Visual Registration Vs Software Assisted Registration Of Mri And Ultrasound Images
Four studies including a total of 556 patients were not able to demonstrate significant differences between the two techniques in clinically significant cancer detection, using definitions of clinically significant cancer ranging from Gleason 3+4 to maximum cancer core length of 4 mm. .
Of note, Puech et al. reported that of 95 men in the study there was a group of 68 men with 79 targets on MRI. Positivity for cancer per target was 47% for visually targeted biopsy and 53% for fusion biopsy. The Authors demonstrated no difference in cancer detection between techniques when they looked at subgroups of posterior, anterior or smallest imaging targets.
Wysock et al. prospectively reported the two targeting techniques in 125 consecutive men, with a total of 172 mpMRI-suspicious lesions that were targeted using software assisted registration. Targets were then blinded, and a second operator took two visually targeted cores and a 12-core biopsy.
Overall cancer detection rate per patient was 45 and 40 , and Gleason sum 7 cancer detection rate was 29 and 24 by fusion and visual registration, respectively . Also this study demonstrated no difference in cancer detection rate between the two techniques, but a trend toward improved cancer detection rate was observed overall and in all subsets, suggesting a need for a larger sample size.
What Are The Limitations Of Ultrasound
A biopsy can only show if there is cancer in the tissue samples. It is possible to miss cancer in unsampled areas of the prostate.
For MRI-guided biopsies, you must remain perfectly still to ensure the technologist captures high-quality images. If you are anxious, confused, or in severe pain, it may be hard to lie still. If so, the images may not be of high enough quality to be useful.
Likewise, the presence of an implant or other metallic object sometimes makes it difficult to obtain clear MR images. A person who is very large may not fit inside certain types of MRI machines.
Bleeding may sometimes occur in the prostate after a biopsy. MR imaging cannot always tell the difference between cancer, inflammation, or the presence of blood. To avoid confusing them, your doctor may perform a repeat MRI six to eight weeks after the biopsy to allow residual bleeding to resolve.
An MRI exam typically costs more and may take more time than other imaging exams. Talk to your insurance provider if you have concerns about the cost of MRI.
Considering Prostate Cancer Screening Options A Prostate Mri May Save You From An Unnecessary Biopsy
1 in 9 men will be diagnosed with prostate cancer during their lifetime. A prostate biopsy is commonly used to diagnose prostate cancer. But a non-invasive, non-surgical alternative exists: prostate MRI. Learn about the advantages of prostate MRI, which may save you from an unnecessary biopsy. And talk to your care provider about having your prostate MRI performed at UVA Medical Center.
Read Also: What Is The Male Prostate
Advanced Magnetic Resonance Mapping Targets Cancer
Using a cutting-edge technique for prostate cancer diagnosis and management, our team at University Hospitals uses MRI mapping to identify the exact location of suspicious tissue. We use images from the MRI to distinguish abnormal tissue from normal tissue. This allows our physicians to more accurately identify prostate cancer tumors and lesions, while also tracking their growth.
Although historically believed that MRI machines couldnt detect cancerous tissue, we now know that MRI images accurately identify aggressive cancers. So, with this knowledge, UH physicians developed the non-invasive fingerprinting technique to map the prostate and help distinguish normal from abnormal prostate tissue.
This breakthrough procedure lets UH physicians also monitor the prostate without making men go through unnecessary biopsies or other invasive examinations. As part of our active surveillance treatment, our team is able to monitor the growth of the tumor and determine if more interventional prostate cancer treatment is needed.
Future benefits may be even brighter: University Hospitals has been awarded a $5 million grant from the National Institutes of Health to further develop MRI mapping and the use of artificial intelligence to predict the likelihood of a cancer diagnosis.
Predictable Mri Patterns Help Identify Suspicious Lesions In The Whole Gland
Depending upon the Gleason score and prior therapies, prostate carcinoma has a certain predictable pattern on multiparametric MRI, according to Dr. Steiner. In general, lesions in the peripheral zone have decreased T2-weighted signal and are relatively focal, he says. In the transitional zone, these lesions are more difficult to evaluate on T1 and T2, but are generally non-encapsulated.
We especially look at diffusion-weighted images and the ADC map. Prostate neoplasms generally have diffusion restriction, so they are bright on diffusion-weighted imaging and dark on an ADC map, which is one of the most important characteristics of neoplasms.
The third characteristic we look at, flow, is somewhat less specific but may be quite important in deciding whether a lesion is significant or insignificant. Prostate neoplasms often have a hypervascular tumor flow pattern, meaning that there is rapid inflow of blood into the lesion and then rapid outflow due to a disrupted capillary bed. This can be graphed on multi-parametric images, allowing us to define regions of interest and look at the actual flow within these regions.
I perform this interrogation using DynaCAD prostate, which also provides an easy way to determine PI-RADS score and create the report for the urologist.
Recommended Reading: What Is The Removal Of The Prostate Called
Medical History And Physical Exam
If your doctor suspects you might have prostate cancer, you will be asked about symptoms you are having, such as any urinary or sexual problems, and how long you have had them. You might also be asked about possible risk factors, including your family history.
Your doctor will also examine you. This might include a digital rectal exam , during which the doctor inserts a gloved, lubricated finger into your rectum to feel for any bumps or hard areas on the prostate that might be cancer. If you do have cancer, the DRE can sometimes help tell if its only on one side of the prostate, if its on both sides, or if its likely to have spread beyond the prostate to nearby tissues. Your doctor may also examine other areas of your body.
After the exam, your doctor might then order some tests.
Use In Men Already Diagnosed With Prostate Cancer
The PSA test can also be useful if you have already been diagnosed with prostate cancer.
- In men just diagnosed with prostate cancer, the PSA level can be used together with physical exam results and tumor grade to help decide if other tests are needed.
- The PSA level is used to help determine the stage of your cancer. This can affect your treatment options, since some treatments are not likely to be helpful if the cancer has spread to other parts of the body.
- PSA tests are often an important part of determining how well treatment is working, as well as in watching for a possible recurrence of the cancer after treatment .
You May Like: Is Hemp Oil Good For Prostate Cancer
Is Prostate Mri With Or Without Mri
Background
Many prostate cancers are slow growing and may not have any harmful effects during a man’s lifetime. Meanwhile, clinically significant cancers can cause problems such as blockage of the urinary tract, painful bone lesions and death. The prostate-specific antigen test followed by tissue samples of the prostate with ultrasound guidance is often used to detect these cancers early. More recently, magnetic resonance imaging has also been used to help make the diagnosis.
What is the aim of this review?
The aim of this review was to compare MRI alone, MRI together with a biopsy, and a pathway that uses MRI to help decide whether to do a biopsy or not with the standard ultrasound guided biopsy in reference to template-guided biopsy.
What are the main results?
We examined evidence up to July 2018. The review included 43 studies, mainly from Western countries, of men aged 61 to 73 years.
In a population of 1000 men at risk for prostate cancer, where 300 men actually have clinically significant prostate cancer, MRI will correctly identify 273 men as having clinically significant prostate cancer but miss the remaining 27 men for the 700 men that do not have clinically significant prostate cancer, MRI will correctly identify 259 as not having prostate cancer but will misclassify 441 men as having clinically significant prostate cancer.
How reliable is the evidence?
What are the implications of this review?
The test accuracy analyses included 18 studies overall.
Moving From Trus Biopsies To Multiparametric Mri And Targeted Biopsies Guided By Fused Mri/ultrasound Images Benefits High
Radiologist Edward Steiner, MD, FACR, has collaborated with urologists to set up an alternative patient pathway for prostate carcinoma diagnosis via the use of multiparametric MRI and MRI/ultrasound fusion for targeted biopsies. Particularly when a patient with clinically significant prostate carcinoma had multiple negative TRUS biopsies before, this targeted procedure can help to quite quickly make a confident diagnosis, start therapy and potentially cure patients who have confined disease. This may be life-changing for the patient.
You May Like: Can Prostate Biopsy Cause Ed
Choosing Between A Prostate Mri Vs Biopsy
Whats worse than a false-positive PSA? A false-negative biopsy.
Research shows that 35% of biopsy results are false negatives. This means despite the invasive sampling of tissues, cancer can go undetected and continue to grow while symptoms persist.
Thats why having a prostate MRI before a biopsy is preferable. It shows the location of potential cancer, which helps direct the biopsy sampling.
Before you decide to get a prostate MRI vs. biopsy, here are a few things to know.
What Is A Prostate Biopsy
There are two main types of prostate biopsies transrectal ultrasound guided biopsies and transperineal biopsies. As the former tends to be more common, well focus on this method.
biopsies use ultrasound guidance with a biopsy tool to snip core samples from the prostate gland. An ultrasound probe and biopsy tool are introduced into the rectum where a biopsy needle penetrates the rectal wall and enters the prostate. The procedure is repeated up to 12 times.
Transrectal prostate biopsies are outpatient or in-office procedures that require only numbing medicine. Passing a needle through the rectum and into the prostate places you at risk of infection. To minimize the risk of infection, urologists commonly prescribe antibiotics beforehand.
Other complications from prostate biopsies include:
- Blood in urine, semen, and stool
Read Also: Does Prostate Milking Prevent Cancer
Open Access License / Drug Dosage / Disclaimer
This article is licensed under the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License . Usage and distribution for commercial purposes as well as any distribution of modified material requires written permission. Drug Dosage: The authors and the publisher have exerted every effort to ensure that drug selection and dosage set forth in this text are in accord with current recommendations and practice at the time of publication. However, in view of ongoing research, changes in government regulations, and the constant flow of information relating to drug therapy and drug reactions, the reader is urged to check the package insert for each drug for any changes in indications and dosage and for added warnings and precautions. This is particularly important when the recommended agent is a new and/or infrequently employed drug. Disclaimer: The statements, opinions and data contained in this publication are solely those of the individual authors and contributors and not of the publishers and the editor. The appearance of advertisements or/and product references in the publication is not a warranty, endorsement, or approval of the products or services advertised or of their effectiveness, quality or safety. The publisher and the editor disclaim responsibility for any injury to persons or property resulting from any ideas, methods, instructions or products referred to in the content or advertisements.
The Groundbreaking Technology Includes:
The PROMAP-MR combines 3D ultrasound and MRI to produce an accurate 3D mapping of biopsy samples within multimodal images.
The PROMAP-US combines full 3D ultrasound and automatic organ tracking to create, visualize and memorize a 3D map of target lesions and biopsy samples.
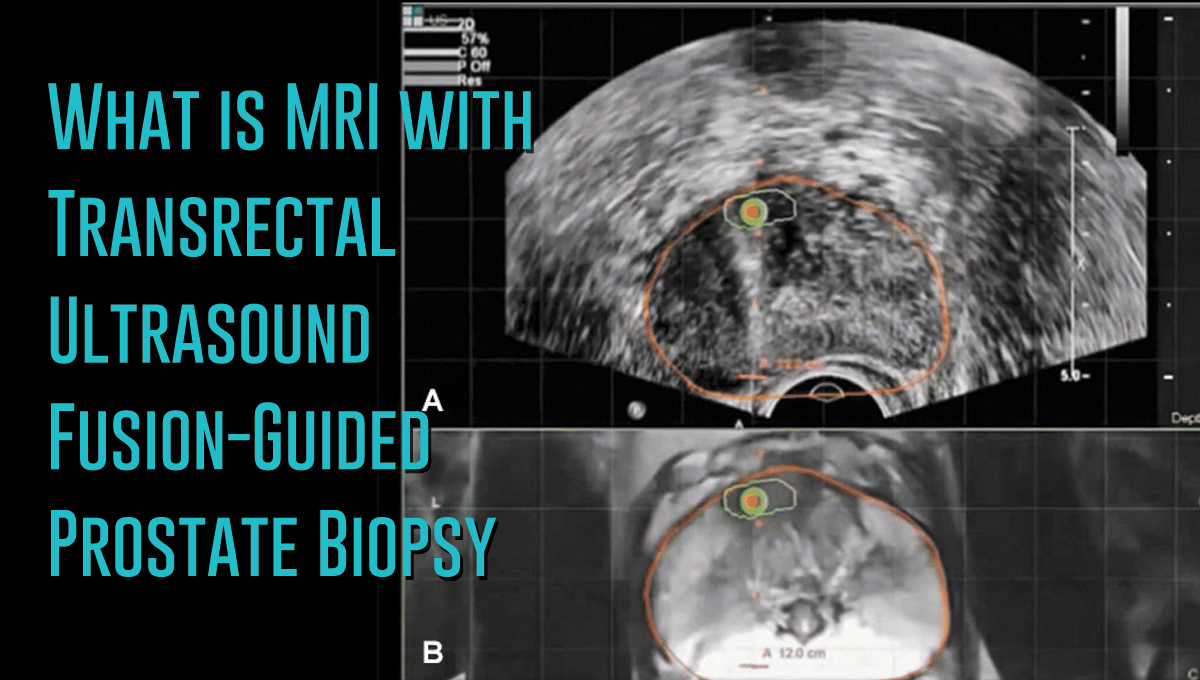
How 3D Ultrasound/MRI Fusion Biopsy Works
- Creates a 3D map of the prostate.
- Identifies suspicious lesions or targets on MRI.
- A specially trained urologist overlays 3D MRI and 3D ultrasound images in order to get a precise picture and location of suspicious areas of the prostate .
- Accurately guides the biopsy needle into the target lesion. Uniform random biopsies of other areas of the prostate may also be performed, depending upon the clinical circumstances.
- The computer creates a record of the exact location of each biopsy, which is then stored and available for future use.
Studies show that computer-assisted 3D Ultrasound/MRI Fusion Biopsy provides a more precise way to identify clinically significant prostate cancers. This allows patients access to unique technology that will significantly improve their clinical outcomes.
Who is a Candidate?
Several groups of patients can take advantage of this diagnostic tool including:
Talk to your doctor about the 3D Ultrasound/MRI Fusion Biopsy to see if you are a candidate for this advanced diagnostic procedure for prostate cancer.
Contact Us
Read Also: What Are The 5 Early Warning Signs Of Prostate Cancer
Summary Of Dr Steiners Experiences:
- High confidence in identifying and segmenting suspicious prostate lesions with multiparametric MRI
- Multiparametric MRI allows visualization of lesions in prostate areas that can hardly be seen via transrectal ultrasound
- Patients needing prostate MRI are directed to 3.0T as the high field strength benefits diagnostic confidence
- Examination time reduced from about 45 min. to about 28 min. thanks to Elition 3.0T with Compressed SENSE and excellent gradient technology
- Patient comfort features and short exam time with Elition are noticed and appreciated by patients
- DynaCAD prostate package allows fast and easy data analysis and PI-RADS score determination, as well as creating well-structured, comprehensive standardized reporting
- Easy transfer of MRI data including segmentation from DynaCAD to UroNav tool for targeted fusion biopsy
- Real-time biopsy guidance by MRI images fused to ultrasound by UroNav probe handling quite similar to TRUS biopsy
- Impressive results seen with MRI/ultrasound fusion biopsies in patients with clinically significant prostate carcinoma that experienced multiple negative TRUS biopsies before
- Entire procedure is reimbursed and the biopsy setup allowed to quickly break even regarding costs
Transrectal Ultrasound Guided Systematic Biopsy
This is the most common type of prostate biopsy. You could also find it as TRUS guided prostate biopsy or TRUS biopsy.
It is the standard procedure because it is applicable for most patients. TRUS biopsies are not only performed in patients with an MRI-positive lesion.
Thus, it could be better to use this biopsy instead of an MRI-guided biopsy in some patients who never had a prostate biopsy done in the past.
This type of biopsy does not feature a high-resolution 3D picture of the prostate. Thus, it requires a higher number of samples to diagnose prostate cancer accurately.
Don’t Miss: If Prostate Is Removed Are You Impotent
% Less Detection Of Insignificant Cancer 3 Times Less Biopsy Core: Less Complication And Side Effects Mri/us Fusion Cancer Detection Rate
PRECISION study : MRI-Targeted or standard Biopsy for Prostate-Cancer Diagnosis
V.Kasivisvanathanet al. May 2018
- In cases of negative results, the hypothesis of cancer cannot be ruled out.
- In cases of low-positive results, suspicion of more aggressive cancer may remain.
Conventional Biopsy : Possible results
25% of cases Biopsy misses the tumor
Fortuitous reaching of non significant cancer
Underestimation of tumors size
Delaying the diagnosis, under- or overestimating the aggressiveness of the disease and, ultimately, failing to provide the best possible care for the patient.
However, the evolution of medical imaging techniques together with advances in fusion technologies have changed the landscape where practices are concerned.
In technical terms, targeted biopsies are made possible by the fusion of ultrasound images of the prostate with MRI scans or PET sequences, in real time during the procedures.
Recommended Reading: How Is Prostate Test Done
Studies Comparing Multiple Mri
Eleven studies were identified which compared two different MRI-targeting techniques. One study was a simulation study, and two studies selected men for one technique or another in a non-randomised fashion, and are described below. The eight remaining studies are summarized in Table 1 and Table S1. Only two studies investigated a totally biopsy-naïve cohort of men . All mpMRI scans were performed on either a 1.5T or 3T scanner and had T2-weighted scans, DWI and DCE. In the study by Lee et al. 12% of men did not have a DCE study. Standard TRUS biopsy was used as an additional comparator in 6 studies.
Table 1
Two studies compared biopsy techniques across different men biopsied at different time periods in the same institution, rather than comparing techniques in the same men, or randomizing men to one approach or another. With a sequential design, it is possible that the selection criteria for men having an MRI or biopsy may differ between groups, or that there may be a learning curve effect both in terms of MRI and biopsy, over time.
You May Like: How Many Stages Of Cancer Are There In Prostate Cancer
What Happens After An Mri
You may resume your normal activities and diet immediately. You may be sore for a few days, and you also may see small amounts of blood in your urine, stool, and semen. However, these symptoms usually last only a few days. A high fever or flu-like symptoms within a few days of the biopsy should cause you to seek attention in a local emergency room to get treated for an infection.
Last reviewed by a Cleveland Clinic medical professional on 11/03/2016.
References
Study Method And Population
From July 2015 to April 2018, a series of 142 consecutive patients undergoing MRI-GB were prospectively enrolled. Indications for MRI-GB included patients with an elevated prostate-specific antigen serum level and/or abnormal digital rectal examination findings and 1 suspicious area on the mpMRI scan. We included both patient biopsy naïve and patient with previous TRUS-GB. According to the European Society of Urogenital Radiology guidelines, the presence of clinically significant PCa on mpMRI is defined as equivocal, likely, or highly likely according to a PI-RADS v2, score of 3, 4, or 5, respectively . The local institutional review board approved the present study.
You May Like: Can You Remove Prostate After Radiation
