss of Rb occurred almost universally in prostatic small cell carcinomas. In contrast, loss of this tumor suppressor occurs rarely in conventional high-grade acinar prostate tumors, acinar carcinomas with NED, and castrate-resistant prostate carcinomas . These data suggest that Rb loss is a critical event in the development of small cell carcinomas and may be a useful diagnostic and potential therapeutic target.
Furthermore, CD44, a major cell-surface receptor for hyaluronic acid and mediates epithelial cell adhesion by its involvement in cell-cell and cell-matrix interactions, has been shown strong and diffuse membrane staining by IHC in 100% of the prostatic small cell carcinoma, whereas in usual prostatic adenocarcinomas only rare positive scattered tumor cells are CD44 positive .
Post Hormone Therapy And Androgen Resistance
Histologically focal neuroendocrine differentiation ranges from 10 to 100% in prostate adenocarcinomas treated by ADT . It is unclear if the morphologic pattern and appearance of neuroendocrine differentiation varies based on the type of anti-androgen regimen. It has been suggested that after failing primary ADT in metastatic castration-resistant PCa, assessing evidence and the possible degree of PCND may prove valuable in predicting the success of continued androgen receptor targeted therapies . More importantly, given the rise and progress in molecular pathology particularly in fields such as pulmonary adenocarcinomas, it is of great current interest to know any molecular variations in post ADT neuroendocrine differentiation and pure NEPC. This level of molecular analysis could provide a greater understanding of androgen resistance and may help better classify post ADT pathologies.
Read Also: How To Reduce Your Chances Of Getting Prostate Cancer
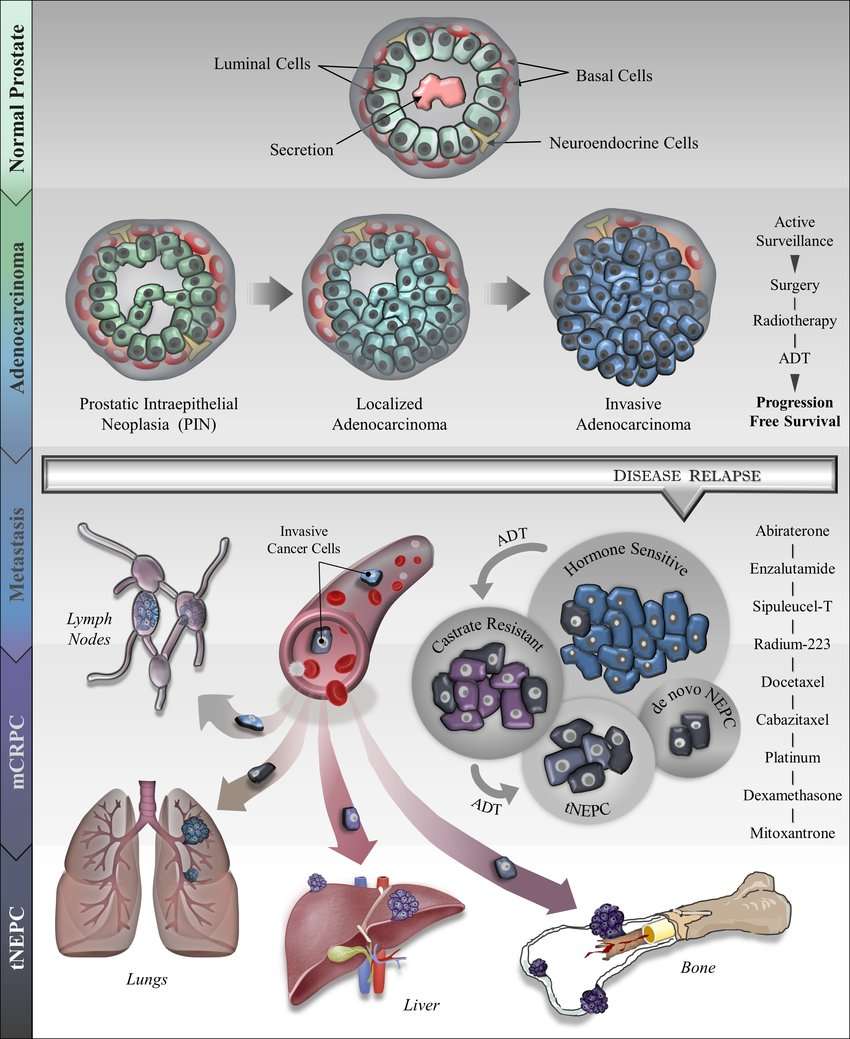
Emergence Of The Neuroendocrine Subtype
Potent hormone therapies like abiraterone and enzalutamide can be effective treatments for men with castrate-resistant prostate cancer. However, almost all men eventually develop drug resistance to these agents.
In some cases, the drug-resistant cancer may look and behave differently than the original cancer, so much so that it is considered a different subtype of the disease. For example, some men who were originally diagnosed with adenocarcinoma prostate cancer develop t-SCNC after treatment with abiraterone or enzalutamide.
Under the microscope, t-SCNC looks quite different from adenocarcinoma: the cells are smaller and more crowded together. And compared to adenocarcinoma prostate tumors, tumors of the t-SCNC subtype are thought to have less hormone signaling and lower prostate-specific antigen.
In addition, t-SCNC shares some features with a small-cell neuroendocrine subtype of prostate cancer that appears in less than 1% of men with newly diagnosed prostate cancer.
To understand how frequently t-SCNC develops after hormone treatment, Dr. Aggarwal and his colleagues analyzed metastatic tumor samples from 202 men with castrate-resistant prostate cancer who had received treatment at multiple institutions. The samples were obtained from metastatic tumors in the bone, lymph nodes, liver, or other soft tissues.
The anatomical site where the metastatic tumor sample had been taken did not appear to affect the frequency of the neuroendocrine subtype, the researchers found.
Predominant Dysregulation Of Mirna Isoforms In Evs From Nepc
Notably, a significant representation of miRNA isoforms was observed in EVs, with a significant alteration in expression of a set of 170 iso-miRs . Top significantly upregulated iso-miRs included those of miR-92b, -423, -10b, -10a, -877, -92a-1, -92-a2, 99b and downregulated miRs had a significant representation of isoforms of miR-143 and miR-145. Figure B represents the miRNA loci producing3 differentially expressed iso-miRs with the predominance of iso-miRs from miR-92b, miR-423, miR-10a, miR-10b and miR-877. Iso-miRs were found to range in length from 14 to 24 nucleotides , with the majority of iso-miRs at 18-21nt. Interestingly, all the isoforms represented in EVs differ from native mature miRNAs in their 3 regions with the seed sequence same as that of corresponding native miRNA.
Figure 2
Predominant dysregulation of miRNA isoforms in EVs from NEPC. Heat map showing differentially expressed iso-miRs in EVs from CRPC-adeno cases as compared to CRPC-NE . Heat map was generated by using R studio software, Version 1.1.463 . miRNA loci producing3 differentially expressed iso-miRs in sequenced samples plotted as a function of number of observed iso-miRs. Range of length of differentially expressed iso-miRs and their abundance across sequenced EV miRNAs extracted from CRPC-Adeno and CRPC-NE samples.
Also Check: Can A Man Get An Erection After Prostate Removal
Prostate Cancer Treatment May Rewire Tumor Engine Potentially Increasing Aggressiveness
Prostate cancer cell, coloured scanning electron micrograph .
A study by researchers at the University of Michigan Rogel Cancer Center suggests that androgen receptor inhibitor drugs, such as enzalutamide can fundamentally rewire and reshape how prostate tumors function, and in certain cases even make them more aggressive. The team carried out gene expression profiling of biopsies of metastatic castration-resistant prostate cancer from men prior to treatment using enza, and also at progression. Their analyses indicated evidence of lineage plasticity, and also identified a gene signature, which they have yet to validate, associated with a risk of therapy-induced lineage plasticity and poor patient survival.
The study was led by Joshi Alumkal, MD, Wicha Family Professor of Oncology and Professor of Internal Medicine at the Rogel Cancer Center, in collaboration with the lab of Zheng Xia, PhD, at the Oregon Health & Sciences University Knight Cancer Institute. Alumkal told GEN, Our results demonstrate that in approximately 15% of cases, tumor lose reliance on the original target of the drug enzalutamidethe androgen receptor. Our results also suggest there may be baseline gene expression changes that allow one to predict that this deadly form of resistance called lineage plasticity, or differentiation change, may happen with enzalutamide treatment.
Treatment Response And Early Progression
Treatment response was determined according to the criteria of the Prostate Cancer Clinical Trials Working Group 2 , defined as at least a 50% serum PSA decline from baseline, with confirmation 34 wk apart, and absence of new metastases on a 68Ga-PSMA-11 PET/CT scan obtained after 2 cycles. Progression was defined as a PSA increase of 25% or more and an absolute increase of 2 ng/mL or more from the nadir or the appearance of new metastases on PET/CT images. The PSA response rate and the percentage PSA decline after 2 cycles were documented. In patients who discontinued RLT , the PSA level at the termination of therapy was used for further analyses. For calculation of progression-free survival, patients were followed for 125 d after the first RLT .
Recommended Reading: How Do You Treat A Prostate Infection
Inducers Of The Neuroendocrine Phenotype In Prostate Cancer
A number of signaling molecules have been shown to trigger the development of neuroendocrine features in prostate adenocarcinoma cells in vitro. Androgen-deprivation therapy affects the expression of epithelial markers with a decrease in E-cadherin and gain of mesenchymal markers, such as N-cadherin, vimentin, Zeb1, Twist1, and Snail2 , toward an epithelial-mesenchymal transition -like state. LNCaP cells transfected with Snail undergo neuroendocrine differentiation with neurite-like morphologic characteristics and increased levels of classical NE markers such as neuron specific enolase and chromogranin A subsequent knockdown of Snail in these cells can revert this phenotype . Similar to ADT, loss or silencing of the AR itself with small interfering RNA may also trigger NE properties to LNCaP cells .
Hypoxia is a characteristic feature of advanced solid tumors and strongly associates with malignant tumor progression and resistance to chemotherapy. Studies have suggested that hypoxia facilitates the malignancy of prostate adenocarcinoma cells by increasing androgen-independence . Other reports show that hypoxia can induce neuroendocrine programs through down-regulation of Notch signaling . Hypoxia down-regulates both PTEN and REST in prostate cancer epithelia inducing expression of neuronal genes and microRNAs associated with neuroendocrine reprogramming .
Pros And Cons Of Mirnas In Therapeutics
Dysregulation of miRNA expression has been implicated in several cancers. Treatments based on miRNAs have been fully explored and due to their ability to regulate a wide array of genes by targeting many mRNAs, they can be effective in the control of cancers, thereby having some added advantage over conventional drugs. In addition, it is easy to design these miRNA such as miRNA mimics, and these miRNA-based drugs can also be highly specific and potent. Another advantage of miRNA-based drugs is their small molecular size and low cost of synthesis. A major drawback in miRNA-based therapy is with drug delivery nucleases in serum and cells of the immune system degrade these exposed miRNAs when systematically injected. In addition, due to the fact that miRNAs can target myriad genes, there is a problem of off-target effects which can be lethal to non-targeted cells.
You May Like: Does Prostate Cancer Affect Libido
Clinical Characteristics Treatment Outcomes And Potential Novel Therapeutic Options For Patients With Neuroendocrine Carcinoma Of The Prostate
Metrics: PDF 1577 views | Full Text 3120 views | ?
Leonidas Apostolidis , Cathleen Nientiedt, Eva Caroline Winkler, Anne Katrin Berger, Clemens Kratochwil, Annette Kaiser, Anne-Sophie Becker, Dirk Jäger, Markus Hohenfellner, Clemens Hüttenbrink, Sascha Pahernik, Florian A. Distler and Carsten Grüllich
Neuroendocrine Cells In Benign Prostate
Prostate is a glandular organ in which the epithelial cells form glands or ducts. Under the light microscope, two types of epithelial cells are easily identifiable in the prostate: secretory cells that produce secreted proteins including prostate-specific antigen and basal cells that likely function as reserve cells. There is a third, minor epithelial cell type called neuroendocrine cells that are scattered among the basal and luminal cells and constitute 1% of the total epithelial cell population.1,2,3 The NE cells can be identified by electron microscopy showing distinct ultrastructural morphology and intracytoplasmic dense-core secretory granules. More commonly, they are detected by immunohistochemistry with antibodies against NE markers such as Chromogranin A or Synaptophysin with the former being more sensitive and specific.1,2,3 In mice, NE cells are concentrated around the proximal urethra while not commonly seen in the various lobes of the prostate. Since NE cells are present in every single benign human prostate, they are presumed to play important roles in prostate development or function. However, little experimental evidence exists that provides significant insights into their function.
Recommended Reading: Cancer Of The Prostate Gland
Large Cell Neuroendocrine Carcinoma
Large cell neuroendocrine carcinoma is characterized by cells arranged in nests with peripheral palisading, abundant cytoplasm, vesicular nuclei and prominent nucleoli. The tumor cells themselves are much larger than those of small cell carcinoma and conventional prostatic adenocarcinoma cells. Neuroendocrine features such as fine chromatin in the tumor cells can be appreciated variably. Often geographic necrosis is seen and it is a very helpful histologic feature in this tumor type. Neuroendocrine differentiation in large cell neuroendocrine carcinoma is often demonstrated by extensive staining of at least one NEC biomarker . Large cell neuroendocrine carcinomas are extremely rare in pure form and typically follow long term hormonal therapy with an average survival of 7 months . Evans et al described the only study on LCNC with 7 total cases of which six presented after long standing ADT. LCNC have also been described in association with PCa and SCC. Large cell neuroendocrine carcinoma of the prostate is a high grade malignancy, its aggressive biological is very similar to that of small cell carcinoma of the prostate.
Large cell neuroendocrine carcinoma of the prostate shows typical salt-and-pepper chromatin patterns, but the tumor cells are much larger than the ones in small cell carcinoma . Neuroendocrine marker such as chromogranin is necessary.
Adenocarcinoma With Neuroendocrine Differentiation
Neuroendocrine differentiation is present at least focally in virtually all cases of prostatic adenocarcinoma, although the number of cells varies according to the tissue fixative employed, the antibody and the method of staining used, and the number of tissue sections examined.641664 Abrahamsson and colleagues identified neuroendocrine-immunoreactive cells in 92% of prostate cancers fixed in formalin and embedded routinely in paraffin.659,662,663 Aprikian and associates665 found neuroendocrine cells in 77% of untreated prostate cancers, 60% of hormone-refractory cancers, and 52% of metastases, with a small number of dispersed positive cells in each of these cases.
Neuroendocrine differentiation typically consists of scattered cells that are inapparent by light microscopy but revealed by immunoreactivity for one or more markers. Chromogranin and serotonin are the best markers of neuroendocrine cells in formalin-fixed sections of the prostate . Neuroendocrine cells in cancer are malignant, and lack androgen receptor expression. Neoplastic neuroendocrine cells devoid of nuclear androgen receptors constitute an androgen-insensitive cell population in prostate cancer. The absence of proliferative and apoptotic activity may endow these tumor cells with relative resistance to cytotoxic drugs and radiation therapy.666
About 10% of adenocarcinomas contain unique neuroendocrine cells with distinctive large eosinophilic granules .
Gavin C Harris, … Frances P O’Malley, in, 2006
Read Also: Rezum Steam Treatment For Prostate
Small Cell Carcinoma And Carcinoid Tumors
Pure small cell carcinomas of the prostate are rare and accounts for no more than 1 percent of all carcinomas of the prostate. Similar to small cell carcinoma of other organs, they are aggressive tumors and often present as locally advanced or metastatic diseases . Occasionally they are associated with paraneoplastic syndromes . Sometimes, small cell carcinomas can occur in patients who have received hormonal therapy for conventional adenocarcinomas of the prostate .
More commonly, small cell carcinoma is seen as a component of mixed tumors which also contain conventional adenocarcinoma. Histologically, small cell carcinomas of the prostate are similar to the more common small cell carcinomas of the lung and are characterized by a solid, sheet-like growth pattern. Tumor necrosis is common. Tumor cells are small, with fine chromatin, scant cytoplasm, and nuclear molding. Mitotic figures, apoptotic figures and crush artifact are frequently observed .
Small cell carcinoma of the prostate. In comparison to adenocarcinoma, such tumor shows sheet-like growth pattern with frequent mitotic figures and apoptotic figures. Tumor cells have scanty cytoplasm, high N/C ratio, fine chromatin pattern and nuclear molding.
Small cell carcinoma is a rapidly growing tumor which disseminates early and the prognosis is poor . Hormonal therapy is not effective in treating such tumors while chemotherapy may have some value .
Incidence Of Nepc And Avpc
NEPC is rarely diagnosed de novo in its pure form , but about 10-17% of patients with metastatic CRPC have been reported to progress with t-NEPC when treated with NHA . Increased therapeutic pressure on the AR signaling pathway due to broad implementation of NHA is assumed to be causative for a rising number of t-NEPC. For example, Abida et al. described an increase of NEPC in mCRPC tissue biopsies from NHA-treated patients compared to NHA-naïve patients . Along with the approval of abiraterone and enzalutamide an increased incidence of patients with NE+ tumors from 6.3% in the time period from 1998 to 2011 to 13.3% in 2012-2016 was reported . Of note, a rising age-adjusted incidence rate of NEPC was also observed in the years 2004-2011 suggesting other factors to promote this phenomenon .
To date, most data are available on NEPC while double negative tumors are still poorly understood. Therefore, this review will focus on the molecular mechanisms and signaling pathways that have been described to contribute to the development of t-NEPC. Key aberrations found in t-NEPC are introduced and interactions potentially involved in the emergence of NE features are highlighted.
Recommended Reading: Is Stage 4 Prostate Cancer A Death Sentence
Origin And Biological Function Of Neuroendocrine Cells
NE cells are present in benign and malignant glands of the prostate, representing 1% of the epithelial cell population. They are considered terminally differentiated distributed in all anatomic zones, with higher concentrations in the transitional and peripheral zones compared with the central zone. The cellular origin of NE cells has not been firmly established. It has been hypothesized that NE cells may arise in the neural crest and migrate to the prostatic epithelium because of the observed appearance of CgA + cells in the paraganglia of future prostatic mesenchyme and eventual dispersion in urogenital mesenchyme. With the sprouting and development of prostatic analgen from the urogenital epithelium, it is thought that NE cells migrate to the basal layer of the mature glands where they are then commonly observed. However, more recent studies have shown strong evidence that NE cells are the progeny of basal cells as NE cells express basal-specific keratins and their differentiation from human pluripotent basal cells has been well demonstrated in vitro., In an in vivo study, Goldstein et al. showed that primary benign human prostate basal cells can be transformed into acinar-type adenocarcinoma-containing NE cells, providing strong evidence that NE cells may be derived from benign basal cells of the prostate.
Cell Lines And Cell Culture
NCI-H660 cell line was obtained from the American Type Culture Collection and cultured under recommended conditions in HITEs media supplemented with 5% FBS, and 1% penicillin/streptomycin. LNCaP-AR and LNCaP-AR-enz resistant cell lines were a kind gift from Dr. Felix Feng at UCSF and were maintained in RPMI 1640 media each supplemented with 10% fetal bovine serum and 1% penicillin/streptomycin. Enz resistant cells were cultured in presence of 50 µM enzalutamide . All cell lines were maintained in an incubator with a humidified atmosphere of 95% air and 5% CO2 at 37 °C.
Recommended Reading: Does An Enlarged Prostate Affect A Man Sexually
