Acinar Adenocarcinoma Of The Lung
Adenocarcinoma is the most common type of lung cancer in the U.S., Japan, and most of Western Europe, although it is the second most common form in Eastern parts of Europe . Adenocarcinomas are exceptionally heterogeneous neoplasms, occurring in four major tissue architectures , and several rarer variants. Most commonly, however, these lesions show a mixture of two or more subtypes or variants, and are subclassified as “adenocarcinoma with mixed subtypes”.
In China, which has the largest number of smokers and lung cancer cases in the world, the acinar tissue architectural pattern is by far the most common histological subtype of adenocarcinoma, comprising about 40% of all adenocarcinomas, and its incidence has increased significantly in recent decades. In Europe, acinar adenocarcinoma may comprise the dominant architectural pattern in as many as 5060% of all adenocarcinomas.
Acinar adenocarcinoma of the lung is a highly lethal disease. Overall five-year survival rates approximate 16% to 22%. Generally, survival is better in all stages for patients with the acinar pattern than it is in patients with the solid pattern, but considerably worse than those with the bronchioloalveolar pattern. Survival is significantly better in patients whose tumors are well differentiated than when poorly differentiated .
Some studies suggest that the oncogenes H-ras and fes are important drivers of oncogenesis in many acinar-type lung cancers.
Recurrent Prostate Cancer Symptoms
Prostate cancer that returns after treatment is considered recurrent. When it returns to the area around the prostate, the disease is classified as a local recurrence. If the cancer is found in another part of the body, the recurrent cancer is considered metastatic. If the cancer metastasizes outside the prostate, it most likely develops in bones first. Metastatic prostate cancer most often spreads to the liver, bones and lungs.
After initial treatment for prostate cancer, PSA levels are expected to drop dramatically. The first sign of recurrent prostate cancer may be a rise in the PSA level. Other symptoms of recurrent cancer may depend on whether and where the cancer has spread. Symptoms include:
- Blood in the urine
- Difficulty breathing
Patients should discuss any symptoms with their doctor and ask about scheduling regular PSA tests after treatment.
Treatment Of Adenocarcinoma Of The Prostate
To date, the treatment of adenocarcinoma of the prostate gland is carried out by various methods, the choice of which depends on the type of tumor and the stage of the pathological process, as well as the age of patients and their condition.
Oncologists-urologists use surgical methods, radiotherapy, tumor destruction by ultrasound or freezing , as well as drug treatment aimed at androgenic blockade of prostate cells. Chemotherapy is used as a last resort to fight adenocarcinoma and its metastases with ineffectiveness of other methods.
Surgical treatment of adenocarcinoma is an open or laparoscopic prostatectomy , which is carried out only with the nonproliferation of neoplasia outside the gland. The abdominal surgery to remove the prostate gland under general anesthesia, endoscopic removal – under epidural anesthesia.
An operation to remove the testicles or part of them is resorted when oncologists decide on the feasibility of a complete blockade of testosterone production. But hormonal preparations with the same therapeutic effect can be used for these purposes , therefore this operation is done in rare cases.
Since most patients survive after such treatment, and the tumor almost does not relapse, oncology specialists of the European Association of Urology recommended cryotherapy for all cancers of the prostate, although, as an alternative method.
Recommended Reading: How Long After Prostate Surgery Does Impotence Last
About The Prostate And Prostate Cancer
The prostate gland, which grows during puberty, is considered an organ and is made up of several dozen lobules or saclike glands, held together with connective prostate tissue and muscle between them. The glands are called exocrine glands, because they secrete liquid to outside the body.
An enlarged prostate, called benign prostatic hyperplasia , is common in men over the age of 40 and may obstruct the urinary tract. The abnormal prostate cell growth in BPH is not cancerous and doesnt increase your risk of getting prostate cancer. However, symptoms for BPH and prostate cancer can be similar.
A condition called prostatic intraepithelial neoplasia , where prostate gland cells look abnormal when examined under a microscope, may be connected to an increased risk of prostate cancer. Prostate cancer is often caught by a doctor performing a digital rectal exam , through a prostate-specific antigen blood test, through a prostate biopsy or with a CT scan.
Another condition, prostatitis, is the inflammation of the prostate. While not cancerous, it may cause higher PSA levels in the blood.
When prostate cancer is found, pathologists stage the disease using a Gleason score, which grades the extent and arrangement of the cell mutations. For instance, a Gleason score of 6, the lowest possible, indicates a low-grade tumor, while cancers with scores of 9 or 10 are considered high-grade or the most aggressive and most likely to spread.
What Does It Mean If In Addition To Cancer My Biopsy Report Also Mentions Acute Inflammation Or Chronic Inflammation
Inflammation of the prostate is called prostatitis. Most cases of prostatitis reported on biopsy are not caused by infection and do not need to be treated. In some cases, inflammation may increase your PSA level, but it is not linked to prostate cancer. The finding of prostatitis on a biopsy of someone with prostate cancer does not affect their prognosis or the way the cancer is treated.
Recommended Reading: Does Prostate Stimulation Increase Testosterone
What Does It Mean To Have A Gleason Score Of 6 7 8 Or 9
Because grades 1 and 2 are not often used for biopsies, the lowest Gleason score of a cancer found on a prostate biopsy is 6. These cancers may be called well differentiated or low-grade and are likely to be less aggressive that is, they tend to grow and spread slowly.
Cancers with Gleason scores of 8 to 10 may be called poorly differentiated or high-grade. These cancers are likely to grow and spread more quickly, although a cancer with a Gleason score of 9-10 is twice as likely to grow and spread quickly as a cancer with a Gleason score of 8.
Cancers with a Gleason score of 7 can either be Gleason score 3+4=7 or Gleason score 4+3=7:
- Gleason score 3+4=7 tumors still have a good prognosis , although not as good as a Gleason score 6 tumor.
- A Gleason score 4+3=7 tumor is more likely to grow and spread than a 3+4=7 tumor, yet not as likely as a Gleason score 8 tumor.
Prostate Cancer Surveillance And Clinical Trials
Men who are older or who have other life-threatening illnesses may be candidates for watchful waiting. With watchful waiting, you do not undergo frequent, invasive testing. One of the reasons for watchful waiting is a slow-growing prostate tumor can behave more like a chronic disease rather than a fatal condition. Watchful waiting is an acceptable option for any man with a low-grade prostate tumor. Your oncologist will only recommend treatment if the tumor causes bothersome symptoms, such as difficulty urinating.
Although treatment is similar for the different types of prostate cancer listed above, knowing what type and stage of prostate cancer you have is important for treatment success. It helps you understand the treatment plan your doctor designs for you, and may help identify if you are eligible for a clinical trial. Trials look at new and better ways to treat prostate cancer. Many trials are specific for a particular stage, such as early stage prostate cancer or advanced prostate cancer. The trial may also consider the type of prostate cancer, such as neuroendocrine prostate cancer.
Read Also: How Do You Find The Prostate Gland
Advanced Prostate Cancer Symptoms
Men with advanced prostate cancer may experience additional symptoms. Thats because the cancer has spread from the prostate to other parts of the body, such as the bones or lymph nodes.
Signs of metastatic prostate cancer may include:
- Swelling in legs or pelvic area
- Numbness or pain in the hips, legs or feet
- Bone pain that persists or leads to fractures
A wide range of treatment options are available for managing advanced cancer. These treatments kill cancer cells, but they may also help patients manage pain.
Prostate cancer treatment: The care you need is one call away
Your multidisciplinary team will work with you to develop a personalized plan to treat your prostate cancer in a way that fits your individual needs and goals.
Active Surveillance And Watchful Waiting
If prostate cancer is in an early stage, is growing slowly, and treating the cancer would cause more problems than the disease itself, a doctor may recommend active surveillance or watchful waiting.
Active surveillance. Prostate cancer treatments may seriously affect a person’s quality of life. These treatments can cause side effects, such as erectile dysfunction, which is when someone is unable to get and maintain an erection, and incontinence, which is when a person cannot control their urine flow or bowel function. In addition, many prostate cancers grow slowly and cause no symptoms or problems. For this reason, many people may consider delaying cancer treatment rather than starting treatment right away. This is called active surveillance. During active surveillance, the cancer is closely monitored for signs that it is worsening. If the cancer is found to be worsening, treatment will begin.
ASCO encourages the following testing schedule for active surveillance:
-
A PSA test every 3 to 6 months
-
A DRE at least once every year
-
Another prostate biopsy within 6 to 12 months, then a biopsy at least every 2 to 5 years
Treatment should begin if the results of the tests done during active surveillance show signs of the cancer becoming more aggressive or spreading, if the cancer causes pain, or if the cancer blocks the urinary tract.
Recommended Reading: Over The Counter Treatment For Enlarged Prostate
Understanding Prostate Cancers Progression
To determine the appropriate treatment, doctors need to know how far the cancer has progressed, or its stage. A pathologist, the doctor trained in analyzing cells taken during a prostate biopsy, will provide two starting pointsthe cancers grade and Gleason score.
- Cancer grade: When the pathologist looks at prostate cancer cells, the most common type of cells will get a grade of 3 to 5. The area of cancer cells in the prostate will also be graded. The higher the grade, the more abnormal the cells.
- Gleason score: The two grades will be added together to get a Gleason score. This score tells doctors how likely the cancer is to grow and spread.
After a biopsy confirms prostate cancer, the patient may undergo additional tests to see whether it has spread through the blood or lymph nodes to other parts of the body. These tests are usually imaging studies and may include a bone scan, positron emission tomography scan or computed tomography scan.
Prostate cancer treatment: The care you need is one call away
Your multidisciplinary team will work with you to develop a personalized plan to treat your prostate cancer in a way that fits your individual needs and goals.
Staging Parameters Margins And More
Surgical margins
- Positive is tumour touching ink.
- “Close” margins have an increased recurrence risk.
Notes:
- Surgical margin – where the surgeon cut.
- It is possible to have EPE without a positive margin.
- It is possible to have a positive margin without EPE.
Rates and implication
Positivity rate varies substantially :
- Norway: 26% — strong dependence on surgeon volume .
- France: 13-17% — PSA and prostate size predictors of positivity.
Note:
- Stage and grade seem to have less impact than surgeons volume on margin positivity rate.
The impact of positive margins:
- Significant modest negative affect on long-term outcome in node negative cancers .
- Weaker impact than stage and Gleason score.
- Bladder neck margin positivity may change the T-stage – see below.
Bladder neck margin
- AKAinvasion of the bladder neck.
- Bladder neck margin positivity typically is pT3a.
- Seen in approximately 1% of prostatectomies.
Extraprostatic extension
- A. CAncer of the Prostate.
Other IHC stains:
- AR +ve — in prostate confined cancer.
- Usually -ve in lymph node +ve disease.
Note:
- Bcl-2 marks basal cells in prostate cancer.
Prostate carcinoma versus urothelial carcinoma
The ISUP panel recommends:
Another panel – if GATA3 isn’t available:
- Prostate: PSA +ve, p63 -ve, HWMCK -ve.
- Urothelial: p63 +ve, HWMCK +ve, PSA -ve.
Notes:
Read Also: Pain In Prostate After Ejaculation
What Does It Mean If My Biopsy Report Mentions The Word Core
The most common type of prostate biopsy is a core needle biopsy. For this procedure, the doctor inserts a thin, hollow needle into the prostate gland. When the needle is pulled out it removes a small cylinder of prostate tissue called a core. This is often repeated several times to sample different areas of the prostate.
Your pathology report will list each core separately by a number assigned to it by the pathologist, with each core having its own diagnosis. If cancer or some other problem is found, it is often not in every core, so you need to look at the diagnoses for all of the cores to know what is going on with you.
What Does It Mean If My Biopsy Report Also Mentions Atrophy Adenosis Or Atypical Adenomatous Hyperplasia
All of these are terms for things the pathologist might see under the microscope that are benign , but that sometimes can look like cancer.
Atrophy is a term used to describe shrinkage of prostate tissue . When it affects the entire prostate gland it is called diffuse atrophy. This is most often caused by hormones or radiation therapy to the prostate. When atrophy only affects certain areas of the prostate, it is called focal atrophy. Focal atrophy can sometimes look like prostate cancer under the microscope.
Atypical adenomatous hyperplasia is another benign condition that can sometimes be seen on a prostate biopsy.
Finding any of these is not important if prostate cancer is also present.
Read Also: How To Properly Use A Prostate Massager
Can The Gleason Score On My Biopsy Really Tell What The Cancer Grade Is In The Entire Prostate
Because prostate biopsies are tissue samples from different areas of the prostate, the Gleason score on biopsy usually reflects your cancers true grade. However, in about 1 out of 5 cases the biopsy grade is lower than the true grade because the biopsy misses a higher grade area of the cancer. It can work the other way, too, with the true grade of the tumor being lower than what is seen on the biopsy.
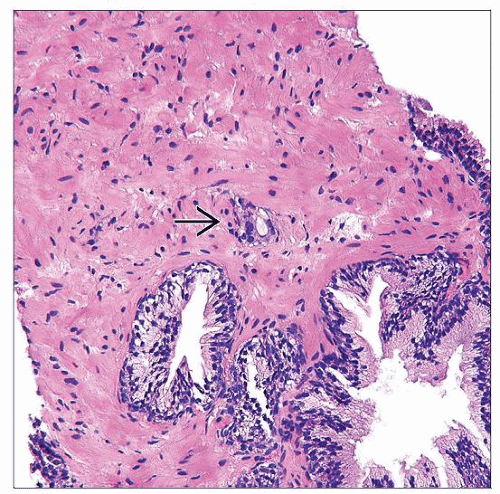
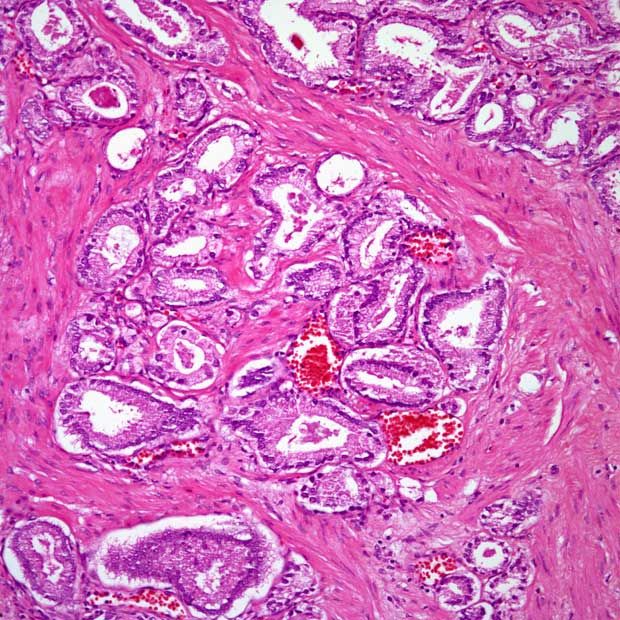
Classification Of Prostatic Diseases
Common diseases of the prostate include acinar adenocarcinoma, BPH, chronic prostatitis, hemorrhage, cysts, calcifications, atrophy and fibrosis. Uncommon diseases of the prostate include tumors other than acinar adenocarcinoma, granulomatous prostatitis containing tuberculosis, abscesses and so on, and idiopathic disorders such as amyloidosis and exophytic BPH.
Many conditions that yield abnormal signals within the prostate, including hemorrhage, cysts, calcifications, atrophy and fibrosis, are benign and highly recognizable on mpMRI . In addition to these benign signal abnormalities and based on the applicability of PI-RADS assessment, we divide other focal signal abnormalities involving the prostate into two categories according to the patients age, serum PSA level, symptoms and mpMRI findings: category 1, diseases for which the PI-RADS assessment is suitable for use, and category 2, diseases for which the PI-RADS assessment is not suitable for use. Category 1 includes prostate cancer , typical BPH in the transitional zone , and some types of prostatitis/granulomatous prostatitis, which overlap in terms of clinical and mpMRI findings, while category 2 includes tumors except for PCa, exophytic BPH nodules, and some types of granulomatous prostatitis , for which PCa may be excluded according to the clinical and MRI findings.
Also Check: What Is The Best Cure For Prostate Cancer
Prophylaxis Of Prostatic Adenocarcinoma
Accessible to all prophylaxis of adenocarcinoma of the prostate gland is largely related to nutrition. If you have extra pounds, eat lots of red meat, love fatty and sweet, regularly and in large quantities drink beer , then you know: the risk of this pathology increases several times!
Experts from the American Cancer Society, based on the study of various case histories and clinical cases of malignant neoplasms of the prostate, recommend a balanced diet with an emphasis on plant foods: vegetables, fruits, whole grains, nuts, seeds , beans and peas. Red meat, as a source of animal protein, is best replaced with fish, white poultry meat and eggs. To the body weight did not exceed the norm, the food should be well balanced in calories and comparable to the level of physical activity. At the same time, protein in the daily diet should account for no more than 30% of calories, 50% for carbohydrates, and only 20% for fats.
But the role in the development of sex hormones leptin, synthesized by cells of adipose tissue, is no longer in doubt, for more details, see What is leptin and how does it affect weight?
Mucinous Pca Showed Similar Prognosis To Typical Prostate Adenocarcinoma
Previous studies remain controversial regarding the clinical progression of mucinous PCa. Several studies have considered this tumor to be an aggressive cancer that tends to develop bone metastases, with an associated poor outcome several studies have considered that mucinous PCa is not more aggressive and may be even less aggressive than typical prostatic adenocarcinoma . Therefore, to determine whether mucinous PCa shows a more adverse prognosis than typical prostate adenocarcinoma, we adjusted for differences in common prognostic predictors between mucinous PCa and typical prostate acinar carcinoma, including age, race, PSA, Gleason score, and SEER summary stage. Interestingly, when total 360 patients with mucinous PCa were compared with a control group of patients with typical prostate acinar adenocarcinoma, mucinous PCa patients had similar survival progression in terms of CSS and OS compared with those with typical prostate acinar carcinoma. Therefore, we can assume that the mucinous are clonally related to typical PCa. Similarly, Johnson et al. revealed that TMPRSS2-ERG is expressed in almost 50% of cases of mucinous PCa and PCa with mucinous features, similar to rates of expression in conventional PCa therefore, this study strongly suggests that these rare subtypes of PCa are clonally related to conventional PCa .
Read Also: Does Prostate Cancer Affect Libido
