Optimising Mri Volume Measurements
Optimal Method of Measurement
The PI-RADS v2.1 guidelines provide the minimal requirements for measurement of volume which are to report a single measurement of a suspicious lesion on an axial image unless it is not clearly delineated, in which case the measurement should be on the image which best depicts the finding . If the largest dimension of the lesion is on sagittal or coronal images, this measurement should also be reported.
The maximal diameter is a simple measurement which is feasible to obtain in clinical practice. It has been used as an inexpensive surrogate for tumour volume in radical prostatectomy specimens following studies comparing different methods for tumour size estimation . The role of maximum diameter for mp-MRI-derived volume estimation is less well-established. Nakashima et al. found that the maximal tumour diameters on MRI and radical prostatectomy specimens should be limited to tumours larger than 1.0;cm in diameter.
Alternative methods include three-dimensional quantification based on an ellipsoid formula or plainmetry. Planimetric volume measurement is presumed to be the most accurate technique and the majority of studies evaluating mp-MRI-derived tumour volumes adopt this approach. Plainmetry requires contouring of the lesion on each axial slice and places a significant additional time burden on the reporting radiologist.
Optimal mp-MRI Sequence
Fig. 1
Other Factors
Enhancing Healthcare Team Outcomes
Prostate cancer diagnosis and treatment can be complex and is often controversial. an interprofessional;team of specialty-trained nurses, nurse practitioners, physician assistants, primary care providers, and urologists must work to manage:
These and many more issues continue to challenge clinicians who deal with;prostate cancer patients and men at risk for this common, potentially lethal male malignancy.
The interprofessional team can optimize the treatment of these patients through communication and coordination of care. Primary care providers, urologists, oncologists, radiation oncologists, and nurse practitioners provide diagnoses and care plans. Specialty care urologic nurses should work with the team for coordination of care and are involved in patient education and monitor compliance. The interprofessional team can thus improve outcomes for patients with prostate cancer.
If You Dont Have Treatment Straight Away
Your doctors monitor your cancer closely if it is unlikely to grow or develop for many years. If it starts to grow, you have treatment. This is called active surveillance. You have active surveillance if you have either:
- low risk localised prostate cancer and surgery or radiotherapy are suitable treatments for you
- intermediate risk localised prostate cancer if you dont want treatment straight away
Another way to monitor prostate cancer is called watchful waiting. You have fewer tests than with active surveillance. You have watchful waiting if the doctor aims to control your cancer and:
- you don’t have any prostate cancer symptoms and you’re not suitable for treatments that aim to cure, such as radiotherapy or surgery
- you dont want active surveillance
You might also have cryotherapy or high frequency ultrasound therapy as part of a clinical trial.;
Radiotherapy and surgery work equally well at curing prostate cancer but they have different side effects. Your doctor can explain these to you.
Recommended Reading: Does An Enlarged Prostate Affect A Man Sexually
Optimising Focal Therapy Treatment Margins
To compensate for the underestimation of mp-MRI tumour volumes, there have been attempts to estimate an appropriate treatment margin to ensure full coverage of the index lesion. The 2015 Focal Therapy Consensus meeting recommended a circumferential margin of 5;mm around a lesion accounting for a 23;mm known registration error and the underestimation by mp-MRI .
The principle of an adequate surgical margin surrounding a tumour is standard for all organ-conserving surgery. There has been extensive research into the appropriate margins for operations such as partial nephrectomy, partial penectomy and partial ureterectomy. For focal therapy, there are challenges to overcome due to the absence of a post-operative specimen to evaluate margin status. This has presented challenges for research into margin status and studies rely on extrapolation from radical prostatectomy specimens which have an inherent selection bias as well as the problems of accurate co-registration between histology and MRI.
This variation highlights the need for individualised treatment margins which are determined based on the appropriate therapeutic risk-benefit ratio for each patient. The optimal margin is influenced by multiple patient-specific and operative factors. Tumour volume is an important component for the surgeon to consider along with other interrelated variables such as index lesion location, histological characteristics and energy modality.
How Do The Treatment Options Compare
A study known as the ProtecT trial is the most important study on treatments for low-risk prostate cancer so far. ProtecT stands for prostate testing for cancer and treatment. This trial compared three treatment options: active surveillance, external radiotherapy and surgery to remove the prostate. A total of 1,643 men between the ages of 50 and 69 took part in the trial. They all agreed to be randomly assigned to one of the three treatment groups. About two thirds of them had low-risk prostate cancer. The treatment outcomes were recorded over an average of ten years, and then compared with each other at the end of the trial.
The following was found over a period of ten years:
- no difference in mortality rate between the active surveillance, radiotherapy and surgical removal groups,
- a somewhat higher risk of metastases in the active surveillance group,
- a much higher risk of accidental urine leakage in men who had surgery,
- a much higher risk of erection problems in men who had radiotherapy or surgery .
- a somewhat higher risk of accidental stool leakage in men who had radiotherapy.
Based on the results of this trial and other research, we have developed a decision aid that can help men who have low-risk prostate cancer to weigh the pros and cons of the various treatment options for example, together with their friends, family and doctors.
You May Like: What Is Perineural Invasion In Prostate Cancer
Gleason Score For Grading Prostate Cancer
Prostate cancer is also given a grade called a Gleason score. This score is based on how much the cancer looks like healthy tissue when viewed under a microscope. Less aggressive tumors generally look more like healthy tissue. Tumors that are more aggressive are likely to grow and spread to other parts of the body. They look less like healthy tissue.
The Gleason scoring system is the most common prostate cancer grading system used. The pathologist looks at how the cancer cells are arranged in the prostate and assigns a score on a scale of 3 to 5 from 2 different locations. Cancer cells that look similar to healthy cells receive a low score. Cancer cells that look less like healthy cells or look more aggressive receive a higher score. To assign the numbers, the pathologist determines the main pattern of cell growth, which is the area where the cancer is most obvious, and then looks for another area of growth. The doctor then gives each area a score from 3 to 5. The scores are added together to come up with an overall score between 6 and 10.
Gleason scores of 5 or lower are not used. The lowest Gleason score is 6, which is a low-grade cancer. A Gleason score of 7 is a medium-grade cancer, and a score of 8, 9, or 10 is a high-grade cancer. A lower-grade cancer grows more slowly and is less likely to spread than a high-grade cancer.
Gleason Prostate Cancer Score
1960s as a way to measure how aggressive your prostate cancer may be.
A pathologist determines your Gleason score by looking at a biopsy of your prostate tissue under a microscope. They grade the cells in the biopsy on a scale of 1 to 5. Grade 1 cells are healthy prostate, whereas grade 5 cells are highly mutated and dont resemble healthy cells at all.
The pathologist will calculate your Gleason score by adding together the number of the most prevalent type of cell in the sample and the second most prevalent type of cell.
For example, if the most common cell grade in your sample is 4 and the second most common is 4, you would have a score of 8.
A Gleason score of 6 is considered low-grade cancer, 7 is intermediate, and 8 to 10 is high-grade cancer.
Recommended Reading: Does Enlarged Prostate Cause Constipation
Justification For A New Guideline
Clinicians treating men with advanced prostate cancer are challenged with the rapidly evolving prostate cancer landscape given the approval of new classes of agents for use in various prostate cancer disease states. The increasing complexity of advanced prostate cancer management underscores the need for the current clinical practice guideline, developed to provide a rational basis for treatment of patients with advanced disease, based on currently available published data. To assist in clinical decision-making, guideline recommendations are furnished according to disease state across the entire continuum of advanced prostate cancer.
Questions To Ask Your Doctor Or Nurse
- What is my Gleason score?
- What is the stage of my cancer?
- What treatments are suitable for me?
- Could my cancer be monitored instead?
- How quickly do I need to make a decision?
- What are the advantages and disadvantages of each treatment?
- What are the side effects?
- How effective is my treatment likely to be?
- What is the risk of my cancer coming back after treatment?
- Can I see the results of treatments youve carried out?
- Can I get copies of all my test results and letters about my treatment?
- Are all of the treatments available at my local hospital?
- If not, how could I have them?
- Can I join any clinical trials?
- If I have any questions or get any new symptoms, who should I contact?
Don’t Miss: What Happens To The Prostate Later In Life
Active Surveillance May Help Your Quality Of Life
With this approach, you have regular checkups, including a PSA test and rectal exam. Youll get a prostate biopsy if needed. You can start treatment at any time if the cancer starts to grow.
Active surveillance is a good choice for many men with low-risk prostate cancer, because they can avoid the side effects of treatment. This is an especially important choice if you are older or in poor health.
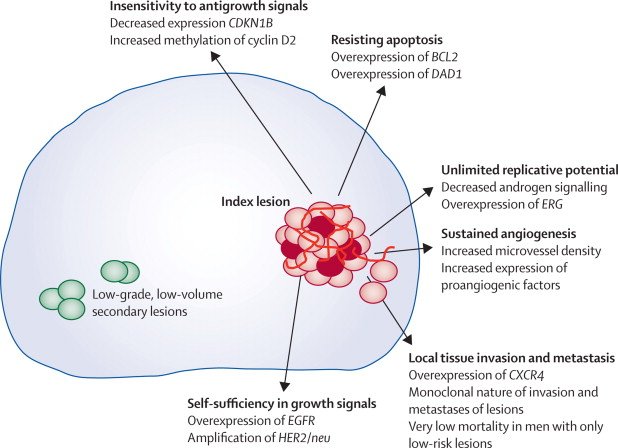
The Natural History And Molecular Biology Of Low Grade Prostate Cancer
Prostate cancer develops with age in the majority of men, including those from all races and regions. In Caucasians, the chance of harboring prostate cancer is approximately the same as ones age; thirty percent of men in their 30s, 40% in their 40s, 80% in their 80s . Most of these are microfoci and low grade, particularly in younger men. The high prevalence of microfocal prostate cancer has been confirmed in autopsy studies of Caucasians, Asians, and other ethnic groups going back more than 50 years. A recent autopsy study in Japanese and Russian men who died of other causes showed that overall 35% of both groups had prostate cancer, and 50% of the cancers in Japanese men aged >70 were Gleason score 7 or above .
You May Like: Is Turmeric Good For Prostate
Monitoring And Treatment Decisions
In the past, men with prostate cancerregardless of whether it was aggressive or notwere almost always treated right away with a targeted therapy like surgery or radiation. However, in recent years, experts have revisited this one-size-fits-all approach to prostate cancer.
Experts now understand that low-risk prostate cancerlike Gleason 6 tumorsmay not need treatment right away. In fact, major medical associations, including the American Urological Association and the Society for Urologic Oncology, now recommend the use of active surveillance for low-risk prostate cancer.
What Does It Mean If My Biopsy Mentions That There Is Perineural Invasion
Perineural invasion means that cancer cells were seen surrounding or tracking along a nerve fiber within the prostate. When this is found on a biopsy, it means that there is a higher chance that the cancer has spread outside the prostate. Still, perineural invasion doesnt mean that the cancer has spread, and other factors, such as the Gleason score and amount of cancer in the cores, are more important. In some cases, finding perineural invasion may affect treatment, so if your report mentions perineural invasion, you should discuss it with your doctor.
Recommended Reading: Would You Expect A Male With Benign Prostatic Hyperplasia To Have Difficulty With Ejaculation
Risk Stratification: Clinically Insignificant Disease
The evidence for which men will benefit from active treatment of prostate cancer is evolving. It has been argued that low-grade and low-volume lesions do not have the typical hallmarks of cancer, certainly do not behave aggressively and may be regarded as clinically insignificant . The ProtecT trial, which randomised men to active monitoring, surgery or radiotherapy in men diagnosed via PSA screening found no difference in prostate cancer-specific mortality at a median follow-up of 10;years . The PIVOT and SPCG-4 RCTs show that the benefit of treatment resided in the high-risk group and possibly in intermediate-risk men too . There is a clear need for improved methods of risk stratifying men so that treatment can be directed towards those who are more likely to derive a cancer-specific mortality benefit.
The most widely used definition of clinically insignificant disease is based on the histopathological parameters set out by Stamey and Epstein . Insignificant prostate cancer is defined on whole-mount prostatectomy as a tumour volume ranging from 0.2 to 0.5;cm3, no Gleason patterns 4 or 5 and organ confined. The original paper by Stamey et al. described a single parameter of tumour volume 0.5;cm3 from a cystoprostatectomy series based on an 8% lifetime risk of being diagnosed with clinically significant cancer. Epstein et al. reported a volume threshold <0.2;cm3 as being insignificant if the criteria of no capsular penetration were applied.
What Is My Outlook
Many men will want to know how successful their treatment is likely to be. This is sometimes called your outlook or prognosis. No one can tell you exactly what will happen, as it will depend on many things, such as the stage of your prostate cancer and how quickly it might grow, your age, and any other health problems. Speak to your doctor about your own situation.
Most localised prostate cancer is slow-growing and may not need treatment or shorten a mans life. For many men who have treatment for localised prostate cancer, the treatment will get rid of the cancer. For some men, treatment may be less successful and the cancer may come back. If this happens, you might need further treatment.
For more information about the outlook for men with prostate cancer, visit;Cancer Research UK. The figures they provide are a general guide and they cannot tell you exactly what will happen to you. Speak to your doctor or nurse about your own situation.
Don’t Miss: Prostate Cancer Shortness Of Breath
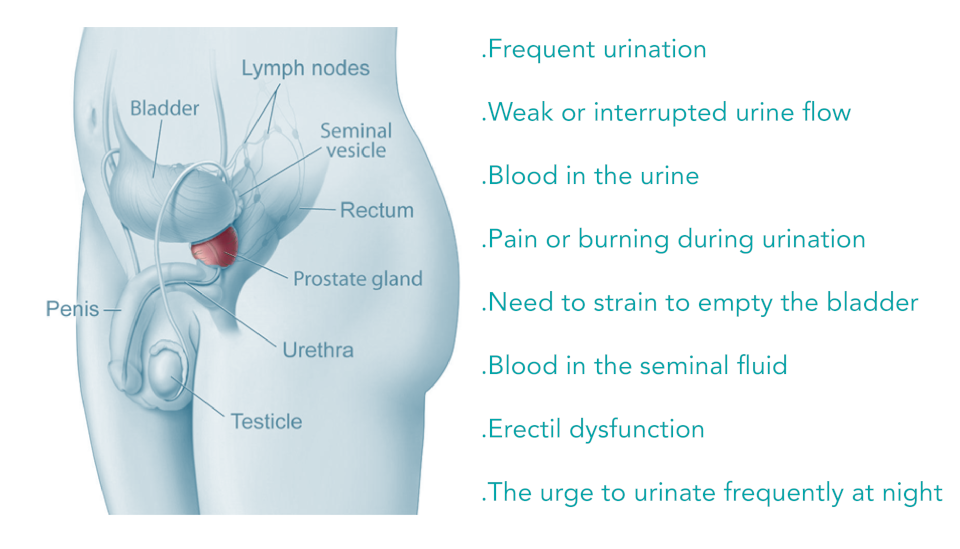
How Is Prostate Cancer Diagnosed
If you have symptoms of prostate cancer, your provider will perform a digital rectal exam and a PSA blood test. If either of those two tests are abnormal, then most likely your provider will recommend that you have a prostate biopsy. A biopsy is the only way to know for sure if you have cancer, as it allows your providers to get cells that can be examined under a microscope.;
The most common way that a biopsy is done is with a trans-rectal ultrasound . A trans-rectal ultrasound is a thin cylinder that puts out sound waves and monitors them when they bounce off of tissue. It is inserted into your rectum, and allows the provider performing the biopsy to view your prostate and choose where to remove the tissue for further evaluation. Any suspicious areas are biopsied. In addition, some tissue will be removed from all of the different parts of the prostate . The procedure is done while you are awake, with the help of some numbing medicine. Unfortunately, a trans-rectal ultrasound isn’t a perfect tool. Even though many samples are taken, it can occasionally miss the area of the cancer. If this happens, and your PSA remains elevated, you may need to have the procedure repeated.
Your provider may order other tests including a;bone scan, CT scan or MRI to see if the cancer has spread to the bones, lymph nodes or other organs.;
What Screening Tests Are Used For Prostate Cancer
There are two tests used for prostate cancer screening:
The American Cancer Society recommends that men make an informed decision on whether or not they should be screened after talking about the risks and benefits of screening with their healthcare provider. Screening is not recommended in men without symptoms of prostate cancer if they have a life expectancy of less than ten years. Men at average risk of developing prostate cancer should begin this conversation at age 50. African American men and men with one relative with prostate cancer should talk with their healthcare provider about screening beginning at age 45. Men at the highest risk, those with more than one first degree relative with prostate cancer at an early age should begin talking about screening at age 40. Repeat screening is based on baseline PSA results, but typically occurs every 1-2 years.
You May Like: Does An Enlarged Prostate Affect A Man Sexually
How Important Is The Gleason Score
The Gleason score is very important in predicting the behavior of a prostate cancer and determining the best treatment options. Still, other factors are also important, such as:
- The blood PSA level
- How much of each core is made up of cancer
- The number of cores that contain cancer
- Whether cancer was found in both sides of the prostate
- Whether the cancer has spread outside the prostate
Relative Survival Stages At The Time Of Diagnosis
According to latest statistics, more than 2,795,592 men are currently living in United States with prostate cancer; yet estimated number of deaths due to prostate cancer in the year 2015 is 27,540 .
- Local stage
The local stage indicates that the cancer has not progressed to any area outside of the prostate gland; the survival rate in local stage is approximately 100 percent. Most of the cases are diagnosed in this stage.
- Regional stage
In this type, the cancer advances to the surrounding tissues around the prostate gland. The survival rate is approximately 100 percent if treatment is sought early.
- Distant stage
This is the most advanced stage of prostate malignancy in which the cancer cells invade lymph nodes and distant organs . The survival rate is 28 percent.
Read Also: Is Viagra Good For Enlarged Prostate
