> > > One Crazy Prostate Trick All Men Over 40 Should Try
Symptomatic treatment of an enlarged prostate usually involves a combination of medication and lifestyle changes. A diet rich in fruits and vegetables may be the best option if you suffer from chronic urination. It will help the body adjust to the increased size of the prostate. Also, taking regular urination intervals will help retrain the bladder to function properly. Inactivity also contributes to urine retention, and cold temperatures can increase the urge to urinate.
Invasive treatment of enlarged prostate includes medication that relieves the pressure on the urethra and bladder. However, if the condition is severe, it may require surgical intervention. If treatment is not successful, the enlarged prostate can become a potentially life-threatening disease. As the hormone levels in the body change, the enlarged prostate can lead to various complications, including urinary retention and even cancer. This is why it is critical to see a doctor for further evaluation.
You May Like: How To Stimulate Your Prostate
Treatment Intensification For High
The STAMPEDE trial results showing a benefit to the addition of abiraterone to ADT in very high-risk localized and node positive disease has ignited interest in treatment intensification in this patient population.140
Multiple trials evaluating next generation androgen signaling inhibitors in high-risk clinically localized disease have either fully accrued or are currently accruing. For example, ENZARAD completed accrual in 2020, while PROTEUS, a randomized, double-blind, placebo-controlled, phase 3 trial of apalutamide plus ADT versus placebo plus ADT prior to radical prostatectomy in patients with localized high-risk or locally advanced prostate cancer, is recruiting at multiple centers internationally. Further, DASL-HiCaP is investigating the impact of the novel androgen receptor antagonist darolutamide on metastasis-free survival in very high-risk localized and biochemically recurrent/persistent disease.
Some Things To Consider When Choosing Among Treatments
Before deciding on treatment, here are some questions you may want to ask yourself:
- Are you the type of person who needs to do something about your cancer, even if it might result in serious side effects?
- Would you be comfortable with watchful waiting or active surveillance, even if it means you might have more anxiety and need more frequent follow-up appointments in the future?
- Do you need to know right away whether your doctor was able to get all of the cancer out ? Or are you comfortable with not knowing the results of treatment for a while if it means not having to have surgery?
- Do you prefer to go with the newest technology , which might have some advantages? Or do you prefer to go with better proven treatments that doctors might have more experience with?
- Which potential treatment side effects might be most distressing to you?
- How important for you are issues like the amount of time spent in treatment or recovery?
- If your initial treatment is not successful, what would your options be at that point?
Many men find it very stressful to have to choose between treatment options, and are very fearful they will choose the âwrongâ one. In many cases, there is no single best option, so itâs important to take your time and decide which option is right for you.
You May Like: Prognosis Of Prostate Cancer Spread To Bones
Also Check: How Do They Check For Prostate Cancer
Integrating Genomic Testing Into Practice
Results of somatic genomic testing can inform treatment in men with prostate cancer, explained Emmanuel S. Antonarakis, MD, Associate Professor of Oncology and Urology, The Johns Hopkins Sidney Kimmel Comprehensive Cancer Center, and Director of Prostate Cancer Medical Oncology Research.
Dr. Antonarakis went into greater detail regarding genomic testing. DNA repair mutations are found in prostate cancerboth single-strand repair and double-strand repair mutations , of which alterations in BRCA1/2 are the most common.
The prevalence of these mutations differs according to localized versus metastatic disease.8 In primary tumors, biallelic DNA repair gene mutations are found in approximately 8% to 10%, whereas they occur in about 20% to 25% of metastatic CRPC, he explained.
A recent paper analyzed DNA repair defects in ductal prostate cancer and found that 49% of patients had somatic DNA repair gene mismatches that were actionable .9 The 2019 version of the NCCN Guidelines recommends testing for HRD and for microsatellite instability or MMR deficiencies in all patients with metastatic prostate cancer. An increased prevalence of these mutations might be found in advanced ductal prostate cancers.
Prostate Cancer Mortality Rates In Low
To determine prostate cancer and other-cause mortality rates in low- and favorable intermediate-risk active surveillance patients.
The SEER Prostate with Watchful Waiting database was used to identify men diagnosed with NCCN low or FIR PCa, between 2010 and 2015, managed with AS. FIR patients were subdivided into three subgroups, based on their intermediate risk factor: grade group two , PSA 10-20 ng/ml or cT2b-c disease. Cumulative incidence function curves with other-cause mortality as the competing risk were utilized. Predictors of PCa mortality were assessed using multivariable regression analysis with semi-parametric proportional hazards modeling.
Among 70,871 patients, 48,127 had low and 22,744 had FIR disease. Median patient age was 64.0 years, and median PSA was 5.70 ng/ml. Median follow-up was 49.0 months. There were 166 PCa and 3,176 other-cause mortalities. The 5-year mortality rates in the low and FIR cohorts overall were 0.29% and 0.28%, respectively . Within the FIR cohort, the corresponding rates were highest in the PSA 10-20 ng/ml subgroup at 0.73%, followed by 0.32% for GG2 FIR and 0.052% for cT2b-c FIR disease . Older age at diagnosis , Medicaid insurance , low socioeconomic , and non-married statuses were associated with increased PCa mortality.
World journal of urology. 2022 Dec 06
Rashid K Sayyid, John Z Benton, William C Reed, Phillip Woodruff, Martha K Terris, Christopher J D Wallis, Zachary Klaassen
Also Check: Ben’s Natural Health Total Health For The Prostate
European Society Of Medical Oncology
The 2015 ESMO guidelines recommend watchful waiting with delayed hormone therapy as an option for localized disease or as an alternative for men with localized or locally advanced disease who are unwilling or unsuited for radical therapy.
Other recommended treatment options include :
-
Active surveillance for men with low-risk disease
-
Radical prostatectomy or radiotherapy for men with low- or intermediate-risk disease
-
Primary androgen deprivation therapy alone is not recommended for treatment of non-metastatic disease
-
For patients with high-risk or locally advanced prostate cancer, external beam RT plus hormone treatment or RP plus pelvic lymphadenectomy
Also Check: Preparation For Prostate Mri Scan
American Society Of Clinical Oncology/cancer Care Ontario Recommendations
ASCO and CCO released a joint clinical practice guideline for treatment of men with metastatic CRPC in 2014. The guideline recommendations include the following :
-
Pharmacologic androgen deprivation therapy should be continued indefinitely
-
Offer patients one of three treatment optionsabiraterone/prednisone, enzalutamide, or radium-223 in addition to hormone deprivation
-
When considering chemotherapy, docetaxel/prednisone should be an option but side effects must be discussed
-
Offer cabazitaxel to men whose disease worsens even if docetaxel has been tried, but again, discuss side effects
-
Offer sipuleucel-T to men with no symptoms or minimal symptoms of cancer
-
Offer mitoxantrone, but include a discussion of the drugâs limited clinical benefit and side effect risk
-
Offer ketoconazole or the anti-androgen therapies bicalutamide, flutamide or nilutamide but discuss the limited clinical benefit for these three medications
-
Do not offer the drugs bevacizumab , estramustine, or sunitinib
-
Begin discussion of palliative care early on while discussing treatment options
You May Like: What Happens When Prostate Removed
Intermediate Risk: Favorable Versus Unfavorable
The intermediate-risk group can be controversial. The current guidelines stratify intermediate-risk patients according to favorable versus unfavorable. Cancers in these 2 groups of patients behave differently, Dr. Mohler said.
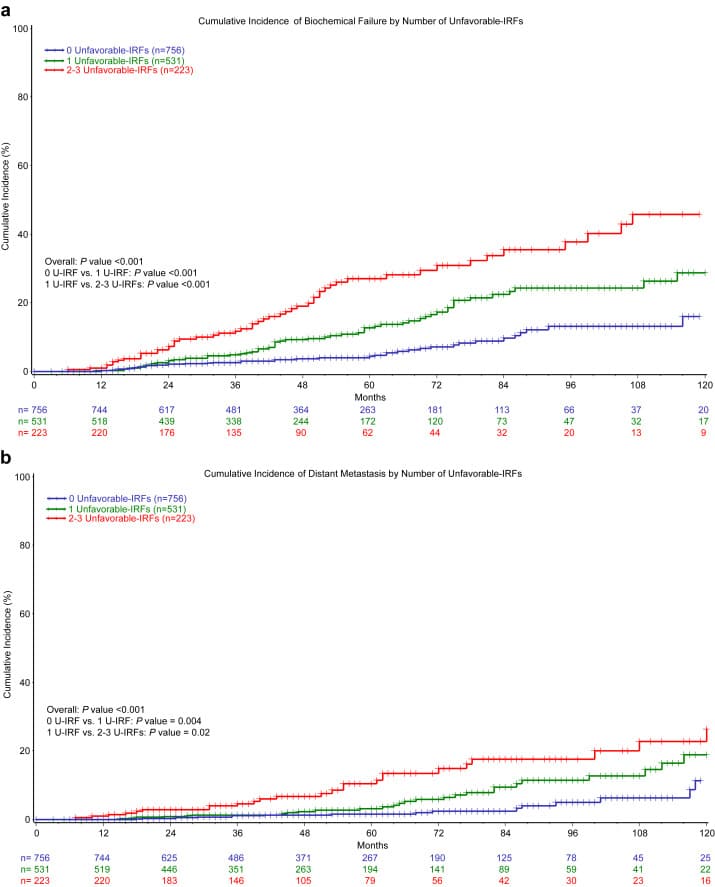
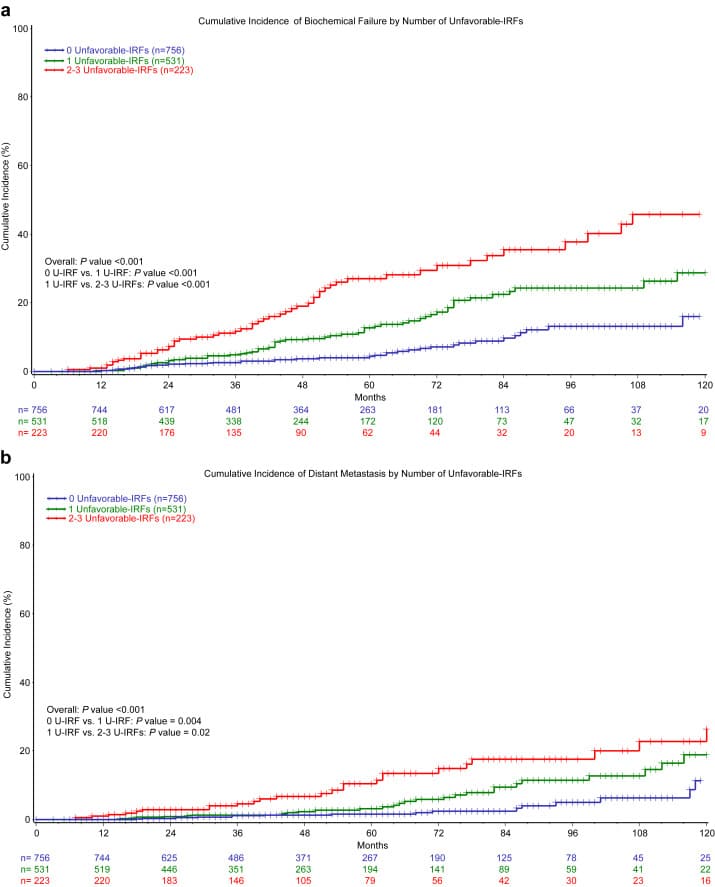
Favorable intermediate-risk patients have 1 intermediate risk factor, Grade Group 1 or 2 cancer, and < 50% of cores positive. Unfavorable intermediate-risk patients have 2 or 3 intermediate risk factors, and/or Grade Group 3 prostate cancer, and/or 50% of biopsy cores positive.
We need to apply caution here. We believe active surveillance should be offered to men with favorable intermediate-risk prostate cancer, but this needs to be considered carefully, he told the audience.
Active surveillance in this setting may include a molecular-based test, 3P MRI, restaging prostate biopsy, surveillance 3P MRI, surveillance prostate biopsies, some combination thereof, or prospective clinical trials.1
Most Patients On Sbrt For Localized Prostate Cancer Do Not Receive Concurrent Adt Despite Nccn Guidelines
Most patients in the United States who receive stereotactic body radiation therapy for unfavorable intermediate- or high-risk localized prostate cancer are not receiving concurrent androgen-deprivation therapy , despite national guideline recommendations that support the concurrent use of ADT with radiation therapy.
Among patients aged > 40 years with localized prostate cancer who received radiation therapy between 2004 and 2015, the use of ADT decreased among those who were considered low risk, favorable intermediate risk, or unfavorable intermediate risk, according to an analysis of data from the National Cancer Database. The use of ADT increased over time only among men with high-risk disease, reported Trevor J. Royce, MD, MPH, MS, Assistant Professor, Department of Radiation Oncology, University of North Carolina at Chapel Hill, and colleagues, in a poster presentation at the 2020 Genitourinary Cancers Symposium.
In general, because there is the potential for quality-of-life effects from ADT, best practice is to use it when there is a proven benefit, noted Dr Royce and colleagues. To be clear, ADT is an extraordinarily effective approach for treating prostate cancer, its just that as clinicians we aim to be judicious with its application.
Although SBRT is noninferior to conventional radiation for tumor control and toxicity, and noninferior to moderate hypofractionation for toxicity, the benefit of ADT combined with SBRT is unknown.
Don’t Miss: Female Hormones For Prostate Cancer
Combination Therapy For Prostate Cancer
Sean McBride, MD, MPH · Memorial Sloan Kettering Cancer Center
Key Takeaways:
-
In men with localized or local-regional prostate cancer, the most commonly used combination treatment is radiation plus androgen deprivation therapy , with a key consideration being the duration of ADT.
-
Results of a recent study have suggested that patients with very-high-risk prostate cancer may benefit more from the addition of orally administered abiraterone than from the use of more traditional injection-based ADT .
-
The US Food and Drug Administration recently approved the orally administered ADT relugolix, which is often used to treat men with prostate cancer and significant cardiac comorbidities, and those who wish to preserve sexual function.
This transcript has been edited for clarity.
In terms of combination therapy for localized or local-regional prostate cancer thats getting treated with radiation, the most common combination therapy to use is androgen deprivation therapy. The critical question thats often involved with androgen deprivation therapy when combined with radiation is, the length of time that androgen deprivation is delivered?
That depends largely on whats called the risk classification for prostate cancer. Most oncologists in the United States use the NCCN risk classification. Theres very-low-risk, low-risk, favorable intermediate-, unfavorable intermediate-, high-risk, and very-high-risk prostate cancer.
Primary Outcomes: Mortality And Metastasis
Of the 1,298 men who received follow-up, 49 died . Thirty-eight men died as a result of causes other than prostate cancer before reclassification or treatment, and nine men died as a result of causes other than prostate cancer after being treated for prostate cancer. Death occurred at a median age of 75.5 years , and the most common overall cause of death was cardiovascular disease. The 47 men who died as a result of causes other than prostate cancer were receiving AS for a median of 7.0 years before their deaths.
Also Check: Gleason Score 7 Prostate Cancer Treatment Options
Focal Therapy For Prostate Cancer
With recent advances in MRI and targeted biopsy, we are better able to locate the exact area of prostate cancer. Men who do not have an enlarged prostate, who have prostate cancer that is detected only in a single region of the prostate and have intermediate grade cancer can be a candidate for focal therapy. This type of therapy treats only the cancerous tissue and spares the normal prostate, thereby preserving urinary and sexual function
Here at UCLA we commonly use cryotherapy or HIFU to focally treat prostate cancer. Given that this is a relatively new form of treatment, we have established rigorous post-treatment protocols using MRI and biopsies to ensure that the cancer has been adequately treated.
Variation In National Use Of Long
Background: The current NCCN Clinical Practice Guidelines in Oncology for Prostate Cancer recommend long-term androgen deprivation therapy for all men with high-risk prostate cancer treated with external-beam radiation therapy . We determined whether the use of long-term ADT varied by the recently defined subcategories of high-risk disease versus unfavorable intermediate-risk disease. Methods: We identified 5,524 patients with unfavorable-risk prostate cancer diagnosed from 2004 to 2007 and managed with EBRT using the SEER-Medicare linked database. Patients were stratified by risk group: unfavorable intermediate-risk, favorable high-risk , very-high-risk , or other high risk . We used multivariable competing risks regression to estimate the rates of long-term ADT by group. Results: Men with favorable high-risk prostate cancer were significantly less likely to receive long-term ADT than those with other high-risk disease , and similarly likely as those with unfavorable intermediate-risk disease . Other high-risk disease was less likely to receive long-term ADT than very high-risk cancer . Despite current guidelines, patients with EBRT-managed high-risk prostate cancer received significantly different rates of long-course ADT based on subclassification. Our results suggest that oncologists view these patients as a heterogeneous group with favorable high-risk cancer warranting less aggressive therapy than other high-risk or very high-risk disease.
Read Also: What Are Side Effects Of Radiation Therapy For Prostate Cancer
About Dr Dan Sperling
Dan Sperling, MD, DABR, is a board certified radiologist who is globally recognized as a leader in multiparametric MRI for the detection and diagnosis of a range of disease conditions. As Medical Director of the Sperling Prostate Center, Sperling Medical Group and Sperling Neurosurgery Associates, he and his team are on the leading edge of significant change in medical practice. He is the co-author of the new patient book Redefining Prostate Cancer, and is a contributing author on over 25 published studies. For more information, contact the Sperling Prostate Center.
Search the spc blog
Matching Treatment For Favorable Risk Prostate Cancer
Today, the majority of PCa cases are diagnosed early thanks to PSA screening coupled with noninvasive multiparametric MRI tumor detection. It therefore makes sense that for those with Gleason 3+3 and some with Gleason 3+4, the conditions are favorable for a successful minimalist approach to managing the disease, including treatment and AS. These are considered favorable low-risk and favorable intermediate-risk prostate cancers. When carefully diagnosed and qualified, these patients may safely hold off on such aggressive radical treatments provided they protect themselves by adhering to monitoring protocols.
Read Also: Best Treatment For Recurrent Prostate Cancer
Intermittent Versus Continuous Adt
Always think about intermittent ADT, Dr. Mohler continued. Several studies have compared these 2 approaches. The best analysis found no survival benefit for continuous versus intermittent ADT. No subgroup favors continuous ADT, and quality of life is better during the off cycle, he stated.
A large meta-analysis of 6 randomized trials comprised of 2,996 men found similar OS for intermittent versus continuous ADT, with improved QoL associated with intermittent ADT.3
SWOG 9346 found that continuous ADT was associated with approximately a 6-month advantage in survival versus intermittent ADT in metastatic hormone-sensitive prostate cancer but with a worse QoL.4 At a median follow-up of 9.8 years, median OS 5.1 years in the intermittent therapy group.
The panel softened our recommendations some time ago to consider intermittent ADT in all men with nonmetastatic prostate cancer and also to consider it in metastatic disease. I believe intermittent ADT should be considered in everyone. ADT can be personalized according to end-of-induction prostate-specific antigen levels, Dr. Mohler said.
Why Is Risk Level Important
Risk level is all about matching the right treatment to the right patient, so its very important!
The idea of classifying PCa according to risk was originally based on the relative risk of PSA failure after prostatectomy or radiation. Until the late 1990s, the only conceivable treatment options were either whole gland surgery or radiation, and watchful waiting . The standard risk classification was the DAmico system:
- Low risk defined as stage T1c, T2a and PSA level 10 ng/mL and Gleason score 6
- Intermediate risk defined as stage T2b or Gleason score of 7 or PSA level > 10 and 20 ng/mL
- High risk defined as stage T2c or PSA level > 20 ng/mL or Gleason score 8.
Don’t Miss: Can You Get Prostate Cancer After Having Your Prostate Removed
Similar Articles Being Viewed By Others
Carousel with three slides shown at a time. Use the Previous and Next buttons to navigate three slides at a time, or the slide dot buttons at the end to jump three slides at a time.
12 December 2018
Hyung L. Kim, Ping Li, Tarek A. Bismar
08 June 2022
Yanhong Yu, Katherine Lajkosz, Michelle R. Downes
02 October 2018
Jeffrey J. Tosoian, Liana B. Guedes, Tamara L. Lotan
27 June 2019
Stefano Luzzago, Michele Catellani, Ottavio de Cobelli
20 July 2021
Randy A. Vince Jr., Ralph Jiang, Todd M. Morgan
12 November 2019
Joseph Marascio, Daniel E. Spratt, Robert B. Den
I Have Heard That Other Factors May Be Included When Evaluating Treatment
Yes, other factors such as the number of biopsies and the presence of Gleason Score 7 versus a Gleason Score may influence the treatment decision. The number of + biopsies is also strongly predictive of outcomes but not typically part of the risk grouping systems. An example would be a person with a multiple + biopsies Gleason 7. His cancer would be considered a High Intermediate Risk and require a combination of External Beam and radiation while another patient with only a few + biopsies could be a Low Intermediate Risk patient and be a good candidate for an implant alone. These factors should be discussed with you doctor.
©2013 Prostate Cancer Center of Seattle | All Rights Reserved | P 1.877.330.7722 OR 206.453.2992 |
Read Also: How To Stop Incontinence After Prostate Removal
