What Are Some Common Uses Of Prostate Mri
Your doctor uses MRI to evaluate prostate cancer and see if it is limited to the prostate. MRI provides information on how water molecules and blood flow through the prostate. This helps determine whether cancer is present and, if so, whether it is aggressive and if it has spread.
Sometimes, MRI of the prostate is needed to evaluate other prostate issues, including:
- infection or abscess.
- an enlarged prostate
- congenital abnormalities
- complications after pelvic surgery
MRI can tell the difference between diseased tissue and normal tissue better than x-ray, CT and ultrasound.
Technique Of Mri Targeted Biopsy
In general, TB can be performed as direct in-bore MRI-guided biopsy, as VE biopsy or as fusion-biopsy with software-registration. Fusion-guided biopsies consist of co-registrating pre-acquired MRI data with real-time US with the use of software and computing of the probe location and can be performed using elastic fusion systems or rigid fusion systems .
Figure 3
Visual estimation
In-bore MRI-guided biopsy
MRI/TRUS-fusion-guided biopsy
Figure 4
Comparative studies of different targeted biopsy approaches
Imaging Tests Used To Diagnose Prostate Cancer
Considering that prostate cancer is the second most common type of cancer found in men, it is incredibly important for men to be aware of the disease. A prostate cancer diagnosis is not rare, and the illness can often be successfully treated when detected before it has the opportunity to spread. To catch prostate cancer early, men must take advantage of the screening and imaging tests available for diagnosing the disease.
To better inform patients about prostate cancer testing, well discuss what prostate cancer is, the methods most medical professionals use to test for prostate cancer and where you can go for reliable prostate cancer imaging testing.
Don’t Miss: What Blood Test Is For Prostate
Choosing Where To Have Your Mri Is Key To Getting An Accurate Diagnosis
Until recently, a patient with abnormally high prostate-specific antigen level would be sent for a biopsy to determine if he had prostate cancer. This biopsy is guided by ultrasound, which urologists use to take twelve samples of the prostatein an attempt to find cancer regardless of where it is in the gland.
As a diagnostic tool for prostate cancer, however, ultrasound is limited. The ultrasound images show the prostate gland well enough to guide the twelve samples, but ultrasound often does not show the cancer inside the prostate. As a result, a biopsy may miss aggressive prostate cancer and may instead discover indolent prostate cancer that need not be treated.
Ultrasound may not find the bad cancer, and sometimes it identifies cancers that would be better left alone, says Dr. Hiram Shaish, assistant professor of radiology at Columbia University Irving Medical Center.
Now, men with high PSA levels are more and more frequently being offered a specialized test called multiparametric magnetic resonance imaging . MpMRI provides high-quality imaging that can visualize cancer in the prostate, distinguishing tumors that need to be treated from insignificant tumors that do not.
Given the insurance restrictions around this costly exam, patients basically have one chance to get it right.
Repeating The Psa Test
A mans blood PSA level can vary over time , so some doctors recommend repeating the test after a month or so if the initial PSA result is abnormal. This is most likely to be a reasonable option if the PSA level is on the lower end of the borderline range . For higher PSA levels, doctors are more likely to recommend getting other tests, or going straight to a prostate biopsy.
Read Also: What Is Prostate Antigen Test
Prostate Cancer Symptoms Are Frequently Ignored Resulting In The Disease Progressing To An Advanced Stage Keep An Eye Out For Any Early Signs Of Prostate Cancer And Don’t Dismiss It As A Minor Illness
Representational image. News 18 Hindi
After lung cancer, prostate cancer is the second leading cause of death, which is the most common non-skin cancer diagnosed in men. In 2020, there will be 34,500 cases of prostate cancer, with a projected increase to 48,700 by 2030. The mortality rate in 2022 will be 16,600. The prostate is a gland in the male reproductive system located just below the bladder and in front of the rectum. It is about the size of a walnut and covers the urethra. Fluid, which is a component of sperm, is produced by the prostate gland.
Pharma companies are on their toes in terms of R& D and manufacturing of more effective drugs for prostate cancer. According to a study published in The Lancet Oncology report, more boys than girls are diagnosed with cancer in India, and the likely cause is societal gender bias. Between January 1, 2005, and December 31, 2019, the researchers collected individual data on children aged 0 to 19 years with cancer from hospital-based records at three cancer centers in India.
Almost all prostate cancers, according to the National Cancer Institute , are adenocarcinomas . Early symptoms of Prostate cancer are frequently absent. Advanced prostate cancer patients may urinate more frequently or have weaker urine flow, but these symptoms can also be caused by other prostate conditions.
Most common symptoms of prostate cancer:
Advanced or metastatic prostate cancer symptoms:
What should young men know about prostate cancer?
What Is The Strength Of The Mri Scanner
The field strength of the MRI magnet is measured in teslas, and systems can range between .5T and 3T. A 3T scanner will provide the radiologist with the highest quality images in the case of the prostate gland which is a very small organ. Images from a scanner with a weaker field strength could potentially lead to an inaccurate diagnosis. We give a lot of second opinions of scans that have been performed elsewhere, says Dr. Shaish. Often the quality isnt high enough, and we cant provide the diagnosis that the patient needs.
Don’t Miss: How Common Is Prostate Cancer
A Different Way To Detect Metastases
Most men diagnosed with prostate cancer have localized disease, meaning the cancer appears to be confined to the prostate gland. However, certain factors have been linked to a higher risk of the cancer eventually spreading .
Currently, in the United States and many other countries, most men diagnosed with high-risk localized prostate cancer undergo additional testing to see if there is evidence of metastatic cancer. For many years, that has been done with a conventional CT scan and a bone scan , the latter because prostate cancer often spreads to the bones.
But both imaging technologies have limitations. Neither is particularly good at finding individual prostate cancer cells, and thus can miss very small tumors. And bone scans can detect bone damage or abnormalities that were caused by something other than cancer , resulting in false-positive findings that can lead to unnecessary additional testing.
So, researchers have been developing and testing other imaging agents that can find prostate cancer cells specifically in the body, Dr. Shankar explained.
As their name implies, PET-CT scans combine a CT scan with a PET scan, another type of nuclear imaging test that requires patients to receive intravenous injections of a radioactive tracer that can be detected on the scan.
Detection Of Recurrent Disease
In patients presenting with recurrent prostate cancer, clinical decision making is essential in both defining the nature of the relapse and selecting the appropriate intervention. At the time of relapse after RP or radiation, patients commonly present with a rising PSA. Clearly, this is representative of local recurrence, metastatic relapse, or both, or may represent residual benign elements in the prostate or prostate bed. Numerous definitions exist for relapse after primary therapy, but within the context of this discussion, the critical element remains defining the nature of the relapse.
In the case of RP, men with rising PSA believed due to isolated local recurrence can undergo salvage radiotherapy as an option for curative therapy. Overall rates of response to salvage radiotherapy suggest that the majority of men with relapse have metastatic disease at presentation. Typically, local recurrence is not identified by local imaging until adequate disease volume for detection exists. Biochemical relapse after RP does not usually occur when serum PSA levels are below 1.0 ng/ml.
Perhaps the best means of assessing the accuracy of ProstaScint in evaluating local recurrence is in comparing its outcome to that of salvage radiation. Wilkinson and Chodak63 evaluated 42 patients with biochemical relapse and proceeded with salvage radiotherapy in 15 who had evidence of isolated local recurrence. The initial and durable responses to radiation were 66.7% and 46.7%, respectively.
You May Like: Can An Mri Detect Prostate Cancer
Search For Metastases In Localized And Locally Advanced Prostate Cancers
The search for metastases was performed based on the presence of clinical symptoms, from the diagnosis of localized PCa in asymptomatic patients, or in the follow-up of treated PCa. Lymph node or bone metastases are rarely detected in this context .
In patients followed-up for localized PCa, metastases should be sought according to the risk group defined by the National Comprehensive Cancer Network or by the European Association of Urology guidelines , to estimate the 5-year biological relapse risk. These guidelines are heterogeneous across the world. Hence, it is of interest to provide answers for routine clinical practice to the following question: How can metastases in LN, bone, or locoregional disease in seminal vesicles be better diagnosed?
Is There Disease in the LN ?
Computed tomography scans are mainly performed to diagnose LN involvement. Nevertheless, there is difficulty with CT scan validation, either at initial diagnosis or for recurrence.
Table 1. Sensitivity and specificity of currently available functional and targeted imaging methods for LN staging of PCa.
Is There Disease in Seminal Vesicles ?
Table 2. Sensitivity and specificity of currently available functional and targeted imaging methods for detection of SVI in PCa.
Is There Disease in Bones ?
Table 3. Sensitivity and specificity of currently available functional and targeted imaging methods for bone staging of PCa.
About Dr Dan Sperling
Dan Sperling, MD, DABR, is a board certified radiologist who is globally recognized as a leader in multiparametric MRI for the detection and diagnosis of a range of disease conditions. As Medical Director of the Sperling Prostate Center, Sperling Medical Group and Sperling Neurosurgery Associates, he and his team are on the leading edge of significant change in medical practice. He is the co-author of the new patient book Redefining Prostate Cancer, and is a contributing author on over 25 published studies. For more information, contact the Sperling Prostate Center.
Search the spc blog
Don’t Miss: Prostate Cancer Survival Rates Radiation Vs Surgery
Introduction To Clinical Context And Proposed Utility Of Modality
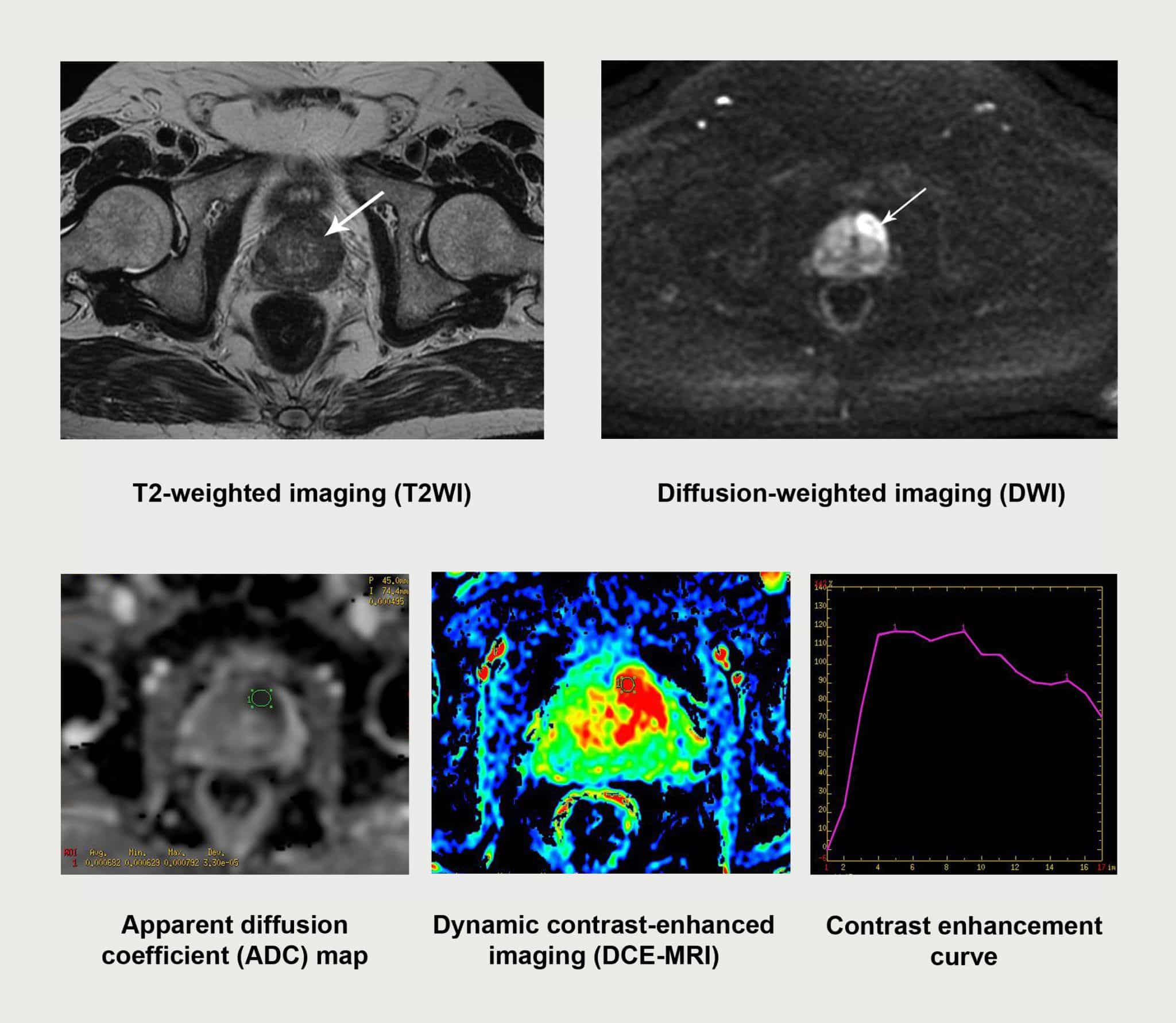
MRI became the method of choice for detection and staging of prostate cancer . Adapted from breast imaging a Prostate Imaging Reporting and Data System was published by the European Society of Urogenital Radiology : PI-RADS version 1 . This first guideline paper was based on a summary score for each lesion assessed in different sequences of mpMRI, consisting of T2w, DWI and DCE-MRI and spectroscopy facultatively. These guidelines have been updated recently by a steering committee including the American College of Radiology , ESUR and the AdMeTech Foundation to the PI-RADS v2 . In this version spectroscopy was omitted and DCE-MRI was attributed a minor role. In contrast to version 1 each lesion is attributed a single score based on findings of mpMRI. The objectives of these guidelines were to promote global standardisation of prostate imaging, to improve detection, localisation, characterisation, risk stratification of prostate cancer in treatment naïve prostate as well as to improve communication with referring urologists. The latest PI-RADS version assesses the likelihood of clinically significant prostate cancer on a 5-point scale for each lesion as follows:
-
PI-RADS 1 Very low
-
PI-RADS 2 Low
-
PI-RADS 3 Intermediate
-
PI-RADS 4 High
-
PI-RADS 5 Very high
For corresponding examples of findings see Fig. .
Fig. 1
What Do My Scan Results Mean
Your TNM stage is used to work out if your cancer is localised, locally advanced or advanced. This can help your doctor see how far it has spread and which treatment might be suitable for you.
Cancer thats contained inside the prostate. Sometimes called early prostate cancer. Possible TNM stages are:
- T stage: T1 or T2
- N stage: N0 or NX
- M stage: M0 or MX.
Cancer thats started to break out of the prostate, or has spread to the area just outside it. Possible TNM stages are:
- T stage: T1 or T2
- T stage: T3 or T4
- N stage: N0 or N1
Read Also: Alternative Cures For Prostate Cancer
Read Also: What Are The Risks Of Prostate Cancer
What Final Thoughts Do You Have For Prostate Cancer Patients Watching
Dr. Tagawa: Yeah, what’s nice in the current era, I would say, of treating men with prostate cancer is we have many more options than we did just a short number of years ago, and those have to do with a combination of both diagnostics such as scans or genetic testing, biopsy et cetera, as well as treatment. So it’s very nice to see that and it’s nice to see them coming together.
To address several of the questions I saw in the Q& A that had to do with different types and availability of these scans, what I would suggest both for treatment as well as imaging is to be your own advocate and advocate for your loved ones and just ask the question. Some of the times, I would say it’s not worth it to even travel across the street to get a fancy scan because it’s not going to make a difference, and other times it would make a major difference to travel for that.
So, ask, and specifically for PSMA PET, there are a number of different agents out there that are confusing even for me, they’re very, very similar. So if one’s available one state over and one’s available 10 states over or in a different country, it probably doesn’t matter so much. So don’t look only for Gallium or only for Fluorine-18 or these different acronyms that we look for. PSMA imaging, I think at least for the beginning, is interchangeable. So any of those will be okay.
Recommended Programs:
What Happens During The Exam
You will be asked to wear a hospital gown during the MRI scan.
As the MRI scan begins, you will hear the equipment making a muffled thumping sound, which will last for several minutes. Other than the sound, you should notice no unusual sensations during the scanning.
Certain MRI exams require an injection of a dye . This helps identify certain anatomic structures on the scan images.
Before the exam, feel free to ask questions and tell the technician or doctor if you have any concerns.
People who get anxious when in tight spaces may benefit from talking to their doctor before the procedure. Some options include taking a prescription medication before the procedure to relieve anxiety or having the exam done in one of the newer and less confining MRI units, called an open MRI, when available.
Read Also: How Does Prostate Cancer Spread To Spine
Imaging Of Nodal Metastases At Initial Staging
The probability for LN metastases at initial diagnosis of localized PCa is associated with risk classification very low risk and low-risk patients have an exceedingly low probability for LN metastasis . Accurate assessment of LN status helps in therapeutic decision making, prediction of recurrence risk, and assessment of prognosis.
The presence of LN metastasis is an independent risk factor for BCR , and there is great interest in preoperative imaging-based identification of LN metastases to optimize surgical and adjuvant or neoadjuvant treatment planning. Currently, the clinical practice and urologic guidelines primarily rely on validated clinical nomograms to help guide decision making for pelvic lymph node dissection, with a calculated estimated risk of more than 5% being an indication to perform extended pelvic lymph node dissection . Even though pelvic lymph node dissection is the traditional gold standard for LN staging, it is an invasive, time-consuming approach largely dependent on surgical skill and templates.
As of yet, no single imaging modality has shown optimal diagnostic performance in the assessment of metastatic LNs. Studies with the PET tracers 18F-choline, 11C-choline, and 18F-fluciclovine reported similar high specificities but low sensitivities ranging from 40% to 50% .
What Do Psa And Next Generation Imaging Tests Mean For Prostate Cancer Patients
In this segment of our Answers Now series, a panel of prostate cancer experts and advocates discuss the latest developments in testing and imaging for prostate cancer. What tests should patients receive, and when? What can PSMA PET and Next Generation Imaging mean for individuals at different points in their prostate cancer journey? Find out in the video above.
Experts include Scott Tagawa, MD, Professor of Medicine and Urology at New York-Presbyterian-Weill Cornell Medical Center and David VanderWeele, MD, PhD, Assistant Professor of Medicine in the Division of Hematology and Oncology at Robert H. Lurie Comprehensive Cancer Center of Northwestern University. The discussion is guided by Patient Power co-founder Andrew Schorr, as well as AnCan Prostate Cancer Moderators Len Sierra and Peter Kafka.
This program is sponsored by Bayer. This organization has no editorial control. It is produced by Patient Power. Patient Power is solely responsible for program content.
Andrew Schorr: Greetings. I’m Andrew Schorr, co-founder of Patient Power. Thank you so much for joining us for the second in our series of Patient Power programs produced in association with AnCan, a wonderful advocacy group that you may know, or if you don’t, you’re going to hear more about it and I hope you’ll take advantage of their support groups and services.
Dr. Tagawa: Thanks for your invitation, I’m happy to be here.
Dr. VanderWeele: Great, thanks for having me. Happy to be here.
Recommended Reading: Gleason Scores In Prostate Cancer
Additional Pet Scanning Faq
Is PET scanning safe?
While PET scanning does involve the use of radioactive tracers, these are diagnostic levels of radiation that are completely safe and have no known side effects.
How long does it take to get the results after a PET Scan?
Images are captured and created during the PET scan procedure, and afterward, a radiologist will utilize their training and experience to interpret the scan and produce a written report of findings and conclusions. This report is then transmitted to your referring physician who would then review those results with you and discuss any further treatment if needed.
What is it like for a patient to have a PET Scan?
Please watch this video we created that clearly walks one through the experience of having a PET scan and answers all common questions about PET scanning.
