Prostatectomy And Sexual Issues
As a man, your prostate gland plays several important roles in your bodys sexual and urinary function.
The nerves that surround your prostate also play an important role in allowing blood to flow to the erectile tissue of your penis when youre sexually aroused.
Because prostate surgery involves removing the prostate gland, its normal to lose some parts of your normal sexual function after the surgery.
For example, radical prostatectomy involves cutting the connection between your urethra and your testicles. This means that sperm is no longer able to flow down your urethra and out the tip of your penis during sex.
Several different approaches are used to remove your prostate gland during surgery. Some of these approaches particularly those used to treat prostate cancer may result in damage to the nerves that surround your prostate gland, testicles and penis.
Because recovery from prostate surgery is usually a slow, gradual process, it may take several months to find out how much your sexual function has been affected by prostate removal.
Can You Live Without A Prostate
Although the prostate is essential for reproduction, it is not essential to live.
In cases where the cancer is contained to the prostate it can be surgically removed through a prostatectomy.
A radical prostatectomy involves removing the entire prostate gland, the surrounding tissue, and some of the seminal vesicles.
Alternatively, laser prostatectomies can be effective as the least invasive type of prostate removal.
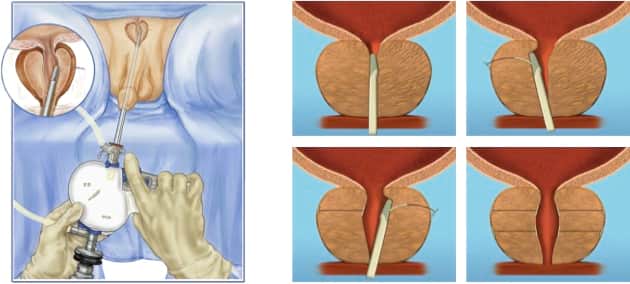
The most common prostatectomy is the transurethral resection of the prostate .
TURPs involve removing part of the prostate gland using a resectoscope which is passed through the urethra – this procedure is commonly used for people with an enlarged prostate.
In come cases prostate cancer can be treated with radiotherapy.
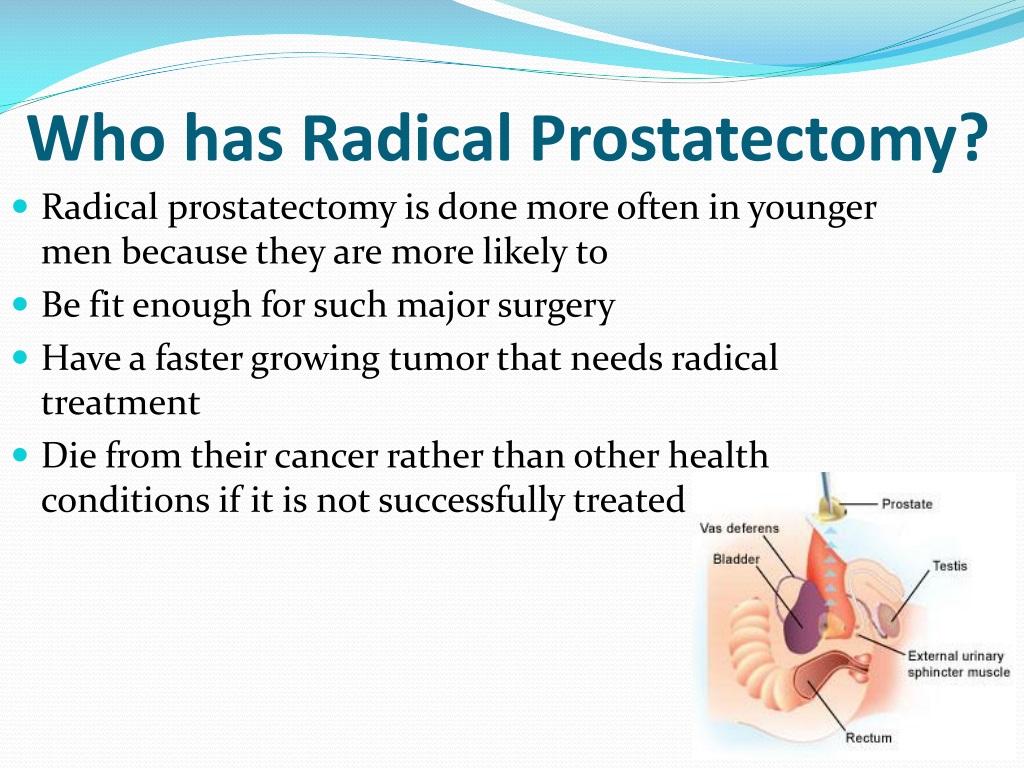
Who Should Get A Radical Prostatectomy
Men younger than 75 years old with limited prostate cancer and who are expected to live at least 10 more years tend to get the most benefit from radical prostatectomy.
Before doing a radical prostatectomy, doctors first try to confirm that the prostate cancer has not spread beyond the prostate. They can figure out the statistical risk of spread by looking at tables comparing the results of a biopsy and PSA levels.
Other tests to check for signs of spread, if needed, can include CT scans, bone scans, MRI scans, ultrasound, PET scans, and bone scans.
If it appears that the prostate cancer hasnât spread, your surgeon may first offer you other options besides surgery. These can include radiation therapy, hormone therapy, or simply watching the prostate cancer over time, since many prostate cancers grow slowly.
Depending on how high your risk of the cancer spreading is, your surgeon may also consider doing an operation called pelvic lymph node dissection.
Recommended Reading: What Is Adenocarcinoma Of The Prostate
Recurrent Prostate Cancer When Is It Happening
According to the Prostate Cancer Foundation, there are 20-30% chances of prostate cancer recurrence after prostatectomy after five years of initial prostate cancer treatment. This includes both surgical intervention and radiation treatment.
As a patient, the prospect of PSA recurrence can be very worrisome. What many patients do not know is that not all modified levels of PSA after prostate cancer treatment indicate recurrent prostate cancer. Some types of levels are much more troublesome than others and treatment approaches can vary tremendously case by case.
When PSA results are equal or greater than 0.2 ng/mL according to an initial test, then the second test was taken two weeks after returns with even a slight increase in PSA levels, then the case turns into a biochemical recurrence. This evolution of the disease can happen within 7 to 28 months after surgery or from 24 to 46 months. Life expectancy after biochemical recurrence of prostate cancer is 94% of 5.6 years after the diagnosis.
Not all changes in the PSA levels mean recurrent prostate cancer after robotic surgery or other forms of treatment. Elevated PSA after prostatectomy may also indicate other conditions, that is why the PSA check is essential after surgery.
Surgically Removing The Prostate Gland
A radical prostatectomy is the surgical removal of your prostate gland. This treatment is an option for curing prostate cancer that has not spread beyond the prostate or has not spread very far.
Like any operation, this surgery carries some risks, such as urinary incontinence and erectile dysfunction.
In extremely rare cases, problems arising after surgery can be fatal.
It’s possible that prostate cancer can come back again after treatment. Your doctor should be able to explain the risk of your cancer coming back after treatment, based on things like your PSA level and the stage of your cancer.
Studies have shown that radiotherapy after prostate removal surgery may increase the chances of a cure, although research is still being carried out into when it should be used after surgery.
After a radical prostatectomy, you’ll no longer ejaculate during sex. This means you will not be able to have a child through sexual intercourse.
You may want to ask your doctors about storing a sperm sample before the operation so it can be used later for in vitro fertilisation .
Read Also: What To Expect With Prostate Cancer
Surgery For Prostate Cancer
Surgery is a common choice to try to cure prostate cancer if it is not thought to have spread outside the prostate gland.
The main type of surgery for prostate cancer is a radical prostatectomy. In this operation, the surgeon removes the entire prostate gland plus some of the tissue around it, including the seminal vesicles.
During Watchful Waiting Or Active Surveillance
If you choose observation or active surveillance, your PSA level will be monitored closely to help decide if the cancer is growing and if treatment should be considered.
Your doctor will watch your PSA level and how quickly it is rising. Not all doctors agree on exactly what PSA level might require further action . Again, talk to your doctor so you understand what change in your PSA might be considered cause for concern.
Don’t Miss: How Is Prostate Cancer Causes
Minimally Invasive Surgical Options
In minimally invasive surgical procedures, we make several small incisions in your abdomen. We then insert a tiny, lighted telescopic camera called a laparoscope, along with specially designed surgical instruments that a surgeon uses to perform the operation.
When you have minimally invasive surgery, youre likely to have less discomfort after the procedure and more likely to recover faster than with a traditional open surgery, in which incisions are larger and more extensive. Many men who have their prostates removed in a minimally invasive operation are able to return home the following day.
We offer two types of minimally invasive surgery.
Many of our surgeons perform robot-assisted laparoscopic prostatectomy. This sophisticated tool offers much finer precision than any other surgical technique.
Using a device called the da Vinci® Surgical System, a surgeon performs the operation while seated at a console that has a viewing screen as well as hand, finger, and foot controls. The screen projects a three-dimensional image, magnified tenfold, of the prostate and the surrounding area. This allows the surgeon to view the surgical site in great detail. The robot then translates the surgeons hand, wrist, and finger movements into real-time movements of the instruments inside the patient.
As an alternative to surgery, we are investigating using focal therapy or radiation treatment instead of surgery to treat only the areas within the prostate gland where the cancer has returned.
Cancer Treatments And Erectile Dysfunction
Following surgery, many men experience erectile dysfunction , but for many, the disruption is temporary. Nerves damaged during surgery may result in erectile dysfunction. A nerve-sparing prostatectomy may reduce the chances of nerve damage. Another factor is the surgeons skill level for performing the nerve-sparing technique, which if done correctly, may improve patients likelihood of retaining erectile function, says Dr. Shelfo.
Prostate cancer may also be treated with various types of radiation therapybrachytherapy, external beam radiation or stereotactic body radiation therapy. Each type of therapy causes somewhat different side effects. About half of all prostate cancer patients who undergo any of these types of radiation therapy are likely to develop erectile dysfunction, according to a 2016 article published in Advances in Radiation Oncology.
When you compare surgery with radiation, both may affect erections, says Dr. Shelfo. Surgery is usually more immediate, and sexual dysfunction has the potential with time to improve. With radiation, erections are usually less affected in the beginning, but over timemonths or, sometimes, yearssexual dysfunction may develop. Both treatments may affect sexual function, resulting in no ejaculate or the ability to attain erections.
Also Check: What Is A Mans Prostate
Physical And Psychological Effects Of Prostate Biopsy And Cancer Diagnosis
The incorporation of prostate-specific antigen measurement and the transrectal ultrasound biopsy probe into standard urologic practice had a dramatic impact on the incidence of prostate cancer in the United States and resulted in a trend toward earlier-stage disease at presentation. No longer were men presenting with late-stage disease or undergoing painful perineal biopsies. The biopsy no longer required an anesthetic or a hospitalization. Within a 7-year period , the annual number of cases diagnosed doubled. Most cases are now detected by PSA elevation, rather than by digital rectal examination.
Though generally well-tolerated when done under a local anesthetic, the TRUS biopsy is not without side effects or complications. In a prospective study of 211 men undergoing prostate biopsies, intraoperative pain was considered severe in 20% of the biopsy events. Preoperative anxiety was reported in 64% of biopsy events and was predictive of intraoperative pain. Anxiety continued post-biopsy and peaked before result disclosure. ED attributed to anxiety in anticipation of biopsy was reported in 7% of cases. The ED incidence doubled to 15% at days 7 and 30 after the biopsy, well after the anxiety associated with the biopsy resolved.4
The Purpose Of Prostate Surgery
Prostate cancer surgery, or radical prostatectomy, is a procedure conventional medicine praises for curing prostate cancer.
It has been performed for many years and was regarded as the gold standard of prostate cancer treatment. However, few studies compare its efficacy to other techniques.
Most men diagnosed with prostate cancer today are typically diagnosed with Gleason 6 cancer levels. But, according to many experts, this diagnosis may not be cancer! According to Mark Scholz, MD, a board-certified oncologist and expert on prostate cancer:
Misuse of the term cancer has tragic implications. Real cancer requires action and aggressive medical intervention with the goal of saving a life. But consider the potential havoc created by telling someone they have cancer when it is untrue. This dreadful calamity is occurring to 100,000 men every year in the United States with men who undergo a needle biopsy and are told they have prostate cancer with a grade of Gleason 6.
The impact of this is quite profound. Most prostate cancer diagnosed today falls into this Gleason 6. If it is not cancer, thousands of men have had aggressive treatment for cancer they dont really have.
Aggressive treatment, usually a complete surgical removal of the prostate , is the typical result. This leaves the patient to suffer from its side effects for the rest of their life.
You May Like: How To Touch My Prostate
About Your Prostate Surgery
A radical prostatectomy is a surgery to remove your entire prostate gland and seminal vesicles. Some of the lymph nodes in your pelvis are removed as well. This is done to prevent cancer from spreading from your prostate to other parts of your body.
A radical prostatectomy can be done in 1 of 2 ways. One way is through an open incision , which is called an open prostatectomy. Another way is to use a laparoscope, which is a tube-like instrument with a camera. Your surgeon will talk with you about the best surgery option for you.
Open prostatectomy
In an open prostatectomy, your surgeon will make an incision that goes from your pubic bone towards your belly button . Theyll remove the pelvic lymph nodes first, followed by the prostate gland, and then the structures next to it.
Figure 2. Open prostatectomy incisions
Laparoscopic or robotic-assisted prostatectomy
During a laparoscopic or robotic-assisted prostatectomy, your surgeon will make several small incisions in your abdomen . Theyll insert a laparoscope into 1 of the incisions and use gas to expand your abdomen. Surgical instruments will be inserted into the other incisions to remove the prostate. Some surgeons at MSK are specially trained to use a robotic device to help with this procedure.
Figure 3. Laparoscopic or robotic-assisted prostatectomy incisions
What Does The Prostate Do
The prostate is a small muscular gland located between the base of the penis and the bladder, surrounding the urethra.
Its role is to secrete prostate fluid which is one of the components of semen.
The prostate’s main function is to produce the thick white fluid that mixes with the sperm produced in the testicles, to create semen.
The muscles of the prostate gland help propel this fluid into the urethra during ejaculation.
As men get older their prostate often enlarges.
Benign prostate enlargement causes men to urinate more frequently and is a common medical condition in men over 50.
BPE does not make a patient more likely to develop prostate cancer, however.
The causes of prostate cancer are largely unknown, although research suggests that it’s linked to obesity and family history.
You May Like: Can Prostate Cancer Cause Back Pain
What Do The Test Results Mean
PSA tests can be difficult to interpret. Tests can also vary from laboratory to laboratory. To ensure accurate comparison, its important to use the same lab each time youre tested.
If your PSA level is low and not rising after repeated tests, its probably not a cancer recurrence. Thats because other cells in your body can produce small amounts of PSA.
Ideally, your post-prostatectomy PSA will be undetectable, or less than 0.05 or 0.1 nanograms of PSA per milliliter of blood . If thats the case, your doctor may call it a remission.
If the result is greater than or equal to 0.2 ng/mL and its risen on two separate tests taken at least two weeks apart, its called a biochemical relapse. You still have PSA in your bloodstream. Theres a chance that cancer has recurred.
A PSA level higher than that may indicate a locally advanced tumor.
Bilateral Orchiectomy Or Surgical Castration
This is another type of prostate surgery, in which both testicles are removed. It is recommended in order to treat or prevent testicular cancer, prostate cancer, and male breast cancer. Bilateral orchiectomy lowers testosterone, the hormone that causes prostate and breast cancer to spread more quickly. By decreasing the levels of testosterone, cancer may spread at a lower rate, and some symptoms, such as bone pain, may be more tolerable.
This procedure usually lasts between 30 and 60 minutes and most people usually go home the day of the surgery, as it has a short recovery time.
Don’t Miss: How Accurate Is Mri In Diagnosing Prostate Cancer
What Is Urinary Incontinence And How Is It Related To Prostate Cancer Surgery
Urinary incontinence is the loss of the ability to control urination . Urinary incontinence sometimes occurs in men who’ve had surgery for prostate cancer.
If youve had prostate cancer surgery, you might experience stress incontinence, which means you might leak urine when you cough, sneeze or lift something that is heavy. This happens because of stress or pressure on the bladder. There is also a type of incontinence that is called urge incontinence. When this happens, you are hit with a sudden need to urinate right away and have leakage before you can make it to the bathroom.
What Is The Prostate Gland
The prostate gland is about the size of a walnut and surrounds the neck ofa man’s bladder and urethrathe tube that carries urine from the bladder.It’s partly muscular and partly glandular, with ducts opening into theprostatic portion of the urethra. It’s made up of three lobes, a centerlobe with one lobe on each side.
As part of the male reproductive system, the prostate gland’s primaryfunction is to secrete a slightly alkaline fluid that forms part of theseminal fluid , a fluid that carries sperm. During male climax, the muscular glands of the prostate help to propel the prostatefluid, in addition to sperm that was produced in the testicles, into theurethra. The semen then travels through the tip of the penis duringejaculation.
Researchers don’t know all the functions of the prostate gland. However,the prostate gland plays an important role in both sexual and urinaryfunction. It’s common for the prostate gland to become enlarged as a manages, and it’s also likely for a man to encounter some type of prostateproblem in his lifetime.
Many common problems that don’t require a radical prostatectomy areassociated with the prostate gland. These problems may occur in men of allages and include:
Cancer of the prostate is a common and serious health concern. According tothe American Cancer Society, prostate cancer is the most common form ofcancer in men older than age 50, and the third leading cause of death fromcancer.
You May Like: Open Mri For Prostate Scan
Msks Approach To Radical Prostatectomy
Our prostate surgery team includes experts in several techniques, including robot-assisted surgery, open surgery, and laparoscopic surgery. Regardless of which surgical approach you choose, our goal is to remove your cancer completely and preserve normal urinary and sexual function.
With all surgical approaches, weve developed and use innovative techniques to preserve the tiny nerves and blood vessels attached to the prostate that help control erections. These and other advances have made some of the complications of prostate cancer surgery less common and more manageable and can spare nerves from damage. Well work closely with you and your medical team to manage any short- or long-term side effects you may experience.
Ultimately, youll help determine which approach your surgeon takes.
