Baseline Characteristics And Vas Pain Scores According To Pnb Sites
Patient characteristics and VAS pain scores according to PNB sites are presented in Table . No differences in PSA concentrations , prostate volume , or prostate cancer detection rate were observed between the base-only PNB group and the base and apex PNB group. There were no significant differences in VAS pain scores among the different time points . Average pain scores at the base, mid, and apex sites are presented in Table . The average VAS pain score across all regions in the base and apex PNB group was lower than that in the base-only PNB group.
Table 1 Baseline characteristics and VAS pain scores according to the PNB sites
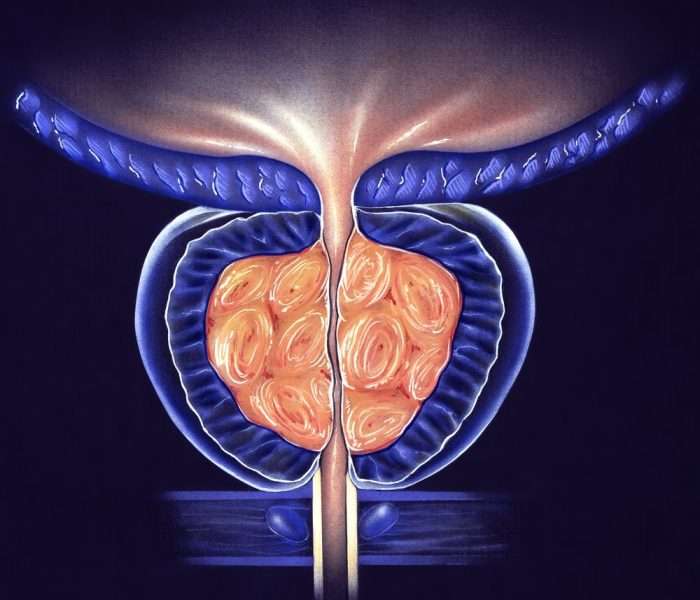
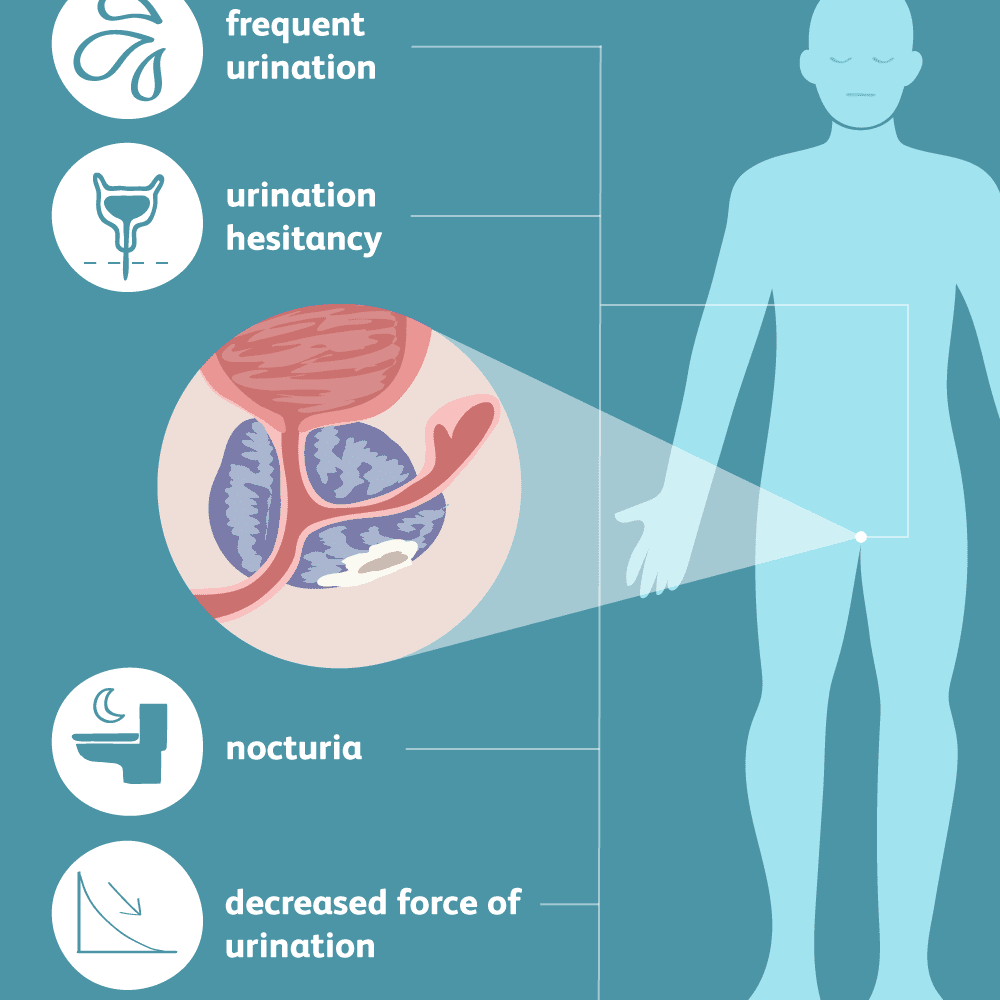
Signs And Symptoms Of Prostate Cancer
What kind of anesthesia is used for prostate biopsy?
Are you put to sleep for a prostate biopsy?
How painful is a prostate biopsy?
How long does a prostate biopsy take?
Signs and symptoms of prostate cancer
Most prostate cancers are found early, through screening. Early prostate cancer usually causes no symptoms. More advanced prostate cancers can sometimes cause symptoms, such as:
- Problems urinating, including a slow or weak urinary stream or the need to urinate more often, especially at night
- Trouble getting an erection
- Pain in the hips, back , chest , or other areas from cancer that has spread to bones
- Weakness or numbness in the legs or feet, or even loss of bladder or bowel control from cancer pressing on the spinal cord
Most of these problems are more likely to be caused by something other than prostate cancer. For example, trouble urinating is much more often caused by benign prostatic hyperplasia , a non-cancerous growth of the prostate. Still, its important to tell your health care provider if you have any of these symptoms so that the cause can be found and treated, if needed. Some men might need more tests to check for prostate cancer.
Read Also:
What Are Some Common Uses Of The Procedure
A prostate biopsy is currently the only way to definitively diagnose prostate cancer. It also helps differentiate cancer from benign prostatic hyperplasia or nodular enlargement of the prostate, a very common condition in middle-aged and older men that requires a different treatment approach than that of cancer.
A prostate biopsy may be ordered if the physician detects a nodule or other abnormality on the prostate during a digital rectal examination , a common prostate cancer screening test.
A biopsy also may be ordered when a blood test reveals elevated levels of prostate-specific antigen. While there are several reasons for an elevated PSA level, higher PSA levels are sometimes associated with cancer. PSA trends over time may trigger your physician to order a biopsy.
MRI-guided prostate biopsy may be used in patients who have a rising PSA level yet a negative ultrasound-guided biopsy. It also may be used in situations where a diagnostic prostate MRI performed due to rising PSA demonstrates a very small abnormality that may not be easily targeted by ultrasound. MRI is also useful in patients who have previously undergone a biopsy and want to improve the sensitivity of the procedure and the precision of the biopsy.
A biopsy not only detects cancer it also provides information on the aggressiveness of the cancer and helps to guide treatment decisions.
You May Like: How To Reduce Prostate Swelling Naturally
Don’t Miss: What Causes Prostate Cancer In Men
Who Interprets The Results And How Do I Get Them
A pathologist examines the removed tissue specimens and makes a final diagnosis. The results usually are available to your physician within a few days of the procedure. The time it takes may vary based on the complexity of the examination, preparation time for the specimens, need for a second opinion and other factors.
Koelis Technology For Prostate Cancer Biopsies
For over a decade KOELIS® has assisted urologists and radiologists from around the world in their routine clinical practice providing the latest technology. In order to bring personalized answers to every patient in the respect of their quality of life, weve developed KOELIS Trinity® the first image-based cartographer. This system allows physicians to perform targeted transperineal or transrectal MRI/US fusion-guided biopsies under local or general anesthesia.
Quality management in patient diagnosis
It is equipped with the exclusive Organ-Based Tracking Fusion® technology which enhances the accuracy of the biopsy. Without changing the usual clinical practices, this technique brings an increased quality control over biopsy localizations. A precise, individual prostate biopsy mapping is a value for the accurate diagnosis and the further management of each patient.
To locate a clinic equipped with our solutions: Discover our interactive map.
Recommended Reading: How To Kill Prostate Cancer
Does The Prostate Swell After A Biopsy
When it comes to inflammatory responses, people differ. No matter how small, any trauma will cause local inflammation, and the prostate will swell a bit. However, in some individuals, this swelling may be more than in others.
This swelling of the prostate can make urinating difficult for individuals. Generally, this swelling would not last long. Nonetheless, your healthcare provider would recommend urinating before the procedure.
For most people, the swelling would last for a few hours. However, if it lasts longer, it may cause urinary retention or a problem peeing. In such instances, doctors may need to insert a catheter.
How To Get The Best Results
Most men do not find prostate biopsy excessively painful or uncomfortable, and the complications are usually not seriousbut can be. Certain steps taken before, during, and after the procedure can improve the outcome:
Take antibiotics. Taking preventive antibioticsbefore and after the procedurecuts the risk of infection substantially. Most infections are not dangerous but could become so if they get out of control. The overall chance of being hospitalized with an infection after prostate biopsy is 1% to 3%.
Review medications. Before the biopsy, your doctor may advise you to stop taking daily low-dose aspirin or an anticoagulant such as warfarin , dabigatran , edoxaban , rivaroxaban , or apixaban . These drugs reduce the blood’s ability to clot. Your doctor will weigh the chance of bleeding against the need for anticoagulants to prevent heart problems or stroke.
Expect anesthesia. Get local anesthesia for the biopsy. This means an injection of a numbing drug into the prostate gland to reduce pain during the biopsy.
Read Also: How To Decalcify The Prostate
What Are The Side Effects Of A Transperineal Biopsy
Side effects of a transperineal biopsy generally include:
- Blood in the urine
Patients can experience discomfort during the placement of the anesthetic. This feeling is like the burning sensation when a dentist works on a tooth. Unlike the transrectal prostate biopsy approach, there is no risk of rectal bleeding as the needle does not go through the rectal wall.
Benefits Of Getting A Prostate Biopsy
A prostate biopsy is the only way to definitively determine whether you have prostate cancer and, if you do, how aggressive it is.
While prostate biopsies arent always conclusive, in general, a biopsy gives men the reassurance of knowing whether they have cancer or not. If you know you have prostate cancer, youre more likely to be appropriately treated.
Appropriate prostate cancer treatment options depend on several factors, including the stage of the cancer, your age, your general health and which risk category your cancer falls into.
Localized prostate cancer is categorized into six risk categories, which range from very low-risk to very high-risk. The risk group is determined by the stage of your cancer, your PSA levels and the Gleason score obtained from the biopsy pathology report.
The National Comprehensive Cancer Network guidelines outline appropriate treatment options based on risk categories and whether the cancer has already metastasized.
Patients whose cancer is confined to the prostate and falls into the very low-risk and low-risk categories tend to have slow-growing cancers. Treatment options for these patients often include active surveillance, radiation therapy or surgery. Similar treatment options may be recommended to patients in the low-risk and favorable intermediate prostate cancer risk categories.
The NCCN guidelines recommend immediate treatment for patients with high-risk disease or those patients whose cancer has metastasized.
Also Check: How Do They Test For Prostate Cancer
What Is A Transperineal Biopsy
This is where the doctor inserts the biopsy needle into the prostate through the skin between the testicles and the back passage . In the past, hospitals would only offer a transperineal biopsy if other health problems meant you couldnt have a TRUS biopsy. But many hospitals have stopped doing TRUS biopsies and now only do transperineal biopsies.
A transperineal biopsy is normally done under general anaesthetic, so you will be asleep and wont feel anything. A general anaesthetic can cause side effects your doctor or nurse should explain these before you have your biopsy. Some hospitals now do transperineal biopsies using a local anaesthetic, which numbs the prostate and the area around it, or a spinal anaesthetic, where you cant feel anything in your lower body.
The doctor will put an ultrasound probe into your back passage, using a gel to make this easier. An image of the prostate will appear on a screen, which will help the doctor to guide the biopsy needle.
If youve had an MRI scan, the doctor may just take a few samples from the area of the prostate that looked unusual on the scan images. This is known as a targeted biopsy.
Prepping Before The Procedure
At least a week before your prostate biopsy procedure, you should discuss your medications with your doctor. You may need to temporarily stop using blood thinners or nonsteroidal anti-inflammatory drugs, as these types of medication can raise the risk of bleeding complications during the procedure.
You may need to do an enema the night before your biopsy and possibly a second enema an hour or two before the procedure.
Don’t Miss: How Do They Check Prostate
Mayo Clinic Finds What Causes Men Pain In Prostate Biopsy And Best Method To Alleviate It
- Date:
- Mayo Clinic
- Summary:
- Researchers at Mayo Clinic have evaluated the major sources of pain for some men during in-office prostate biopsy and an anesthetic method that can best lessen it. Findings were presented recently at the annual meeting of the North Central Section of the American Urological Association in San Diego. Most prostate biopsies are performed on men who have abnormal digital rectal exams or abnormally elevated prostate-specific antigen tests to evaluate the potential presence of cancer.
Researchers at Mayo Clinic have evaluated the major sources of pain for some men during in-office prostate biopsy and an anesthetic method that can best lessen it. Findings were presented recently at the annual meeting of the North Central Section of the American Urological Association in San Diego.
Most prostate biopsies are performed on men who have abnormal digital rectal exams or abnormally elevated prostate-specific antigen tests to evaluate the potential presence of cancer.
“Prostate biopsy evokes significant anxiety for some men due to anticipated pain associated with the procedure,” says Richard Ashley, M.D., Mayo Clinic urology resident and lead study investigator. “We also noted that it seemed more men had pain with their prostate biopsies than we would have liked, and we wanted to make this procedure as comfortable as possible.”
The findings in this study need to be verified by other researchers in a larger study, according to Dr. Ashley.
Story Source:
Diagnosing Prostate Cancer 2 Biopsy Types
A pathology affecting almost one in seven men worldwide, prostate cancer care relies, above all, on the early, accurate and reliable diagnosis of the disease.
The prostate biopsy therefore constitutes a critical stage in the patient journey. At present, there are two types of biopsy in practice.
The blind biopsy
The vast majority of prostate biopsies today are carried out transrectally by means of a 2D ultrasound probe. During the procedure, the doctor aims to take 12 evenly spread samples in order to maximise the chances of finding an infected site. There are two main reasons why these biopsies are referred to as blind:
- Conventional ultrasound techniques are not particularly effective when it comes to visualising potential cancer sites directly on the ultrasound scanner.
- The ultrasound guidance tool only allows for 2D visualisation, making it difficult to take an even spread of organ samples.
The development of multiparametric Magnetic Resonance Imaging of the prostate has considerably improved the sensitivity and specificity of prostate cancer diagnoses See the related studies. Given the excessive constraints associated with biopsies performed directly under MRI, an alternative has now emerged, enabling real-time integration on the ultrasound scanner of information based on MRI sequences: MRI-US fusion.
The fusion or targeted biopsy
Don’t Miss: What Are The Five Stages Of Prostate Cancer
Now We Can Ditch Useless Video Calls With Patients
It’s official: video call GP appointments are relatively useless.
That was confirmed last week in a report by researchers at the University of Oxford, which included feedback from patients, doctors and technology experts.
The study concluded that seeing patients via a video call risked missing serious diagnoses and that patients were rarely satisfied.
It’s official: video call GP appointments are relatively useless
Ive been saying for years that video consultations were mostly a waste of time especially when the former Health Secretary Matt Hancock seemed obsessed with pushing them on patients in 2020.
Patients are often surprised when I reject their request for a video call and say that Id rather speak to them on the phone instead.
Phone conversations are far more natural rubbish wi-fi signals make it hard to hear what patients say in video calls.
Thankfully, video calls arent widely used in NHS GP practices any more, the report stated, and I hope it stays that way.
Precancerous Cells And Pin
Sometimes, the results will show that precancerous cells, or prostatic intraepithelial neoplasia , are present.
If these PIN are low grade, the doctor will not consider this a matter of concern. Many males have low grade PIN. However, if the PIN are high grade, there is a chance that cancer may develop. In these cases, a doctor may suggest further tests.
If a person already has prostate cancer, the grade of the PIN does not matter, as it does not affect the severity or the Gleason score of the cancer.
Carcinoma in situ refers to cells that have the potential to become cancerous. They can occur almost anywhere in the body.
Recommended Reading: What Is Stage 3 Prostate Cancer
During The Prostate Biopsy
Depending on the type of procedure youre having, a doctor may ask you to lie on one side with your knees pulled up toward your chest or lie on your stomach. They will then apply a special gel to the area they will be examining.
In order for the doctor to obtain tissue from only suspicious parts of your prostate, imaging is necessary to help guide the biopsy needle to the right spots.
A commonly used imaging technique is the transrectal ultrasound , which involves placing a thin ultrasound probe into the rectum. TRUS uses sound waves to create images of the prostate.
Your doctor may also use magnetic resonance imaging , which involves magnetic fields and special radio waves that create detailed pictures of the prostate.
Once your doctor locates the areas to be biopsied, they will insert a core needle into your prostate to remove a small cylinder of tissue. In a typical prostate biopsy, they will remove 10 to 12 samples.
A prostate biopsy procedure usually takes around 10 minutes. Youll likely experience some soreness and discomfort for a few days afterward. During that time, you should refrain from heavy lifting and other strenuous activities.
What Does The Equipment Look Like
Ultrasound equipment:
Ultrasound scanners consist of a console containing a computer and electronics, a video display screen and a transducer or probe that is used to do the scanning. The transducer sends out inaudible high frequency sound waves into the body and then listens for the returning echoes. The principles are similar to sonar used by boats and submarines.
The ultrasound image is displayed on a video screen that looks like a computer or television monitor. The resulting image is based on the amplitude and frequency of the signal. The ultrasound image makes an image taking into account signal travel time, tissue composition, and type of body structure through which the sound travels.
The ultrasound probe used in prostate biopsies is about the size of a finger. Once the probe is placed in the rectum, the biopsy is performed with a spring-driven needle core biopsy device, or biopsy gun. The handheld device includes a long but very thin needle specially designed to open inside the prostate, take the sample and then close.
MRI equipment:
The traditional MRI unit is a large cylinder-shaped tube surrounded by a circular magnet. You will lie on a table that slides into the center of the magnet.
You May Like: Is Advanced Prostate Cancer Terminal
You May Like: How To Promote Good Prostate Health
He Felt That There Was A Lack Of Concern For Privacy And Dignity During Investigations Such As
However, a number of the men we interviewed found the biopsy painful and quite distressing. One man likened the biopsy to ‘an air gun in reverse’, and another said that the procedure ‘brought tears to your eyes’. A man who had a biopsy done in a private hospital in 1994 described the biopsy as ‘ghastly’. In 1997 he had another biopsy, this time within the National Health Service, but he found the experience equally painful, and refused to allow more than four cell samples to be taken. The use of Periprostatic nerve block with local anaesthesia before a prostate biopsy is now considered standard care, patients should not undergo the procedure without it.
Technique And Anesthetic Agents Used For The Periprostatic Nerve Block
The technique for the periprostatic nerve block is based on the original method described by Nash et al. in 1996 for basal injections. The procedure can be performed in an out-patient setting, but resuscitation facilities should be available. The same protocol used for pre-procedure preparation of TRUS-guided prostate biopsy is followed. The bladder is emptied before the procedure to prevent urinary retention .
The optimal patient position for performing the periprostatic nerve block is the left lateral decubitus position with buttocks at or slightly beyond the side of the table, the left leg in a straight position, and the right leg flexed so as to touch the abdomen. The lithotomy position is an alternative, but it is associated with more discomfort .
Optimal position of ultrasound transrectal transducer with biopsy-guide attachment for periprostatic nerve block. Tip of ultrasound transducer is pressed against prostate and anterior rectal mucosa. Transducer is manipulated to direct needle towards neurovascular bundles at base and apex of prostate and local anesthetic drug is injected around bundles.
Read Also: Why Does The Prostate Feel Good
