Transcriptional Profiling Of Matched Patient Biopsies Clarifies Molecular Determinants Of Enzalutamide
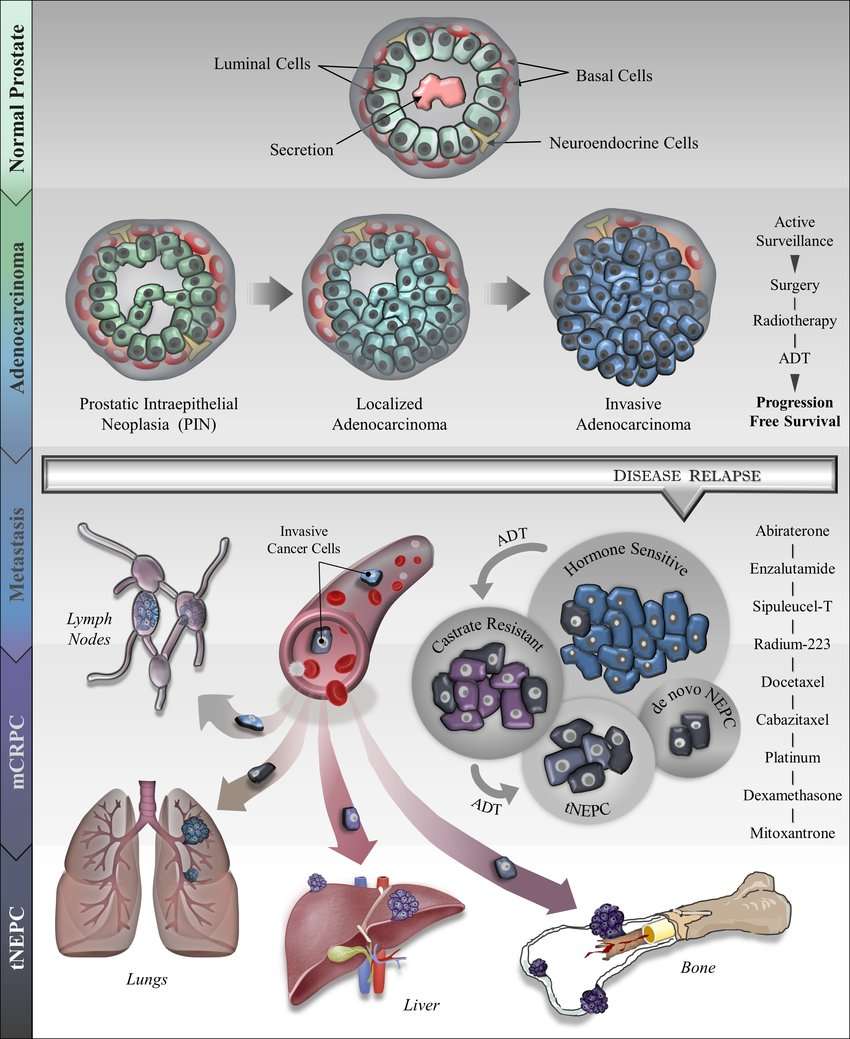
Lineage plasticity is increasingly recognized as an emergent resistance mechanism after treatment with androgen receptor signalling inhibitors. To understand determinants of resistance, the authors analyzed the transcriptomes of patient tumor biopsies before enzalutamide treatment and at progression and identified a gene expression program associated with lineage plasticity risk and poor outcomes.
Improving Biopsies For Prostate Cancer
Traditionally, prostate cancer has been diagnosed using needles inserted into the prostate gland in several places under the guidance of transrectal ultrasound imaging to collect samples of tissue. This approach is called systematic biopsy.
However, ultrasound does not generally show the location of cancer within the prostate. It is mainly used to make sure the biopsy needles go into the gland safely. Therefore, biopsy samples using ultrasound guidance can miss cancer altogether, or identify low-grade cancer while missing areas of high-grade, potentially more aggressive cancers.
Some doctors, concerned that a systematic biopsy showing only low-grade cancer could have missed a high-grade cancer, may suggest surgery or radiation. However these treatments are for a cancer that may have never caused a problem, which is considered overtreatment.
Using MRI and ultrasound. Scientists at NCI have developed a procedure that combines magnetic resonance imaging with TRUS for more accurate prostate biopsies. MRI can locate potential areas of cancer within the gland but is not practical for real-time imaging to guide a prostate biopsy. The new procedure, known as MRI-targeted biopsy, uses computers to fuse an MRI image with an ultrasound image. This lets doctors use ultrasound guidance to biopsy areas of possible cancer seen on MRI.
Prostate Cancer Research: Staging Of Prostate Cancer
Determining stage of prostate cancer plays a key role in deciding the treatment options. However, imaging techniques, such as CT and MRI, used in prostate cancer cannot detect all cancer areas, particularly the small cancerous areas in lymph nodes.
A novel method, called multiparametric MRI, can help determine the extent of cancer and how aggressive can the cancer be, as these factors may affect the treatment options. This examination involves a standard MRI followed by at least one different MRI technique . Then, results of different scans are taken into consideration.
Another novel method, called enhanced MRI, may help detect the lymph nodes that contain cancer cells. First, a standard MRI is scanned. Next, small magnetic particles are injected and other scan is run on the next day. Differences between these two scans indicate the potential cancer cells in lymph nodes. The initial results of this technique are promising however, it should be further studied before it is commonly used.
A new type of positron emission tomography that uses radioactive carbon acetate instead of labeled glucose may be helpful for determining the prostate cancer in other parts of the body and whether the treatment is working or not. This technique is also studied today.
Read Also: Adenocarcinoma Prostate Gleason Score 7
Research Into Treatment For Prostate Cancer
Before new treatments can be introduced, they need to be tested thoroughly. This is so we can be sure that they work and that they are safe.
Go to Cancer Research UKs clinical trials database if you are looking for a trial for prostate cancer in the UK. You need to talk to your specialist if there are any trials that you might be able to take part in.
Some of the trials on this page have now stopped recruiting people. It takes time before the results are available. This is because the trial team follow the patients for a period of time and collect and analyse the results. We have included this ongoing research to give examples of the type of research being carried out on prostate cancer.
Study Shows Which Patients With Advanced Prostate Cancer Will Benefit From Chemotherapy
24 June 2022
Researchers have recommended changes to how cancer patients are treated, after a new UCL-led study discovered that chemotherapy is significantly more effective for some men with advanced prostate cancer than others.
On average, docetaxel chemotherapy improved 5-year survival by 10% compared to standard hormone therapy, which works by reducing the levels of male hormones in the body to stop them from reaching the cancer cells.
And both treatments may be offered to all men diagnosed with advanced prostate cancer.
However, the research, which was presented at the American Society of Clinical Oncology and funded by Prostate Cancer UK, found that men who had many metastases when they were diagnosed benefitted most from docetaxel chemotherapy, with 39% surviving five years, compared to 26% who had hormone therapy alone.
Among those with many metastases who also had larger prostate tumours, 55% survived for five years after having the treatment, compared to just 20% of men who just had hormone therapy.
In this study, those with many metastases or high volume metastatic disease, had either four or more secondary tumours in the bones and/or any metastasis in an organ such as the liver or lungs.
Meanwhile, men with fewer than 4 bone metastases and who had been diagnosed with prostate cancer at an earlier stage, did not benefit from docetaxel chemotherapy at all.
Around 47,500 men are diagnosed with the cancer each year, with 6,000 cases classed as advanced.
Don’t Miss: How To Promote Good Prostate Health
Cris Impact In Prostate Cancer
Since 1953, the Cancer Research Institute has provided almost 100 grants to research and clinical trial initiatives in the field of prostate cancer, totaling almost $25 million in financial support.
In fact, $9 million of this funding was given in conjunction with the CRI Prostate Cancer Initiativea program started in 1996 to support clinical research promising the most readily available and immediate benefits to prostate cancer patients. The CRI Prostate Cancer Initiative also aimed to improve prostate cancer patient outreach and increase public awareness of the disease.
Our organization has also participated in cooperative efforts to develop informative resources and materials for prostate cancer patients in close partnership with national nonprofit ZEROs patient support program.
Some work and recent findings by CRI investigators that are advancing the understanding and treatment of prostate cancer include:
See what prostate cancer-specific research were currently funding. With your help, we can fund more research and revolutionize the way cancer is treated, forevercuring more people and saving more lives.
- Immunomodulators
- Oncolytic Virus Therapy
- PSCA: a surface protein that is found on several cell types and is often overexpressed by cancer cells
- PSMA: a surface protein found on prostate cells that is often overexpressed by prostate cancer cells
Allowing Cells To ‘let Their Freak Flags Fly’
According to Lee, immunotherapies like checkpoint inhibitors have achieved response rates of around 20% to 30% in many different solid tumor types, but they have not worked as well in prostate cancers.
One reason, he believes, is because prostate cancers donât have a lot of DNA mutations, or as he puts it, they have a âlow mutational burden.â
âThe importance of that is that the immune system has to figure out what is âself’ and what is ânon-self’ or foreign,â he said. âCancer develops in our body, so itâs part of us. If there are mutations, the proteins that are presented or flagged on the surface appear abnormal to the immune system.â
But with a low mutational burden, there arenât many abnormal flags flying.
âThat makes it difficult for the immune system to even act,â Lee said. âAnd on top of that, prostate cancers have an environment that is very inhospitable to the activity of immune cells.â
Lee and his team have come up with a potential workaround, though. Since the immune system usually recognizes cancer cells by their abnormal flags â or antigens â and prostate cancer has few mutations , the researchers devised a plan to force cancerâs hand.
âThe hope is that, by inhibiting ERAP1, youâre raising the flag of these antigens that the immune system can recognize to slow down or decrease the growth of these tumors,â he said.
Don’t Miss: What Age To Check Prostate Cancer
Targeted Radiation Therapy And Psma
Scientists are also developing targeted therapies based on PSMA, the same protein that is being tested for imaging prostate cancer. For treatment, the molecule that targets PSMA is chemically linked to a radioactive compound. This new compound can potentially find, bind to, and kill prostate cancer cells throughout the body.
In a recent clinical trial, men with a type of advanced prostate cancer who received a PSMA-targeting drug lived longer than those who received standard therapies. Ongoing and planned clinical trials are testing PSMA-targeting drugs in patients with earlier stages of prostate cancer, and in combination with other treatments, including targeted therapies like PARP inhibitors and immunotherapy.
New Epigenetic Markers For Prostate Cancer Discovered
by Garvan Institute of Medical Research
New epigenetic biomarkers to predict more aggressive forms of prostate cancer have been discovered by scientists at the Garvan Institute of Medical Research.
The biomarkers can be used in combination with traditional clinical tools to predict if a man will go on to develop a more metastatic and lethal form of the disease and could help clinicians to develop a better treatment plan.
“There’s a need for men with prostate cancer to have more personalized treatments guided by the nature of their tumors, and they can’t get that without new biomarkers that can better predict the risk of developing the lethal form the disease,” says Professor Susan Clark, Head of the Epigenetic Research lab at Garvan and lead researcher of the study.
Prostate cancer is, globally, the second most common cancer diagnosed in men. After diagnosis, about 50% of men will develop metastatic cancer during their lifetime. Typically, metastasis takes 15 or more years to develop, but a small percentage of men develop a fatal, metastatic form much earlier after diagnosis.
The new study is published in the journal Clinical and Translational Medicine.
Historic samples important in finding prostate cancer biomarkers
This is one of the most long-term and comprehensive molecular studies of prostate cancer progression. The slow progression of the disease makes studying its biology difficult.
The new findings provide hope for a pathway to more personalized cancer treatment.
Don’t Miss: Can Prostate Cancer Spread To Testicles
Could It Work In Other Cancers
Even better, thereâs a possibility that this innovative approach may lead to immunotherapies for other solid tumors.
âOver 30,000 men pass away every year in the U.S. from metastatic prostate cancer,â Lee said. âWeâre hoping that these two strategies can be leveraged to develop new treatment combinations for that disease and expand the powerful reach of immunotherapies for advanced prostate cancer. And weâre also hoping that if successful, this concept can be broadly applied in the future to other cancer types.â
Chakoian said the potential to expand into additional cancers is whatâs most exciting for him.
âIf he can break through that conundrum and develop new therapies for prostate cancer, some of the principles that heâs come up with may be applicable to other solid tumor cancers,â Chakoian said. âThatâs the part of this project that Iâm excited about, finding new ways for the T cells to find the cancer cells and kill them. Thatâs brilliant.â
Lee, who has been at Fred Hutch for nearly five years, admits his project is âambitious,â and he said much credit goes to the Kleberg Foundation for their financial support.
Immunotherapy For Prostate Cancer Includes Two Fda
The prostate is a small, walnut-shaped gland that is part of the male reproductive system. The prostate is located just below the bladder, where it surrounds the top portion of the urethra . The main function of the prostate gland is to secrete fluid that nourishes and protects sperm.
As the second most common male cancer in the world, prostate cancer affects roughly 1.3 million people and kills more than 360,000 people each year, which represents about 4% of all cancer deaths worldwide. In the United States alone, there will be roughly 248,000 new cases and more than 34,000 deaths in 2021. Prostate cancer, the eighth leading cause of cancer-related deaths, will impact an estimated 1 in every 7 men in their lifetimes.
In its early stages, prostate cancer is highly treatable, with five-year survival rates close to 100%. Once prostate cancer has metastasized, however, the 5-year survival rate falls to less than 30%, highlighting a significant need for more effective treatment of advanced stage disease.
Also Check: What Happens If Prostate Is Removed
Prostate Cancer Research: How Does Detecting Gene Changes Work
Gene changes are particularly useful in men who have already been diagnosed with prostate cancer. When doctors analyze their gene changes they can get a clearer picture of their condition. It could reveal more accuracy on important information respective to their condition. For example, how probable it is their cancer may grow or spread.
With this new information at hand, they can better adapt their treatment options to each patient, on a case-by-case basis.
Ultrasound Scan Can Detect Prostate Cancer: Research
Washington , October 29 : According to new research, an ultrasound scan can be used to detect prostate cancer.
Researchers at Imperial College London, University College London and Imperial College Healthcare NHS Trust have found that a new type of ultrasound scan can diagnose most prostate cancer cases with good accuracy in a clinical trial involving 370 men.
The ultrasound scans missed only 4.3 per cent more clinically important prostate cancer cases — cancer that should be treated rather than monitored — compared to magnetic resonance imaging scans currently used to detect prostate cancer.
MRI scans are expensive and time-consuming. The team believes that an ultrasound scan should be used as a first test in a community healthcare setting and in low and middle-income countries which do not have easy access to high-quality MRI scans. They say it could be used in combination with current MRI scans to maximise cancer detection. The study is published in Lancet Oncology.
Professor Hashim Ahmed, lead author of the study and Chair of Urology at Imperial College London, said: “Prostate cancer is the most commonly diagnosed cancer in the UK. One in six men will be diagnosed with the disease in their lifetimes and that figure is expected to rise.
Although mpUSS is more widely available than mpMRI there has been no large-scale studies to validate its effectiveness as a test to detect prostate cancer cases.
Also Check: Why Does My Prostate Hurt
Attacking Prostate Cancer: The Latest Weapons
Tanya Dorff, M.D., an internationally renowned expert in the treatment of prostate cancer, has seen the future and she likes the view.
Our patients are living significantly longer, said Dorff, associate professor in the Department of Medical Oncology & Therapeutics Research. Thats due in part to intensified first line therapy, or better use of existing drugs, as well as a rapid acceleration of new drug development. As a result, she says We can promise men, even with advanced prostate cancer, years of good quality life.
Good news, considering that prostate cancer is the second most common cancer in men, with over 260,000 new cases every year. And advanced prostate cancer can be deadly, claiming 34,000 lives annually.
Dorff is determined to bring those numbers down. She believes the true path to success is clear.
Immunotherapy will get us there, she says.
Parp Inhibitors For Prostate Cancer
A PARP inhibitor is a substance that blocks an enzyme in cells called PARP. PARP helps repair DNA when it becomes damaged. Some prostate tumors have genetic defects that limit their ability to repair DNA damage. Such tumors may be sensitive to PARP inhibitors.
Two PARP inhibitors, olaparib and rucaparib , have been approved for some men whose prostate cancer has metastasized, and whose disease has stopped responding to standard hormone treatments.
Don’t Miss: Do You Lose Your Hair With Radiation For Prostate Cancer
Research Into The Quality Of Life Of Men With Prostate Cancer
More and more men are surviving prostate cancer. So researchers are interested in the quality of life of men who finish their treatment. They want to see which men are more likely to have side effects from their treatment.
They are also looking into the mental wellbeing and quality of life of men newly diagnosed with prostate cancer.
New Treatment Approved For Late
- By Charlie Schmidt, Editor, Harvard Medical School Annual Report on Prostate Diseases
In late March, the FDA approved a new therapy for advanced prostate cancer that is metastasizing, or spreading, in the body. Called Pluvicto , and delivered by intravenous infusion, the treatment can seek out and destroy tumors that are still too small to see with conventional types of medical imaging.
Pluvicto is approved specifically for men who have already been treated with other anticancer therapies, including chemotherapy and hormonal therapies that block the tumor-promoting hormone testosterone. The drug contains two parts: one that binds to a protein on prostate cancer cell surfaces called PSMA, and a radioactive particle that kills the cancer cells. Most normal cells do not contain PSMA, or do only at very low levels. This allows Pluvicto to attack tumors while sparing healthy tissues.
To confirm whether a man is eligible for the drug, doctors first inject a radioactive tracer that travels the bloodstream looking for and then sticking to PSMA proteins. Cancer cells flagged by the tracer will show up on a specialized scanning technology called positron-emission tomography. About 80% of prostate cancer patients have PSMA-positive tumors for those who do not, the treatment is ineffective.
Recommended Reading: How Long Does Zoladex Work For Prostate Cancer
An Increase In Available Drug Options
While LuPSMA isnt yet on the market, the sheer number of new medications already available for advanced prostate cancer has been a major research boon in recent years. The proliferation of medications within the advanced prostate cancer space has significantly increased the options available to the treating provider, Dr. Haywood says. Since the time I started urology training, several medications targeting the androgen hormone axis have been approved, resulting in significant expansion of the options available to men with advanced prostate cancer. More on those next.
