What Does It Mean If In Addition To Cancer My Biopsy Report Also Mentions Acute Inflammation Or Chronic Inflammation
Inflammation of the prostate is called prostatitis. Most cases of prostatitis reported on biopsy are not caused by infection and do not need to be treated. In some cases, inflammation may increase your PSA level, but it is not linked to prostate cancer. The finding of prostatitis on a biopsy of someone with prostate cancer does not affect their prognosis or the way the cancer is treated.
Treatments May Have Side Effects
The treatment options for early-stage prostate cancer fall into three broad categories: surgery, radiation therapy, and active surveillance. Your doctor will make a treatment recommendation based on your numbers as well as a mathematical tool known as a nomogram, which can help you and your doctor better assess how extensive your cancer is likely to be and whether it is likely to become active in the future.
Yet clinical studies have not provided any evidence that one treatment is better than another or that any treatment at all actually prolongs life: The average 5-, 10-, and 15-year survival rates are virtually the same for all treatment options in early-stage prostate cancer, including active surveillance. Its also important to understand that no mathematical model is foolproof, and some men diagnosed with early-stage, locally confined disease will later find out that their cancer was more extensive than originally believed.
If you are diagnosed with early-stage prostate cancer, you have a number of treatments to choose from. A brief comparison is listed in Table 2.
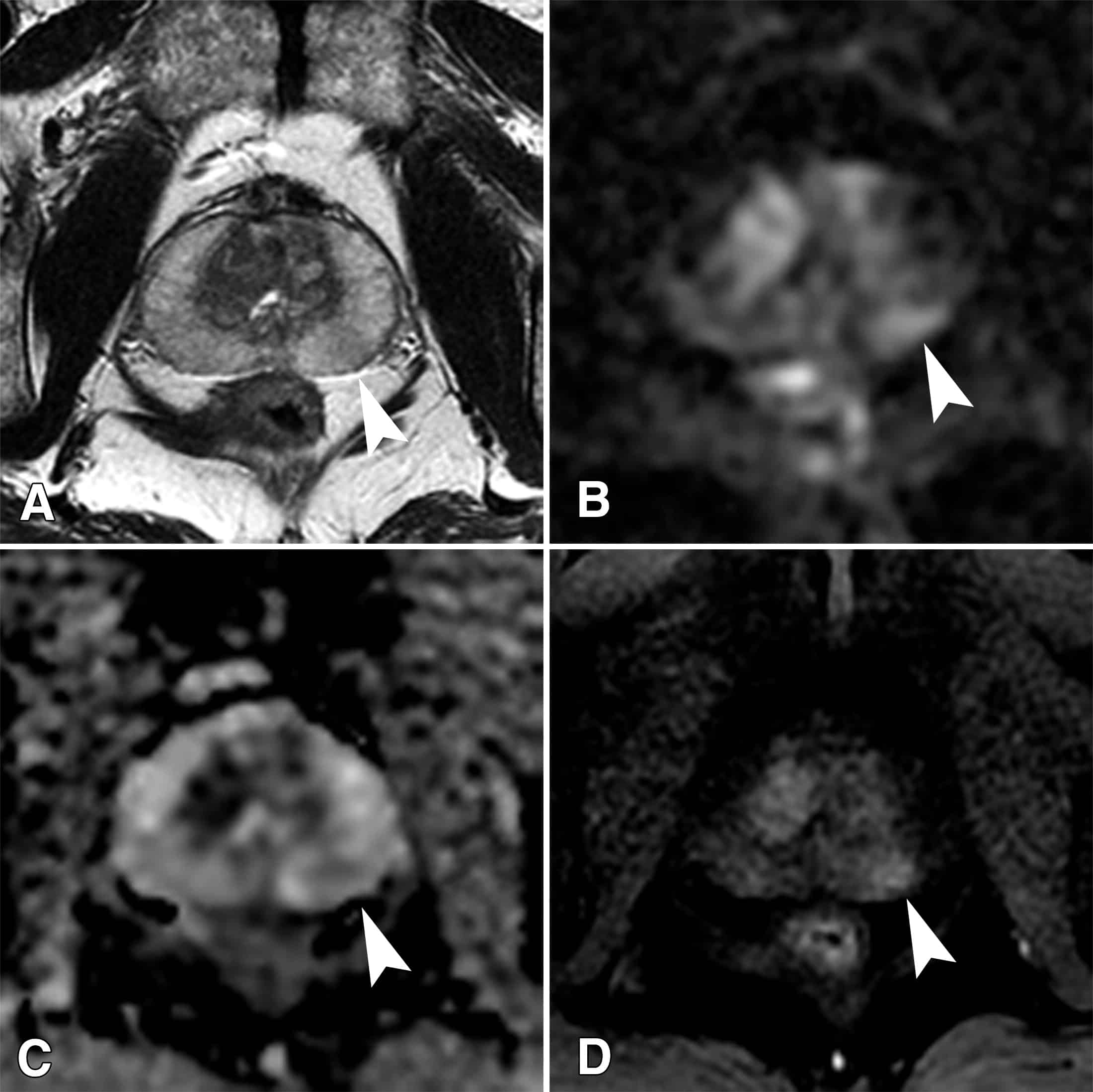
Correlation Of Percent Pattern 4 Between Needle Biopsy And Radical Prostatectomy Specimens
Correlations between Gleason scores at needle biopsy and corresponding radical prostatectomy remain a major issue, although the modified Gleason grading system has contributed to achieving better concordance. For instance, a study involving 7,643 matched biopsiesâprostatectomies published in 2012 revealed up-grading in 36.3%, 25.8%, and 30.6% of cases with biopsy Gleason scores 5â6, 3+4, and 4+3, and down-grading in 12.0% and 41.1% cases with biopsy with Gleason scores 3+4 and 4+3, respectively . To the best of our knowledge, only a few studies have assessed the concordance between the quantity of Gleason pattern 4 in prostate biopsy and prostatectomy findings.
In one study, a total of 256 biopsy cases with Gleason score 7 cancer divided into five groups, 1â20%, 21â40%, 41â60%, 61â80%, and 81â100%, according to the highest percentage of GP4 in the biopsy were correlated with histopathological findings of matched radical prostatectomy . Up-grading at prostatectomy was observed in 15.9% of biopsy Gleason score 3+4=7 cases and 11.5% of biopsy Gleason score 4+3=7 cases. Higher percentage of Gleason pattern 4 in biopsy was significantly associated with not only higher incidence of Gleason score â¥7 but also larger tumor volume and higher pathologic stage in prostatectomy specimens.
Don’t Miss: Can Keytruda Treat Prostate Cancer
What Does It Mean When There Are Different Core Samples With Different Gleason Scores
Cores may be samples from different areas of the same tumor or different tumors in the prostate. Because the grade may vary within the same tumor or between different tumors, different samples taken from your prostate may have different Gleason scores. Typically, the highest Gleason score will be the one used by your doctor for predicting your prognosis and deciding on treatment options.
What Does It Mean To Have A Gleason Score Of 6 7 8 Or 9
Because grades 1 and 2 are not often used for biopsies, the lowest Gleason score of a cancer found on a prostate biopsy is 6. These cancers may be called well differentiated or low-grade and are likely to be less aggressive that is, they tend to grow and spread slowly.
Cancers with Gleason scores of 8 to 10 may be called poorly differentiated or high-grade. These cancers are likely to grow and spread more quickly, although a cancer with a Gleason score of 9-10 is twice as likely to grow and spread quickly as a cancer with a Gleason score of 8.
Cancers with a Gleason score of 7 can either be Gleason score 3+4=7 or Gleason score 4+3=7:
- Gleason score 3+4=7 tumors still have a good prognosis , although not as good as a Gleason score 6 tumor.
- A Gleason score 4+3=7 tumor is more likely to grow and spread than a 3+4=7 tumor, yet not as likely as a Gleason score 8 tumor.
Recommended Reading: What Age To Check Prostate Cancer
What Does It Mean If In Addition To Cancer My Biopsy Report Also Says Acute Inflammation Or Chronic Inflammation
Inflammation of the prostate is called prostatitis. Most cases of prostatitis reported on a biopsy are not caused by infection and do not need to be treated. In some cases, inflammation may increase you PSA level, but it is not linked to prostate cancer. The finding of prostatitis on a biopsy of someone with cancer does not affect their prognosis or the way the cancer is treated.
What Tests Check For Prostate Cancer
Common tests to check for prostate cancer include:
- Digital rectal exam: Your doctor inserts a finger into your rectum and touches your prostate gland. The doctor feels the shape of the prostate gland and checks for any hard spots.
- PSA blood test: This blood test tells how much PSA is in your blood. Many men with prostate cancer have PSA levels that are higher than normal or that have gotten higher over time.
- A high PSA level does not always mean a man has prostate cancer. As men get older, their prostate gland may grow larger over time. This growth, and other health conditions, can cause a high PSA level in men who do not have prostate cancer.
If the test results are not normal, your doctor may recommend more tests, such as a biopsy. During a biopsy, the doctor uses a needle to take out a tiny piece or pieces of the prostate gland. An ultrasound probe may be used to guide the needle. Another doctor called a pathologist looks at the tissue under a microscope to check for cancer cells.
Note
Read Also: Can A Swollen Prostate Affect Bowel Movements
Which Prostate Cancers Really Need Treatment
July 9, 2013 by Bert Vorstman
> some 75% of all prostate cancers diagnosed are classed as favorable-risk Gleason 6 > GENERALLY, MOST of these favorable-risk Gleason 6 stage T1c prostate cancers need NO treatment whether through focal therapy or whole gland treatment> GENERALLY, MOST favorable-risk Gleason 6 cancers do NOT PROGRESS while being monitored on ACTIVE SURVEILLANCE> 25% or less of prostate cancers detected are the high-risk significant prostate cancers and it is these cancers which demand treatment> NOT ALL PROSTATE CANCERS ARE EQUAL> more people die from drug resistant infections every year than from breast cancer and prostate cancer combined> the importance of prostate cancer is greatly overemphasized> the preoccupation with PSA prostate cancer screening and detection, particularly for the insignificant Gleason 6 prostate cancer, is disingenuous
THEREFORE, on both MOLECULAR and CLINICAL fronts, it is ABUNDANTLY CLEAR thatthe Gleason 6 prostate cancer is essentially,> INSIGNIFICANT> a MISNOMER and should NOT be called a cancer> grossly MISMANAGED and MISTREATED as if a significant high-risk cancer
Which prostate cancers really need treatment?> only some 25% of prostate cancers diagnosed are classified as high-risk> significant or high-risk prostate cancers needing treatment are: * men with Gleason 4+3, 4+4 and above * men with significant volume of 4s in a Gleason 3+4
The Role Of Psa In Staging
Prostate cancer causes cells to become malignant and multiply uncontrollably. This can lead to overproduction of PSA, and higher levels of PSA in the bloodstream.
However, some men who have prostate cancer do not exhibit elevated PSA levels. And certain noncancerous conditions, like a prostate infection or benign enlargement, can also cause high PSA levels.
PSA levels are just one factor used in determining the stage of prostate cancer. Another diagnostic tool is called the Gleason scale. This rates the extent of abnormality in your prostate cells after biopsy.
At a certain point in prostate cancers late-stage progression, Gleason and PSA become less useful. When a tumor is large enough, doctors no longer need these numbers to predict its growth or malignancy.
Recommended Reading: How Do You Treat Prostate Cancer
Prostate Cancer Stages And Other Ways To Assess Risk
After a man is diagnosed with prostate cancer, doctors will try to figure out if it has spread, and if so, how far. This process is called staging. The stage of a prostate cancer describes how much cancer is in the body. It helps determine how serious the cancer is and how best to treat it. Doctors also use a cancerâs stage when talking about survival statistics.
The stage is based on tests described in Tests to Diagnose and Stage Prostate Cancer, including the blood PSA level and prostate biopsy results.
Also Check: Prostate Cancer Stage 7 Treatment
What Is The Test To See If I Have Elevated Psa
Healthcare providers use a blood test to measure PSA levels.
You may have a digital rectal exam together with a PSA test to check for signs of prostate cancer. During a DRE, your provider inserts a gloved finger into the rectum to check for bumps or other irregularities.
Depending on the results of your initial test, your provider may want you to repeat the test. PSA levels can change. A second test gives your provider more details about your prostate health.
You May Like: What Type Of Doctor Treats Prostate Issues
Percent Gleason Pattern 4 In Stratifying The Prognosis Of Patients With Intermediate
Meenal Sharma1, Hiroshi Miyamoto1,2,3
Department of Pathology and Laboratory Medicine, 2 University of Rochester Medical Center , , USA
Contributions: Conception and design: All authors Administrative support: None Provision of study material or patients: None Collection and assembly of data: All authors Data analysis and interpretation: All authors Manuscript writing: All authors Final approval of manuscript: All authors.
Correspondence to:
Abstract: The Gleason score remains the most reliable prognosticator in men with prostate cancer. One of the recent important modifications in the Gleason grading system recommended from the International Society of Urological Pathology consensus conference is recording the percentage of Gleason pattern 4 in the pathology reports of prostate needle biopsy and radical prostatectomy cases with Gleason score 7 prostatic adenocarcinoma. Limited data have indeed suggested that the percent Gleason pattern 4 contributes to stratifying the prognosis of patients who undergo radical prostatectomy. An additional obvious benefit of reporting percent pattern 4 includes providing critical information for treatment decisions. This review summarizes and discusses available studies assessing the utility of the percentage of Gleason pattern 4 in the management of prostate cancer patients.
Keywords: Gleason grading prognosis prostate biopsy radical prostatectomy
Submitted Dec 12, 2017. Accepted for publication Mar 14, 2018.
Does Percent Gleason Pattern 4 Stratify The Prognosis Of Patients Undergoing Radical Prostatectomy
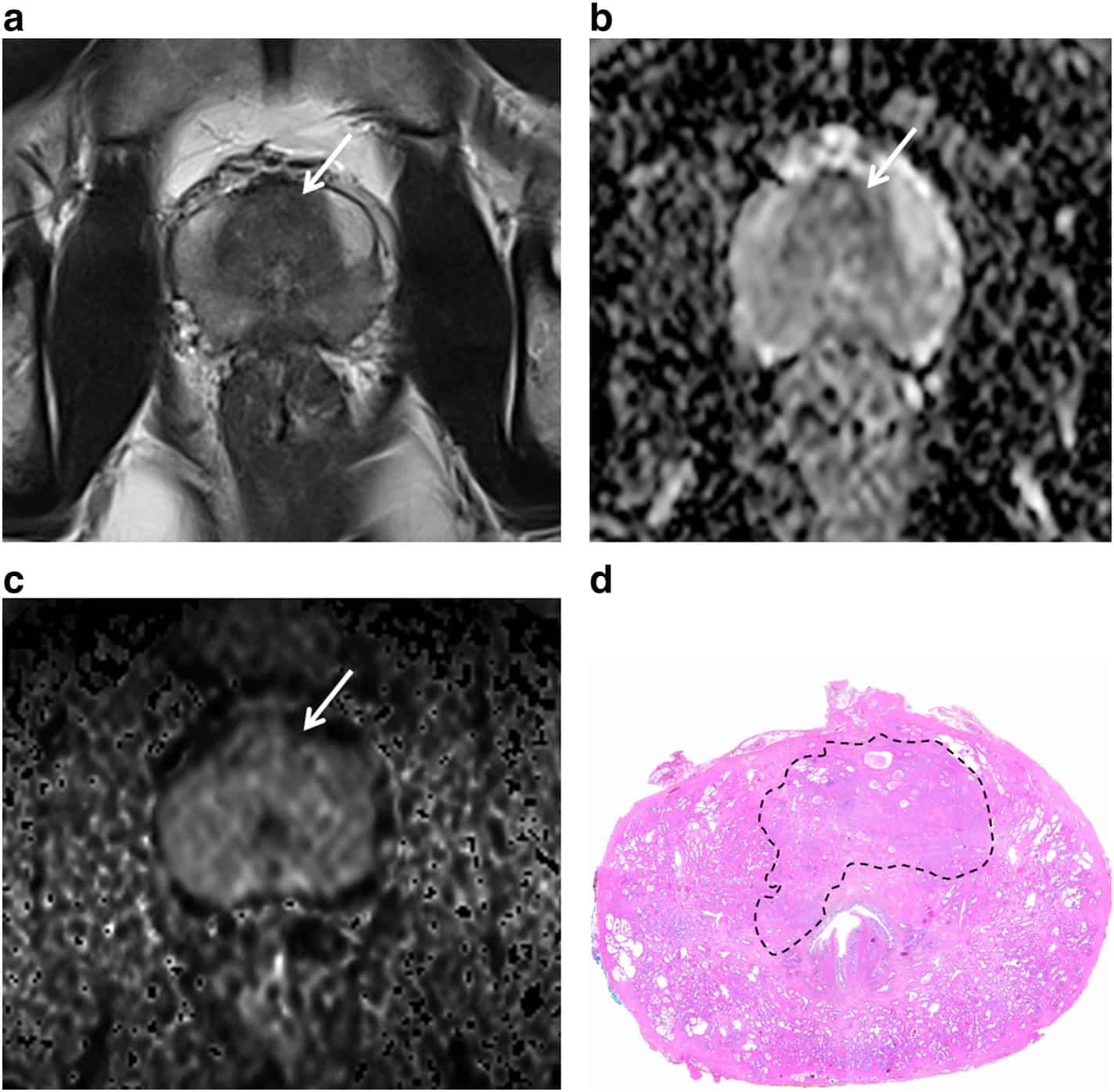
Table 1 summarizes the findings in previous studies assessing the impact of percent Gleason pattern 4 in prostate needle biopsy, radical prostatectomy, or both on stratifying patient outcomes.
Table 1
Prior to the recommendation from the ISUP 2014 consensus conference, the relative proportion of high-grade carcinoma in radical prostatectomy specimens was reported to strongly associate with established prognostic factors, such as higher preoperative prostate-specific antigen levels, positive surgical margins, extraprostatic extension, and lymph node metastasis. In a study by Cheng et al. involving 504 men who underwent radical prostatectomy for clinically localized prostate cancer, the rates of 10-year cancer-specific survival were 100%, 85%, and 67% in those with 0% Gleason pattern 4/5, 1â20% Gleason pattern 4/5, and > 20% Gleason pattern 4/5, respectively . Thus, in these 504 patients, the combined percent Gleason patterns 4 and 5 were found to be an independent predictor of cancer-specific survival.
Sauter et al. subsequently assessed a system for integration of both Gleason patterns 4 and 5 into a continuous numerical scale or score . Based on their data from 13,261 prostatectomy specimens and 3,295 matched biopsies, the IQ-Gleason score appeared to represent an efficient approach for combining quantitative Gleason grading and tertiary patterns into a single prognostic variable.
Read Also: Can You Get Prostate Cancer From Asbestos
What Are The Damico Risk Categories
The DAmico system provides an estimate of the risk of recurrence at five years after treatment. This system is one of the most widely used for risk assessment. It combines the PSA, Gleason score, and the clinical stage to create low, intermediate, and high risk categories. The higher the risk category, the higher the chance of recurrence is five years after treatment.
The DAmico risk categories are below. If one factor is putting you in a lower category but another is putting you in a higher category, then the higher category takes precedent.
Read Also: What Kind Of Doctor Checks For Prostate Cancer
What Does An Elevated Psa Level Mean If Ive Had Prostate Cancer In The Past
If youve ever had treatment for prostate cancer, youll have regular PSA screenings for the rest of your life. An increasing PSA level may mean the cancer has returned. Your care team may use other tests, including imaging scans and biopsies, to check for signs of cancer. If cancer returns, your team will discuss your treatment options with you.
You May Like: What Foods Are Good For Your Prostate
What If My Biopsy Shows Cancer
If the biopsy shows prostate cancer, your doctor will determine how likely your cancer is to grow quickly and spread. Sometimes, prostate cancer grows slowly over many years. But other times, it grows quickly.
Your doctor can use your PSA level, Gleason score, and tumor score to determine your risk level. The following pages give more information about Gleason score, T-score, and prostate cancer risk levels.
Gleason Score
The Gleason score is a common scale used to determine how fast your prostate cancer is likely to grow. Gleason scores can range from 2 to 10, but most often range from 6 to 10. The higher the Gleason score, the more likely your cancer is to grow and spread.
Tumor Score
The T-score tells how far your prostate cancer has grown.
- T1: The cancer is too small to be felt during a digital rectal exam or seen in an imaging test . The cancer is found from a biopsy done after a man has a high PSA level or has surgery for problems urinating. The cancer is only in the prostate gland.
- T2: The cancer can be felt during a digital rectal exam and may be seen in an imaging test. The cancer is still only in the prostate gland.
- T2a: The cancer is in one-fourth of the prostate gland .
- T2b: The cancer is in more than one-fourth of the prostate gland , but has not grown into the other side of the prostate gland.
- T2c: The cancer has grown into both sides of the prostate gland.
Risk Level
| Risk Level* |
|---|
Dont Miss: Msk Precise For Prostate Cancer
Grade Groups Of Prostate Cancer
The Grade Group is the most common system doctors use to grade prostate cancer. It is also known as the Gleason score.
The grade of a cancer tells you how much the cancer cells look like normal cells. This gives your doctor an idea of how the cancer might behave and what treatment you need.
To find out the Grade Group, a pathologist
Recommended Reading: How Do You Treat A Prostate Infection
Physical Emotional And Social Effects Of Cancer
Cancer and its treatment cause physical symptoms and side effects, as well as emotional, social, and financial effects. Managing all of these effects is called palliative care or supportive care. It is an important part of your care that is included along with treatments intended to slow, stop, or eliminate the cancer.
Palliative care focuses on improving how you feel during treatment by managing symptoms and supporting patients and their families with other, non-medical needs. Any person, regardless of age or type and stage of cancer, may receive this type of care. And it often works best when it is started right after a cancer diagnosis. People who receive palliative care along with treatment for the cancer often have less severe symptoms, better quality of life, and report that they are more satisfied with treatment.
Palliative treatments vary widely and often include medication, nutritional changes, relaxation techniques, emotional and spiritual support, and other therapies. You may also receive palliative treatments similar to those meant to get rid of the cancer, such as chemotherapy, surgery, or radiation therapy.
Before treatment begins, talk with your doctor about the goals of each treatment in the treatment plan. You should also talk about the possible side effects of the specific treatment plan and palliative care options.
Read Also: Stage Four Prostate Cancer Prognosis
What Does It Mean If My Biopsy Report Also Mentions Atrophy Adenosis Or Atypical Adenomatous Hyperplasia
All of these are terms for things the pathologist might see under the microscope that are benign , but that sometimes can look like cancer.
Atrophy is a term used to describe shrinkage of prostate tissue . When it affects the entire prostate gland it is called diffuse atrophy. This is most often caused by hormones or radiation therapy to the prostate. When atrophy only affects certain areas of the prostate, it is called focal atrophy. Focal atrophy can sometimes look like prostate cancer under the microscope.
Atypical adenomatous hyperplasia is another benign condition that can sometimes be seen on a prostate biopsy.
Finding any of these is not important if prostate cancer is also present.
Read Also: How Do They Take Out Your Prostate
If Treatment Does Not Work
Recovery from cancer is not always possible. If the cancer cannot be cured or controlled, the disease may be called advanced or terminal.
This diagnosis is stressful, and for many people, advanced cancer may be difficult to discuss. However, it is important to have open and honest conversations with your health care team to express your feelings, preferences, and concerns. The health care team has special skills, experience, and knowledge to support patients and their families and is there to help. Making sure a person is physically comfortable, free from pain, and emotionally supported is extremely important.
People who have advanced cancer and who are expected to live less than 6 months may want to consider hospice care. Hospice care is designed to provide the best possible quality of life for people who are near the end of life. You and your family are encouraged to talk with the health care team about hospice care options, which include hospice care at home, a special hospice center, or other health care locations. Nursing care and special equipment, including a hospital bed, can make staying at home a workable option for many families. Learn more about advanced cancer care planning.
After the death of a loved one, many people need support to help them cope with the loss. Learn more about grief and loss.
