S8037 Cpt Code Description And Guidelines
Magnetic resonance cholangiopancreatograph is defined as follows.
Description: Magnetic Resonance Cholangiopancreatography.
The S8037 CPT code pays almost 1232.00 dollars by the insurances that cover this CPT code under their policies.
Medicare does not cover this code as of 2007. Medicare has advised us to use the abdomen MRI codes to bill this procedure.
The descriptions of the CPT codes for abdomen can be found in the section about MRI Abdomen.
These codes precisely describe the services performed. A MRCP study does include a standard MRI of the abdomen along with images to better delineate the bile duct anatomy.
How Much Does A Prostate Biopsy Cost
If you were recently screened for prostate cancer and your PSA test or digital rectal exam showed abnormal results, your doctor may recommend a prostate biopsy to investigate further.
Amino found that the median network rate for a prostate biopsy is $877. Keep in mindthis is an estimate for what you and your health insurance company might pay together for the biopsy.
Read on to learn more about what a prostate biopsy is and who might need to have one.
Diagnostic Centers Of America Is Now Rayus Radiology Florida Southeast
RAYUS Radiology now offers a network of 9 outpatient imaging centers in the Florida Southeast area. RAYUS is one of the nations leading providers of high-quality diagnostic imaging and interventional radiology services.
This relationship allows us to continue to deliver high-quality local imaging care-with the same subspecialized radiologists, staff and locations, while tapping into a broad national support.
You May Like: Is Prostate Cancer Linked To Skin Cancer
Coding Guidelines For Mri Cpt Codes
The phrase with contrast is used in the MRI CPT codes for procedures that are performed using contrast material for imaging enhancement and represents contrast material administered intravascular, intra-articularly or intrathecal route of administration.
Gadolinium is the contrast that is mostly coded for the MRI CPT codes. For intra-articular injection, use the appropriate joint injection CPT code that is present in musculoskeletal system.
Whenever radiographic arthrography is performed, also use the code for arthrography supervision and interpretation related to appropriate joint .
Use the appropriate joint injection MRI code if computed tomography or/and magnetic resonance arthrography are performed without radiographic arthrography.
Imaging can be required during the completion of certain procedures or imaging procedures may also be required during surgical procedures to evaluate the imaged area.
Many services that include image guidance are not separately reportable when it is included in the base service, that is shown in AMA CPT code section guidelines.
However, whenever a procedure or service that is marked as a separate procedure is carried out independently or distinct from any other procedures/services provided at that time, it can be reported by itself.
Some of the important key elements in the medical charts include:
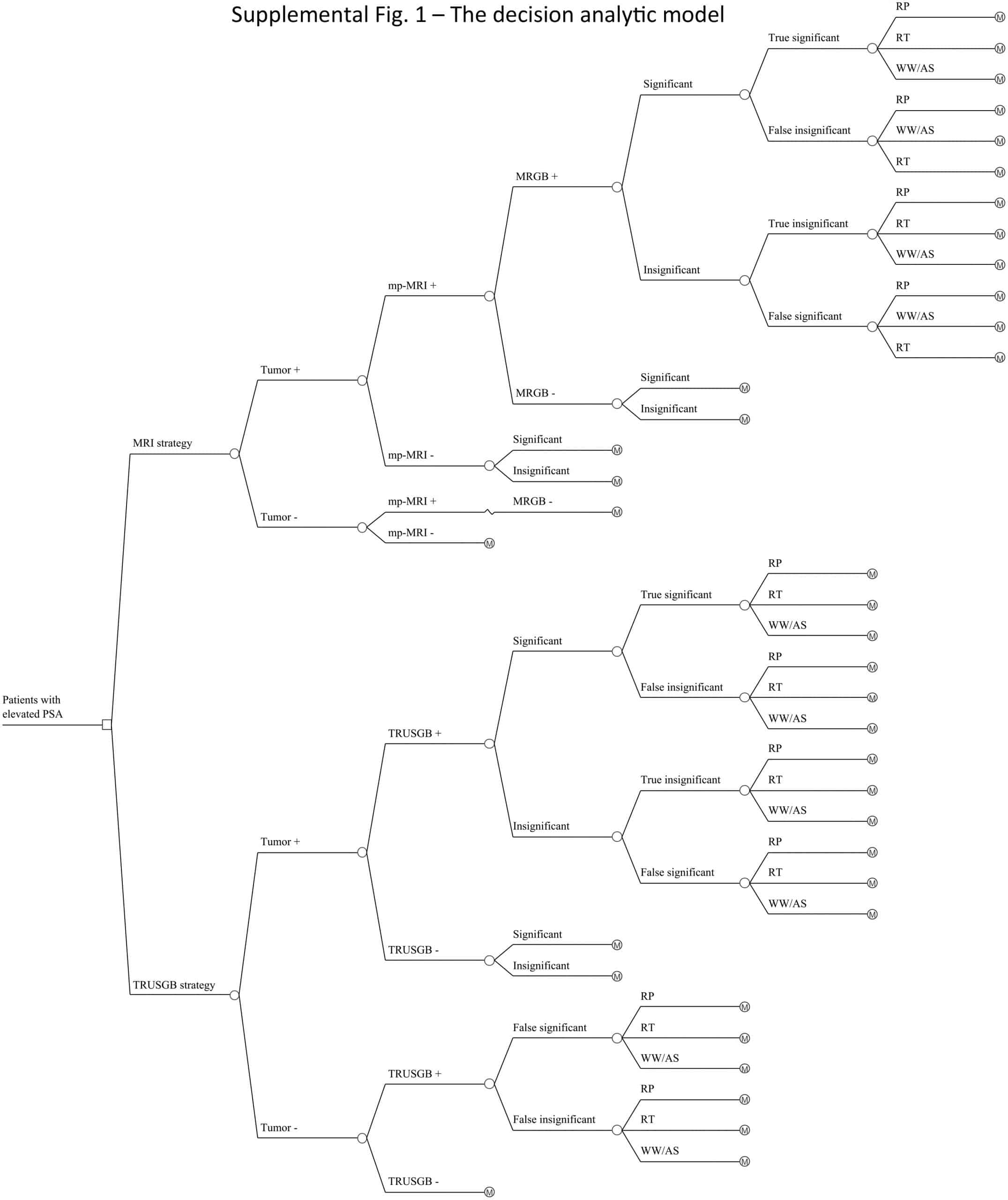
Characteristics Of Enrolled Studies
Out of the 26 enrolled studies, 25 used paired designs and 1 was a RCT. MRI-TB was used in all MRI navigation methods. Six studies included biopsy naïve patients, whereas six studies enrolled participants with prior negative biopsy results. The other studies used mixed biopsy, however, one study did not specify the biopsy type. 23 of the included studies provided clinically significant PCas definition and reported its detection rate. Some articles defined clinically significant PCa based on Gleason score 7 or > 2 positive cores. Some studies used Gleason score with other criteria based on core information . The sample size in each article ranged between 33 and 1042. Patient age ranged from 59 to 70 years. 1.5-T or 3.0-T scanner was used for mp-MRI examination in all included studies. Each patient presented with at least one disputable lesion as shown by MRI results, and each lesion was obtained from at least one targeted core. Systematic biopsies from the same session were carried out using a median of 10 – 13 cores through the transrectal route. Main features of included studies and PCa cases are presented in Table 1. The quality assessment of these enrolled studies is shown in Tables 2, 3 and Figure 2.
Table 1 Clinical characteristics of include studies.
Table 2 Quality assessment according to QUADAS-2 of the included studies.
Table 3 Quality assessment according to Cochrane Collaboration Risk of Bias Tool.
Read Also: How Can You Get Prostate Cancer
How Should I Prepare
Prior to a prostate biopsy, tell your doctor about all the medications you take, including herbal supplements. List any allergies , recent illnesses, and other medical conditions.
You may need to stop taking blood thinners for seven to 10 days before the procedure. This will help prevent excessive bleeding during and after the biopsy. The doctor may check your blood clotting on the day of the procedure. Ask your doctor and the hospital radiology clinic or department for more information.
You may need to take oral antibiotics a day before and the morning of the biopsy. This will help prevent infection.
If you are having an MRI-guided biopsy, you will need to wear metal-free clothing and remove any metallic objects, such as jewelry, watches, and hearing aids.
A technologist will walk through an MR imaging safety checklist with you. Tell your technologist about prior surgeries and metal implants, such as pacemakers, aneurysm clips, and joint replacements.
An MRI-guided procedure may use an injection of gadolinium contrast material. Because gadolinium does not contain iodine, it can be used safely in patients with contrast allergies.
Your MRI procedure may use an endorectal coil. This is a thin wire covered with a latex balloon. The doctor will lubricate this assembly and gently insert it into your rectum. Tell the doctor if you are allergic to latex so they may cover the coil with a latex-free balloon.
What Is A Prostate Biopsy
A prostate biopsy is a procedure used to test for cancer in the prostate, a small reproductive gland that helps create sperm in men.
During a prostate biopsy, a urologist will use a needle to remove several samples of tissue from your prostate. This can be done in three ways:
-
Transrectal: Your doctor will insert a needle through the wall of the rectum and into your prostate to collect small tissue samples. This is a very common method.
-
Transurethral: Your doctor will insert a thin, lighted tube through the urethra and into your prostate to collect small tissue samples.
-
Transperineal: Your doctor will insert a needle through the perineum and into your prostate to collect small tissue samples.
No matter what method you and your doctor choose, you will be offered some form of anesthesia. You may have local anesthesia, which will numb the area, or general anesthesia, which will make you unconscious for the entire procedure.
After the biopsy is done, the tissue samples will be sent to pathology to look for cancer cells. Then, your doctor may request that you schedule a follow-up visit to hear your results. Before scheduling your procedure, make sure to talk to your doctor about all your options.
Recommended Reading: Can You Get An Erection Without A Prostate
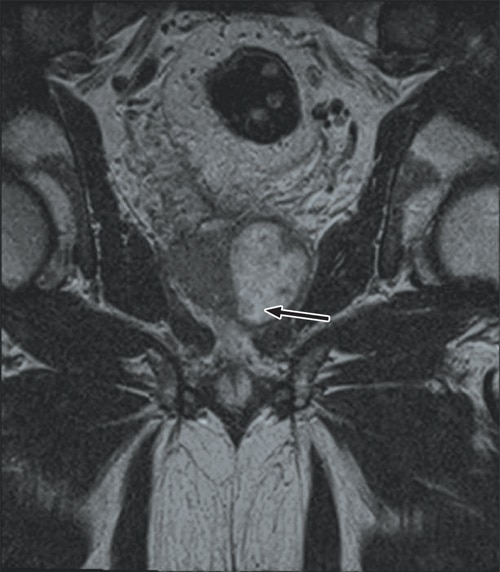
What Is An Mri Guided Prostate Biopsy
As the name implies, an MRI guided prostate biopsy is a type of biopsy in which the prostate is located through MRI technology.
MRI means Magnetic Resonance Imaging. It is more accurate than ultrasound scans, X-rays, and CT scans.
The difference is that an MRI scan uses very potent magnets to create images through radio waves. This makes a very detailed picture of the prostate gland.
Thus, the doctor can see particular areas that look suspicious and direct the biopsy needle more accurately.
But anyone who had an MRI done will know that you cant have any metal objects around during the procedure.
If thats the case, how can you perform a biopsy guided by MRI? They achieve this through a technology we call a fusion-guided biopsy.
You will go through an MRI, and then the doctor takes the image through high-tech software. They would then perform a prostate ultrasound, and the software merges the photos from the MRI and those of the ultrasound.
Thats how the doctor will see the trouble area very accurately, and the biopsy will have a more accurate result.
Cervical Spine Mri Cpt Codes
Cervical spine MRI can be billed with the following CPT codes. The 72141 CPT code can be used for cervical spine MRI without contrast material.
The 72142 CPT code can be billed for cervical spine MRI with contrast material/materials and the 72156 CPT code can be used for cervical spine MRI without contrast followed by contrast material/materials.
Read Also: Does A Nodule On The Prostate Mean Cancer
How Does The Procedure Work
Ultrasound procedure:
Ultrasound imaging uses the same principles as the sonar that bats, ships, and fishermen use. When a sound wave strikes an object, it bounces back or echoes. By measuring these echo waves, it is possible to determine how far away the object is as well as its size, shape, and consistency. This includes whether the object is solid or filled with fluid.
Doctors use ultrasound to detect changes in the appearance of organs, tissues, and vessels and to detect abnormal masses, such as tumors.
In an ultrasound exam, a transducer both sends the sound waves and records the echoing waves. When the transducer is pressed against the skin, it sends small pulses of inaudible, high-frequency sound waves into the body. As the sound waves bounce off internal organs, fluids and tissues, the sensitive receiver in the transducer records tiny changes in the sound’s pitch and direction. A computer instantly measures these signature waves and displays them as real-time pictures on a monitor. The technologist typically captures one or more frames of the moving pictures as still images. They may also save short video loops of the images.
MRI procedure:
A computer processes the signals and creates a series of images, each of which shows a thin slice of the body. The radiologist can study these images from different angles.
MRI is often able to tell the difference between diseased tissue and normal tissue better than x-ray, CT, and ultrasound.
Cost Considerations Of Mpmri As A Screening Modality For Prostate Cancer
In 2016 a pilot study using prostate MRI as a cancer screening modality was published . The cohort included 47 volunteer Canadian men without family history of prostate cancer aged 50â75. The authors utilized a 3T non-endorectal coil MRI and biopsied all patients regardless of PSA. Eighteen of 47 men were identified with prostate cancer and 3 of the 18 had tumors identified only on MRI-targeted biopsies. At all points in the receiver operating characteristic curve mpMRI was superior to PSA level for prediction of prostate cancers. The cost implications of utilizing upfront MRI as a screening modality are likely in excess of what is feasible, even in the most resource-rich healthcare environments. However, if a clinical risk stratification tool can identify a subset of patients with high likelihood of mortality from prostate cancer who are poorly predicted by PSA levels, it may be reasonable approach in these patients.
Read Also: What Is A Transrectal Ultrasound Of The Prostate
Transrectal Ultrasound Guided Systematic Biopsy
This is the most common type of prostate biopsy. You could also find it as TRUS guided prostate biopsy or TRUS biopsy.
It is the standard procedure because it is applicable for most patients. TRUS biopsies are not only performed in patients with an MRI-positive lesion.
Thus, it could be better to use this biopsy instead of an MRI-guided biopsy in some patients who never had a prostate biopsy done in the past.
This type of biopsy does not feature a high-resolution 3D picture of the prostate. Thus, it requires a higher number of samples to diagnose prostate cancer accurately.
Mri Chest And Brachial Plexus Cpt Codes
The CPT codes for Chest MRI and Brachial Plexus MRI are CPT 71550, CPT 71552.
The 71550 CPT code can be used to bill Chest MRI without the injection of contrast material.
The 71551 CPT code can be used for MRI with the injection of contrast material.
The last CPT code is 71552 and can be used to code MRI for chest and brachial plexus with and without the injection of contrast material.
Also Check: What Is The Most Common Cause Of Prostatitis
What You Need To Know About The Prostate Cpt Code For Mri Prostate
A enlarged prostate can also cause blockages in the urethra. A blocked urethra can also damage the kidneys. A patient suffering from an enlargement of the prostate may have pain in his lower abdomen and genitals. If pain is present, a digital rectal examination will reveal hard areas. A doctor may prescribe surgery or perform an endoscopic procedure. If the enlarged prostate is not completely removed, it will shrink.
While the size of an enlarged prostate will influence the extent of urinary symptoms, men may experience a range of urinary symptoms. Some men have minimal or no symptoms at all. Some men will have a very enlarged prostate, whereas others will have a mild enlargement. Generally, the symptoms can stabilize over time. Some men may have an enlarged prostate but not notice it. If they have an enlarged colon, their physician can perform a TURP procedure.
Read Also: What Is Elevated Psa Level In Prostate
What Is The Screening Controversy
The U.S. Preventive Services Task Force recently concluded that PSA-based screening results in small or no reduction in prostate cancer-specific mortality and is associated with harms related to subsequent evaluation and treatments and thus recommended limited use of the PSA test. On the other hand, the American Urologic Association recommends that screening be considered for asymptomatic men ages 55 to 69 years. Unfortunately, current diagnostic tools, including PSA screening, are unable to distinguish life-threatening prostate tumors from indolent tumors. As a result, many patients have received unnecessary, invasive prostate biopsies and aggressive therapy, which often has side effects, unnecessary cost, and emotional distress for the patient.
Don’t Miss: Where Is The Mens Prostate
> > > All Natural Technique Fixes Enlarged Prostate Watch Here< <
Surgical procedures to remove the diseased prostate are usually necessary. Surgical procedures are not always necessary. If the disease is caused by bacterial infections, a doctor can treat the symptoms using alpha-blockers or surgery. Physical therapy, relaxation exercises, and warm baths are all recommended. A physician may also prescribe antibiotics to cure the infection. A bacterial infection can also cause a recurrence of the condition.
An enlarged prostate can be uncomfortable for both men and women. Some of the symptoms of an enlarged male reproductive organ include a weakened urine stream, urgent need to urinate, and urinary tract infections. BPH can also cause damage to the kidneys. A sudden inability to urinate can be life-threatening, as it can lead to bladder and kidney damage. Unfortunately, most men with enlarged prostrates put up with the symptoms for years before they seek treatment. However, many of the men with symptoms finally decide to go to a doctor for proper gynecological evaluation and to begin enlarged prostatic therapy.
Cost Considerations Of Mpmri In Patients With A Prior Negative Biopsy
The indication for which there appears to be the best evidence for cost efficacy in prostate MRI is in the man with a negative prior ultrasound-guided prostate biopsy and continued clinical suspicion for prostate cancer . In the past clinical nomograms provided information about likelihood of repeated biopsies being positive, but did not provide guidance for localization of repeat biopsy . Similarly, additional tests and biomarkers have been shown to improve the performance of PSA in men with prior negative biopsy . Studies of MR guided biopsy in men with prior negative ultrasound biopsy have shown an increased rate of detection of high grade tumors, especially in the anterior prostate, a region often poorly sampled in ultrasound-guided biopsy . A study from 2015 showed both cost savings in using MRI to inform repeat biopsy and that a large portion of repeat biopsies could be avoided . In patients undergoing MR-guided biopsy after negative prior biopsy the possibility of avoiding systematic biopsies as a cost saving measure has been raised. This approach should be used with caution as it appears that systematic biopsies still add value and detect some clinically relevant cancers in this setting . As MRI techniques continue to refine and MRI use in prostate cancer management grows, MRI before repeat prostate biopsy is likely to become increasingly common.
Read Also: How Does A Prostate Massager Work
What Are The Limitations Of Ultrasound
A biopsy can only show if there is cancer in the tissue samples. It is possible to miss cancer in unsampled areas of the prostate.
For MRI-guided biopsies, you must remain perfectly still to ensure the technologist captures high-quality images. If you are anxious, confused, or in severe pain, it may be hard to lie still. If so, the images may not be of high enough quality to be useful.
Likewise, the presence of an implant or other metallic object sometimes makes it difficult to obtain clear MR images. A person who is very large may not fit inside certain types of MRI machines.
Bleeding may sometimes occur in the prostate after a biopsy. MR imaging cannot always tell the difference between cancer, inflammation, or the presence of blood. To avoid confusing them, your doctor may perform a repeat MRI six to eight weeks after the biopsy to allow residual bleeding to resolve.
An MRI exam typically costs more and may take more time than other imaging exams. Talk to your insurance provider if you have concerns about the cost of MRI.
How To Get The Most For Your Money
Even if your insurance does cover some or most of your prostate biopsy, youll likely pay a portion of the total cost out-of-pocket. To make sure youre getting the most care for your money:
-
Ask your insurance company about your costs, like co-insurance, copays, and deductibles.
-
Utilize your Health Savings Account , Flexible Spending Account , and Health Reimbursement Account to cover out-of-pocket expenses.
-
Use Amino to compare prices for different doctors.
-
Have a conversation with your doctor. This is especially important if you dont have insurance and are paying for the full cost of the biopsy yourself. Some doctors will offer a discount or an interest-free payment plan if they know youre shouldering the cost on your own.
Don’t Miss: Hormone Treatment For Prostate Cancer Nhs Side Effects
