Clinical And Histological Analysis
All prostate biopsies performed outside our institution were reviewed in accordance with our presurgical protocol.
Histology sections from prostatectomy specimens and the prostate biopsy were processed in accordance with the International Society of Urological Pathology Consensus Guidelines.
The prostatectomy specimens were sliced from apex to base at 46mm intervals in a plane perpendicular to the prostatic urethra. The distal portions of the apex and the proximal parts of the base were amputated at 4mm intervals and sliced longitudinally to assess the caudal and cranial surgical margins. After fixation in 5% buffered formalin, each block was processed and embedded in paraffin, and then 45m sections were cut with a microtome and stained with hematoxylineosin.
Tumors were classified as pECE negative if no ECE was detected, and pECE positive if pECE was detected. A pECE+ diagnosis implied the presence of a tumoral extension beyond the periphery of the prostate gland.
The clinical and laboratory data evaluated included the age of the patients, PSA levels, PSA density , and mpMRI and surgery dates. Data on the patients was anonymized and then collated in an Excel database and organized according to the surgery dates.
Prevalence Of Prostate Cancer
Prostate cancer is the second most common cancer in U.S. men and is the second leading cause of cancer death in men. One in nine men born in the U.S. today will be diagnosed with prostate cancer during his lifetime. The risk of dying from prostate cancer, however, is much lower, at one in 41. Your individual risk depends on your risk factors. Continue reading this document to better understand your particular risk.
The American Cancer Society has estimated that more than 248,000 new cases of prostate cancer will be diagnosed each year in the United States and more than 33,000 men will die from the disease. The death rate for prostate cancer is twice as high for African American men as for the general population.
Most cases are diagnosed when men are in their 60s and 70s , although prostate cancer is sometimes detected in men in their 50s or younger. The good news is that the five-year survival rate for all stages of prostate cancer has increased from 69% to almost 99% over the past 20 years. These rates vary depending on the extent of disease. Reasons for this improvement include increased public awareness, earlier detection though screening with prostate specific antigen blood tests, and advances in the treatments for this cancer.
Introduction To Clinical Context And Proposed Utility Of Modality
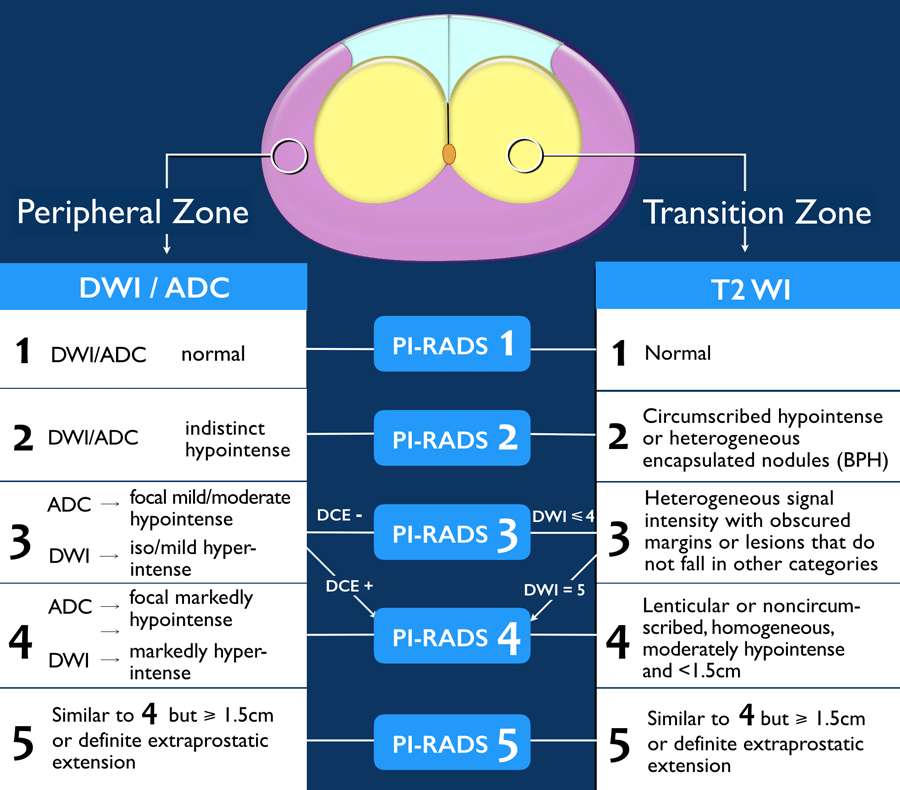
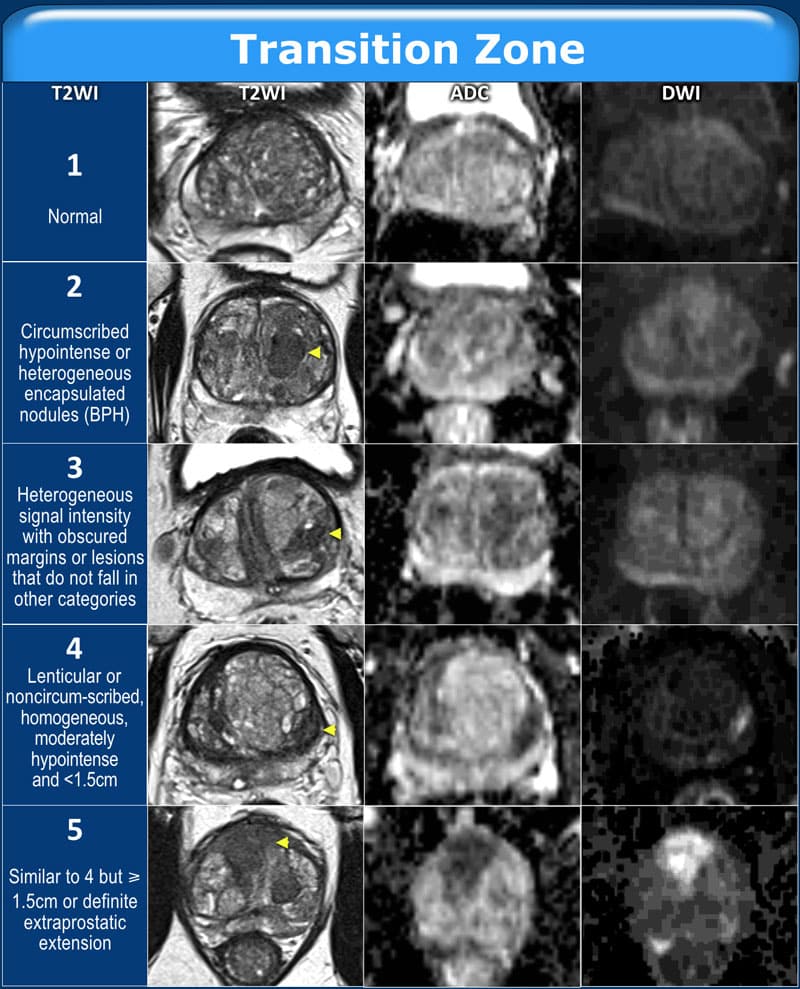
MRI became the method of choice for detection and staging of prostate cancer . Adapted from breast imaging a Prostate Imaging Reporting and Data System was published by the European Society of Urogenital Radiology : PI-RADS version 1 . This first guideline paper was based on a summary score for each lesion assessed in different sequences of mpMRI, consisting of T2w, DWI and DCE-MRI and spectroscopy facultatively. These guidelines have been updated recently by a steering committee including the American College of Radiology , ESUR and the AdMeTech Foundation to the PI-RADS v2 . In this version spectroscopy was omitted and DCE-MRI was attributed a minor role. In contrast to version 1 each lesion is attributed a single score based on findings of mpMRI. The objectives of these guidelines were to promote global standardisation of prostate imaging, to improve detection, localisation, characterisation, risk stratification of prostate cancer in treatment naïve prostate as well as to improve communication with referring urologists. The latest PI-RADS version assesses the likelihood of clinically significant prostate cancer on a 5-point scale for each lesion as follows:
-
PI-RADS 1 Very low
-
PI-RADS 2 Low
-
PI-RADS 3 Intermediate
-
PI-RADS 4 High
-
PI-RADS 5 Very high
For corresponding examples of findings see Fig. .
Fig. 1
Read Also: Does Prostate Cancer Run In Families
Side Effects Of Radical Prostatectomy
The most common side effects of the procedure are incontinence and erectile dysfunction . The incontinence, though common early after surgery, usually goes away. Whether erectile function returns depends on whether the nerves surrounding the prostate can be spared at surgery, patient age and baseline function. Men who are older or already have erection problems are most likely to have erectile dysfunction afterward.
For more information on erectile dysfunction and treatment, see Managing Erectile Dysfunction A Patient Guide.
Tests To Diagnose And Stage Prostate Cancer
Most prostate cancers are first found as a result of screening. Early prostate cancers usually dont cause symptoms, but more advanced cancers are sometimes first found because of symptoms they cause.
If prostate cancer is suspected based on results of screening tests or symptoms, tests will be needed to be sure. If youre seeing your primary care doctor, you might be referred to a urologist, a doctor who treats cancers of the genital and urinary tract, including the prostate.
The actual diagnosis of prostate cancer can only be made with a prostate biopsy .
On this page
Donât Miss: Vitamins For Prostate Health Mayo Clinic
Recommended Reading: What Happens If Your Prostate Is Removed
What Is The Prevalence Of Pi
The prevalence of prostate cancer and csPCa in published reports varies greatly . Several factors may influence the calculated prevalence, such as patient population, recruitment, definition of csPCa, and the diagnostic procedures. In MRI studies on prostate cancer, the prevalence of positive MRI varies comparably .
However, the prevalence of the maximal PI-RADS 3 score for the whole prostate is not clearly studied in the literature. For this review we initiated an explorative search to get insight into the prevalence of PI-RADS category 3 lesions. We identified relevant manuscripts published in the period 2014 to 2017. We summarized the results of each study and categorized the multiparametric MRI data into PI-RADS 12, 3, 4 and 5, and separately into a PI-RADS 45 group . In addition a sub classification was made within the patient groups of first biopsies, previously negative biopsies, and active surveillance biopsies for the PI-RADS 3 lesions.
Table 1
In men with respectively first biopsies, previously negative biopsies, and active surveillance biopsies, prostate MRIs were classified as PI-RADS 3 in 22% , 32% and 22% . In two large cohorts of men with mixed first and previously negative biopsies, the prevalence of maximal PI-RADS 3 score was 31% and 32% .
Cancer May Spread From Where It Began To Other Parts Of The Body
When cancer spreads to another part of the body, it is called metastasis. Cancer cells break away from where they began and travel through the lymph system or blood.
- Lymph system. The cancer gets into the lymph system, travels through the lymph vessels, and forms a tumor in another part of the body.
- Blood. The cancer gets into the blood, travels through the blood vessels, and forms a tumor in another part of the body.
The metastatic tumor is the same type of cancer as the primary tumor. For example, if prostate cancer spreads to the bone, the cancer cells in the bone are actually prostate cancer cells. The disease is metastatic prostate cancer, not bone cancer.
Denosumab, a monoclonal antibody, may be used to preventbone metastases.
Read Also: What To Expect After Radiation Treatment For Prostate Cancer
Prostate Cancer Risk Assessment
Prostate cancer represents a wide spectrum of disease. Some prostate cancers progress and need treatment, while others grow slowly, if at all, and can be managed conservatively with a system of careful monitoring called active surveillance. It is important to learn the characteristics of your cancer before making treatment decisions. There are many ways to determine prostate cancer risk, most of which incorporate information from several parameters, including the PSA, Gleason score and tumor extent .
Eight Types Of Standard Treatment Are Used:
Watchful waiting or active surveillance
Watchful waiting and active surveillance are treatments used for older men who do not have signs or symptoms or have other medical conditions and for men whose prostate cancer is found during a screening test.
Watchful waiting is closely monitoring a patients condition without giving any treatment until signs or symptoms appear or change. Treatment is given to relieve symptoms and improve quality of life.
Active surveillance is closely following a patient’s condition without giving any treatment unless there are changes in test results. It is used to find early signs that the condition is getting worse. In active surveillance, patients are given certain exams and tests, including digital rectal exam, PSA test, transrectal ultrasound, and transrectal needle biopsy, to check if the cancer is growing. When the cancer begins to grow, treatment is given to cure the cancer.
Other terms that are used to describe not giving treatment to cure prostate cancer right after diagnosis are observation, watch and wait, and expectant management.
Surgery
Patients in good health whose tumor is in the prostategland only may be treated with surgery to remove the tumor. The following types of surgery are used:
Don’t Miss: What Is Super Beta Prostate
Management Of Men With Pi
Posted by Samir S. Taneja, MD | Mar 2022
Samir S. Taneja, MD, presented Management of Men With PI-RADS 4-5 Lesions and Negative Biopsy during the 25th Annual Southwest Prostate Cancer Symposium conference on December 9, 2021, in Scottsdale, Arizona.
How to cite: Taneja, Samir S. Management of Men With PI-RADS 4-5 Lesions and Negative Biopsy. December 9, 2021. Accessed Dec 2022. https://grandroundsinurology.com/management-of-men-with-pi-rads-4-5-lesions-and-negative-biopsy/
What Combined Strategies In Pi
In the setting of suspicious imaging findings, it is accepted that MRI cannot negate the need for biopsy. Histopathological proof by targeted biopsies is necessary due to the high false-positive rate of MRI . If additional information can help to clarify further risk of suspicious lesions on MRI, the number of biopsies and false positive results can be reduced. Several strategies of combining additional information to MR imaging are under investigation. They may demonstrate a benefit in making a decision about which patient needs a biopsy and concurrently help avoid unnecessary biopsies. Studies on the added value in classifying further risk of PI-RADS category 3 lesions are limited.
You May Like: Is Sex Good For An Enlarged Prostate
Cancer Detection Rate Stratified By Lesion Localization
Our subgroup analysis according to lesion localization shows that estimates of cancer detection rates do not differ for PI-RADS 25 between peripheral zone and transition zone . For PI-RADS 1 , only 1 study reports lesions in the peripheral zone for this assessment category the obtained difference in cancer detection rate in PI-RADS category 1 should therefore be considered with care.
Diagnosis Of Prostate Cancer
When a digital rectal exam or a PSA test reveal abnormal results, the next step is further testing to determine whether prostate cancer is present, or another cause may be to blame.
Your doctor will evaluate your test results and any symptoms you may be experiencing and recommend the next tests you may need. The most common diagnostic tests for the prostate include:
Ultrasound: A transrectal ultrasound involves inserting a small ultrasound probe into the rectum. The ultrasound machine sends out sound waves and then measures the echoes that bounce back off body structures to create an image of the landscape of the structure. It can provide images that show the extent of prostate enlargement or abnormalities.
MRI: Magnetic resonance imaging is sometimes used to create a more detailed set of images than an ultrasound can provide. Results will be reported as a PI-RADS score.
- PI-RADS 1: very lowclinically significant cancer is highly unlikely to be present
- PI-RADS 2: lowclinically significant cancer is unlikely to be present
- PI-RADS 3: intermediatethe chance of clinically significant cancer is neutral
- PI-RADS 4: highclinically significant cancer is likely to be present
- PI-RADS 5: very highclinically significant cancer is highly likely to be present
Regardless of which procedure is used to take a sample, the prostate tissue is then examined under a microscope by a pathologist, to confirm the presence or absence of cancerous cells.
Read Also: How Do Prostate Problems Start
> > > 1 Bedtime Hack To Pee Like A Bull
An enlarged prostate can also be the cause of other problems. If the enlarged prostate is causing symptoms, the best treatment would be a natural remedy. In the meantime, there are treatments for a wide range of conditions that cause a man to experience pain. A common surgical procedure involves an electric loop, laser, or electro-stimulation. The procedure is a safe and effective option for treating enlarged or symptomatic BPH.
When Further Treatment Is Needed
While prostate cancer diagnosis and treatment have improved significantly in recent years, the cancer can still recur. That’s why it is essential that you and your doctor continue to monitor your PSA on a quarterly basis for some period of time, no matter how successful your treatment seems to be. Patients usually can consider a number of treatment options to treat or control recurrent cancer. Choosing among them requires a new decision-making process.
Don’t Miss: What To Feel For In A Prostate Exam
Where Do These Numbers Come From
The American Cancer Society relies on information from the SEER database, maintained by the National Cancer Institute , to provide survival statistics for different types of cancer.
The SEER database tracks 5-year relative survival rates for prostate cancer in the United States, based on how far the cancer has spread. The SEER database, however, does not group cancers by AJCC TNM stages . Instead it groups cancers into localized, regional, and distant stages.
- Localized: There is no sign that the cancer has spread outside the prostate.
- Regional: The cancer has spread outside the prostate to nearby structures or lymph nodes.
- Distant: The cancer has spread to parts of the body farther from the prostate, such as the lungs, liver, or bones.
Mri Interpretation And Biopsy Techniques
Multi-parametric MRI was performed prior to biopsy, with time intervals of 0 to 436 days . A single radiologist evaluated T2-weighted images, diffusion-weighted images, apparent diffusion coefficient map images, and dynamic contrast-enhanced axial MR images prior to the biopsy. Lesion were categorized as 4 or 5 based on PI-RADS v2 . After interpreting the MR images, the radiologist performed TRUS-guided biopsy. Before he began this study, he had performed TRUS-guided systematic biopsies more than 3000 times and cognitive biopsies more than 500 times according to the pre-biopsy MRI findings .
All patients had antibiotic medication prior to the biopsy procedure. The patients were placed in the left lateral decubitus and knee chest position, and a high-resolution transducer in an ultrasound scanner was introduced transrectally by a single radiologist who interpreted the pre-biopsy MRI according to PI-RADS v2. The transducer was lightly pressed against Denonvilliers fascia without compressing the prostate to detect focal lesions, which were previously categorized as PI-RADS 4 or 5 on MRI . Prostate compression was performed to reduce the tumor-to-probe distance when an anterior lesion was evaluated and biopsied .
Also Check: Can A Man Get An Erection After Prostate Surgery
Screening For Prostate Cancer
At UCSF, we believe in testing men so they know if they have prostate cancer, but that doesn’t mean every man diagnosed should have aggressive treatment. Screening is the only way to detect high-risk, potentially life-threatening prostate cancer early, while it can still be cured.
Most prostate cancers in the U.S. are identified through the following screening tests:
- Prostate-specific antigen . This simple blood test checks levels of prostate-specific antigen, a protein produced by prostate cells. The higher the PSA level, the more likely prostate cancer is present. But PSA elevations can also occur in benign conditions, most commonly benign prostatic hyperplasia, in which the prostate enlarges, as occurs in most men over their lifetime.
- Digital rectal exam . For this physical examination, your doctor inserts a lubricated gloved finger into your rectum to feel for any irregular or abnormally firm areas. While most prostate cancers are detected by PSA screening, some cancers produce little PSA but are detected by DRE.
In some circumstances, your doctor may order a repeat PSA or other tests to help determine whether a benign condition led to an elevated PSA. These tests may include:
- Multiparametric MRI
An MRI exam of the prostate is helpful and can allow for a more targeted biopsy.
Genetic And Genomic Tests For Localized Prostate Cancer
Genetic testing
A man’s inherited genes predict his prostate cancer risk. For a long time, we have known that there is a family risk in prostate cancer. If your father or brother has prostate cancer, or your mother or sister has breast or ovarian cancer, you are at higher risk of being diagnosed with prostate cancer. To partially quantify that genetic risk, a germline test can be performed before a biopsy. This test of DNA from healthy cells can determine whether you have inherited genetic mutations, such as BRCA1 and BRCA2, known to increase prostate cancer risk. If the test shows you’re low risk, you may be able to avoid a biopsy even if you have a slightly elevated PSA, while still being actively monitored for prostate cancer.
Genomic testing
If already diagnosed with prostate cancer, you may undergo another type of test for assessing your genetic risk. A genomic test of tissue from your biopsy or prostatectomy can look for somatic mutations, alterations in the DNA of the cancer cells themselves. Genomic tests measure expression of various genes that relate to how aggressive a cancer is likely to be. They indicate how rapidly cancer cells are growing and how genetically abnormal they are relative to normal cells.
Also Check: Can Prostate Cancer Spread To Lymph Nodes
New Trus Techniques And Imaging Features Of Pi
- Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, South Korea
Purpose: To determine if the new transrectal ultrasound techniques and imaging features contribute to targeting Prostate Imaging and Reporting and Data System 4 or 5.
Materials and Methods: Between December 2018 and February 2020, 115 men underwent cognitive biopsy by radiologist A, who was familiar with the new TRUS findings and biopsy techniques. During the same period, 179 men underwent magnetic resonance imagingTRUS image fusion or cognitive biopsy by radiologist B, who was unfamiliar with the new biopsy techniques. Prior to biopsy, both radiologists knew MRI findings such as the location, size, and shape of PI-RADS 4 or 5. We recorded how many target biopsies were performed without systematic biopsy and how many of these detected higher Gleason score than those detected by systematic biopsy. The numbers of biopsy cores were also obtained. Fisher Exact or MannWhitney test was used for statistical analysis.
PI-RADS 4 or 5 can be more precisely targeted if the new TRUS biopsy techniques are applied.
