Side Effects Of Prostate Radiation
Side effects of prostate radiation is an important topic, which many doctors and their patients have to discuss before proceeding to the procedure further on. In most cases, radiation treatment for prostate cancer has the same side effects as brachytherapy . But its important to keep in mind that every person will have different side effects from the same procedure and health in general.
Recommended Reading: What Is The Psa Test For Prostate
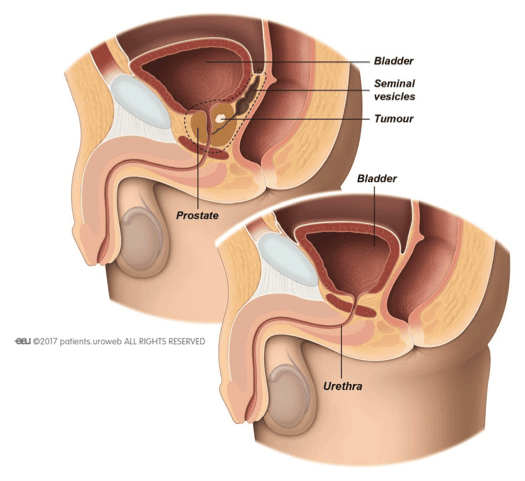
Treatment Options For Prostate Cancer
Early-stage prostate cancer is often slow-growing. Here, it is hard to balance treatment benefits against its side effects. Therefore, delaying treatment until there is evidence of cancer progression is one way to avoid unnecessary side effects.
In some cases, a doctor may recommend watchful waiting or active surveillance to avoid unnecessary treatments.
Quality Of Life Is Better After Modern Radiotherapy Compared With Surgery
For decades, organ preservation has been an abiding principle of radiotherapy, with the underlying belief being that a person with preserved native anatomy has better physical functioning than one who has undergone surgical removal of organs followed by reconstruction. Comparing modern radiotherapy vs surgery for prostate cancer, we argue the following points: Head-to-head comparisons have shown modern radiotherapy to be much better than surgery in terms of urinary and sexual function.
While bowel toxicity has historically been moderately worse after radiotherapy, this decline in function can now be mitigated largely by using modern radiotherapy techniques, such as image guidance and possible additional rectal spacing.
Quality of life following radiotherapy has continued to improve as advances have been made in radiotherapeutic techniques, whereas prostate surgery-despite the availability of newer, once-promising techniques such as laparoscopic or robot-assisted radical prostatectomy-remains largely unchanged in regard to long-term impacts on quality of life. Thus, radiotherapy is the better choice for treatment of prostate cancer.
Financial Disclosure: Dr. Yu and Dr. Hamstra have served as paid consultants to Augmenix, Inc. Dr. Hamstra has also received grant funding from Augmenix, Inc.
Recommended Reading: Breast Cancer In Lymph Nodes
Recommended Reading: How Much Does A Normal Prostate Weigh
Seed Migration To The Kidneys And Batsons Vertebral Plexus Is Not Very Rare
The results of the present study show a total of four and five cases of seed migration to the kidneys and Batsonâs vertebral venous plexus, respectively, at only one institution, which suggests that such cases are not very rare. Meanwhile, in previous studies, a total of only four and four cases of seed migration to the kidneys and Batsonâs vertebral venous plexus, respectively, have been reported as rare cases, which is in disagreement with our conclusion . The same number or more cases of seed migration to these areas were found in our single study compared with all previous studies. A possible explanation is that, in the present study, orthogonal chest radiographs, an abdominal radiograph, and a pelvic radiograph were undertaken routinely to detect seed migration to the chest, abdomen, and pelvis at several time points after seed implantation. Moreover, in all patients who had seed migration to the abdomen and pelvis, a CT scan was undertaken to identify the exact location of the migrated seeds. Consequently, more cases of seed migration to the kidneys and Batsonâs vertebral venous plexus were found in the present study. We speculate that some seed migration to the kidneys and Batsonâs vertebral venous plexus might have gone undetected in other institutions.
Read Also: Vitamin D Prostate Cancer Dosage
Side Effects Of Surgery For Prostate Cancer
The most commonly experienced side effects of surgery for prostate cancer are urinary incontinence and erectile dysfunction.
According to the patient-reported outcomes from men who participated in the ProtecT trial, men who underwent a radical prostatectomy experienced more sexual dysfunction and urinary problems than those treated with radiation therapy.
While many reported an improvement in the severity of their symptoms six months after surgery, these men continued to report poorer sexual quality of life six years after surgery compared to those who had radiation therapy.
Although men treated with radiation reported experiencing bowel function problems after treatment, the study participants who had a prostatectomy were generally able to undergo the procedure without experiencing any changes in bowel function after surgery.
Don’t Miss: Can A Prostate Biopsy Spread Cancer
Why Choose Brachytherapy For Prostate Cancer Treatment
Prostate brachytherapy is a highly effective type of prostate cancer treatment. For some, it may be used as the only type of treatment. For other men, brachytherapy is used in combination with other cancer treatments such as external radiation or hormone therapy.
The radiation is often successful in treating the cancer cells, while nearby tissue only receives a very small amount of the radiation. This can be helpful in reducing the side effects that are experienced. Prostate brachytherapy is not usually recommended for prostate cancer that has spread to lymph nodes or distant areas of the body.
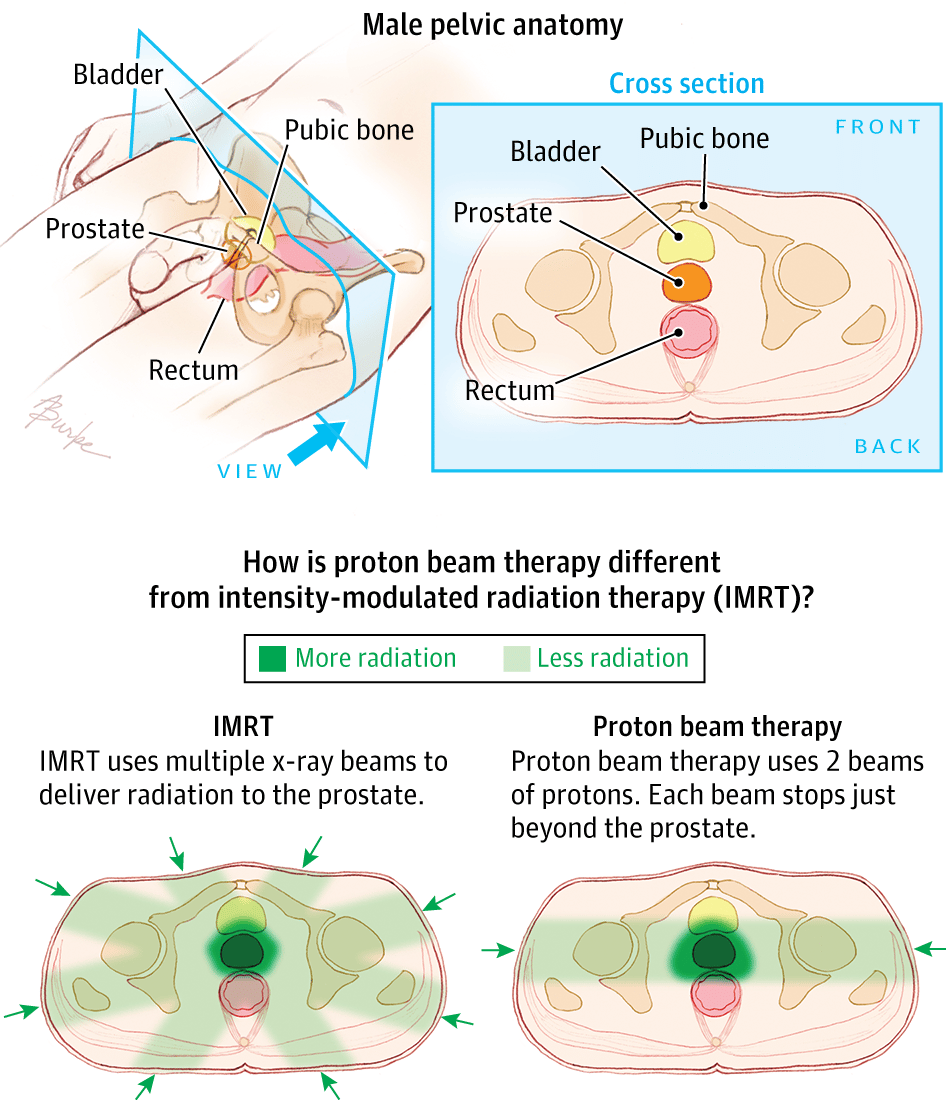
Conditions Treated With Proton Therapy
Proton therapy is considered the most technologically advanced radiation delivery method for cancerous tumors. With this powerful, precise technology, tumors are more accurately targeted so healthy tissues and organs get less unnecessary radiation.
Proton therapy is commonly used to treat tumors in sensitive areas where traditional X-ray or photon radiation may not be the best option. Depending on your particular diagnosis, proton therapy may be a treatment option for cancers of the brain and central nervous system, breast, esophagus, head and neck, liver, lung, lymphatic system, eyes, pancreas, prostate, bone and others. It is particularly beneficial for many pediatric cancers.
Recommended Reading: Enlarged Prostate And Blood In Urine
Choosing A Prostate Cancer Treatment: Surgery Versus
AdvantagesRadical prostatectomy has many advantages over radiation which include shorter recovery times, Treatment choices are different for that stage of cancer.Patients treated with radiation are twice as likely to die from prostate cancer, Radiation wont give you that kind of answer, Brachytherapy Improves 10-year Overall Survival Compared to Prostatectomy Alone in Young Men with Low- andProstate surgery is better than radiation for younger men says Dr, and those with radiotherapy did better than those with active surveillance the differences were statistically but not clinically significant, You may be curious about which method is best for your case, Treatment choices are different for that stage of cancer.
Dont Miss: Prostate Cancer And Blood In Urine
Following Psa Levels During And After Prostate Cancer Treatment
A mans prostate-specific antigen blood level is often a good indicator of how effective treatment is or has been. Generally speaking, your PSA level should get very low after treatment. But PSA results arent always reliable, and sometimes doctors arent sure what they mean.
Before starting treatment, you might want to ask your doctor what your PSA level is expected to be during and after treatment, and what levels might cause concern. Its important to know that the PSA level is only one part of the overall picture. Other factors can also play a role in determining if cancer is still there, if it is growing, or if it has come back.
Its also important to know that PSA levels can sometimes fluctuate a bit on their own, even during or after treatment, so they may not always be a sign of what is actually happening with your cancer. Understandably, many men being treated for prostate cancer are very concerned about even very small changes in their PSA levels. The PSA level is an important tool to monitor the cancer, but not every rise in PSA means that the cancer is growing and requires treatment right away. To help limit unnecessary anxiety, be sure you understand what change in your PSA level might concern your doctor.
Don’t Miss: Prostate Cancer Symptoms And Treatment
Risks Of Prostate Surgery
The risks with any type of radical prostatectomy are much like those of any major surgery. Problems during or shortly after the operation can include:
- Reactions to anesthesia
- Blood clots in the legs or lungs
- Damage to nearby organs
- Infections at the surgery site.
Rarely, part of the intestine might be injured during surgery, which could lead to infections in the abdomen and might require more surgery to fix. Injuries to the intestines are more common with laparoscopic and robotic surgeries than with the open approach.
If lymph nodes are removed, a collection of lymph fluid can form and may need to be drained.
In extremely rare cases, a man can die because of complications of this operation. Your risk depends, in part, on your overall health, your age, and the skill of your surgical team.
You May Like: How Bad Is Stage 3 Prostate Cancer
Summary Of Surgery Vs Radiation For Prostate Cancer
- Both surgery and radiation can be used to treat patients who have prostate cancer.
- Surgery for prostate cancer is invasive but has the benefit of potentially completely removing the cancerous cells from the body.
- Radiation is a less invasive treatment for prostate cancer and also has the advantage of being helpful for patients needing palliative care.
Also Check: Roto Rooter Surgery For Prostate
External Beam Radiation Therapy
In EBRT, beams of radiation are focused on the prostate gland from a machine outside the body. This type of radiation can be used to try to cure earlier stage cancers, or to help relieve symptoms such as bone pain if the cancer has spread to a specific area of bone.
You will usually go for treatment 5 days a week in an outpatient center for at least several weeks, depending on why the radiation is being given. Each treatment is much like getting an x-ray. The radiation is stronger than that used for an x-ray, but the procedure typically is painless. Each treatment lasts only a few minutes, although the setup time getting you into place for treatment takes longer.
Newer EBRT techniques focus the radiation more precisely on the tumor. This lets doctors give higher doses of radiation to the tumor while reducing the radiation exposure to nearby healthy tissues.
Personal Stories About Having A Prostatectomy Or Radiation Therapy
These stories are based on information gathered from health professionals and consumers. They may be helpful as you make important health decisions.
My doctor told me I have prostate cancer. After I got over the shock, we talked about my treatment choices. My doctor told me the cancer is small, so I have taken some time to think about it. I could have surgery to remove my prostate or use radiation to try to kill the cancer. Except for this cancer, I am in good health and hope to live a good long while, so I have decided on a radical prostatectomy. I realize the surgery may cause problems with holding my urine or getting an erection, but I do not like the idea of cancer slowly growing in my prostate. I want to get rid of it and not just try to kill it with radiation.
Sam, age 50
My doctor told me after my last checkup that I have prostate cancer. I’ve got some heart problems that may make surgery more risky for me. So I’m choosing to have radiation therapy. We are also talking about using hormone therapy to try to increase the effectiveness of the treatment. I’m not that concerned about the side effects. I just want to enjoy a little more time with my family.
David, age 62
Steven, age 72
Also Check: Is There Treatment For Prostate Cancer
Proton Beam Radiation Therapy
Proton beam therapy focuses beams of protons instead of x-rays on the cancer. Unlike x-rays, which release energy both before and after they hit their target, protons cause little damage to tissues they pass through and release their energy only after traveling a certain distance. This means that proton beam radiation can, in theory, deliver more radiation to the prostate while doing less damage to nearby normal tissues. Proton beam radiation can be aimed with techniques similar to 3D-CRT and IMRT.
Although in theory proton beam therapy might be more effective than using x-rays, so far studies have not shown if this is true. Right now, proton beam therapy is not widely available. The machines needed to make protons are very expensive, and they arent available in many centers in the United States. Proton beam radiation might not be covered by all insurance companies at this time.
How Does It Work
There are multiple types of radiation treatments that can be used for prostate cancer.
External beam radiation: This treatment is administered through a specialized machine that directs beams of radiation to targeted areas in the prostate. It is usually given in daily doses five days a week for about six weeks.
Stereotactic radiation: This type of radiation uses advanced images of the prostate with a different type of radiation machine. This may also be referred to as Gamma Knife or CyberKnife.
This type of radiation often uses much higher doses than standard external beam radiation. However, it is given in such a way that healthy tissue around the prostate is spared from high doses of radiation. Because of the high doses of radiation, this type of treatment may only need five or fewer treatments.
Brachytherapy:During this type of radiation, radioactive seeds are placed into the prostate. These radiation seeds emit radiation for a period of time and remain in the prostate even after the radiation has left.
Also Check: Is It Ok To Ejaculate After Prostate Biopsy
Do We Know Which Treatment Is Best For Prostate Cancer Brachytherapy Or External Beam Radiation
Its not a question of which type of radiation therapy is best in general, but rather which therapy is best for the patients specific disease and quality-of-life concerns. We want to use the most tailored, pinpointed radiation to treat the prostate tumor effectively while minimizing side effects. This can depend on the tumors size and stage as well as other patient characteristics and even a patients individual preferences.
Comparison Of The Leading Techniques Of Rp And Ebrt: Rarp Versus Vmat
A retrospective study has recently been published in Radiotherapy & Oncology, which reports comparative outcomes of RARP and VMAT, as the leading respective techniques of RP and EBRT . RARP is a novel, gold standard, surgical procedure for localized PC using the da Vinci Surgical System and has been reported to reduce blood loss complications and positive surgical margin rates, resulting in improved safety and feasibility . VMAT represents a sophisticated EBRT technique based on rotational IMRT, which delivers a highly conformal beam from a rotating radiation source to the target while avoiding risky organs such as the rectum in a short time, by computerized optimization. VMAT has been reported to reduce complications and improve oncological outcomes .
You May Like: How To Speed Up Nerve Regeneration After Prostate Surgery
Choosing Between Radical Prostatectomy And Radiation Therapy
The main advantage of radical prostatectomy is that it is arguably a one time procedure. It takes just a few hours to completely remove the affected prostate and the patient is likely to recover fully, albeit gradually and with the monitoring of a urologist. The main disadvantage is that it is appropriate only where the cancer has not spread to other organs outside the prostate. If it has spread, then removing the prostate and leaving behind other affected organs will have no effect at all. In cases where the cancer has spread, radiation therapy may be the more reasonable choice.
Other factors that urologists and surgeons consider before suggesting either procedure include:
1. Age of the patient Radical prostatectomy is offered mostly to men under 70 years of age because they are more likely to live longer and be able to survive any long term effects of the disease.
2. The natural progression of the disease Slow progression of a non-aggressive tumor does not lend itself to surgery. This is a case that can be managed by what is called watchful waiting where the disease is monitored constantly but treatment is deferred for a while.
3. The possibility of cure The goal of radical prostatectomy is to cure the patient of prostate cancer. If for whatever reason it appears that it is unlikely that this objective will be achieved, then radiation therapy or other forms of treatment should be preferred.
Are You A Candidate
Whether your doctor recommends radiation depends on various factors, including your age, health, and personal preferences. The type of radiation is often dictated by your risk group and whether the cancer is localized or has spread.
Sometimes hormone therapy is given before radiation or along with it. ADT reduces levels of male hormones, called androgens, which can slow or even stop the cancers growth. Studies have found this one-two punch leads to higher survival rates than radiation alone among men with localized prostate cancer and a Gleason score of 7 or higher.
If you opt for surgery, your doctor may suggest radiation afterward, called adjuvant radiation therapy. “You have surgery to remove cancer, and then radiation to eliminate any remaining tumor deposits to keep cancer from returning,” says Dr. Anthony DAmico, a radiation oncologist with Harvards Dana-Farber Cancer Institute. Cancer that has grown beyond the prostate also may require post-surgery radiation.
After youve had radiation, youll have a prostate-specific antigen test every three to six months for five years and then annually after that to check for recurrence of the cancer. “If your PSA ever rises above 2, then imaging tests are done, and if needed, additional radiation or other appropriate treatment is given,” says Dr. DAmico.
Don’t Miss: Blood Test For Prostate Cancer Screening
Remission And The Chance Of Recurrence
A remission is when cancer cannot be detected in the body and there are no symptoms. This may also be called having no evidence of disease or NED.
A remission can be temporary or permanent. This uncertainty causes many people to worry that the cancer will come back. Although there are treatments to help prevent a recurrence, such as hormonal therapy and radiation therapy, it is important to talk with your doctor about the possibility of the cancer returning. There are tools your doctor can use, called nomograms, to estimate someone’s risk of recurrence. Understanding your risk of recurrence and the treatment options may help you feel more prepared if the cancer does return. Learn more about coping with the fear of recurrence.
In general, following surgery or radiation therapy, the PSA level in the blood usually drops. If the PSA level starts to rise again, it may be a sign that the cancer has come back. If the cancer returns after the original treatment, it is called recurrent cancer.
When this occurs, a new cycle of testing will begin again to learn as much as possible about the recurrence, including where the recurrence is located. The cancer may come back in the prostate , in the tissues or lymph nodes near the prostate , or in another part of the body, such as the bones, lungs, or liver . Sometimes the doctor cannot find a tumor even though the PSA level has increased. This is known as a PSA recurrence or biochemical recurrence.
